7 Hand fractures and joint injuries
Synopsis
 Diagnosis of hand fractures and joint injuries requires history, examination, and adequate imaging studies.
Diagnosis of hand fractures and joint injuries requires history, examination, and adequate imaging studies.
 Treatment decisions are based on fracture geometry, stability, and individual patient needs.
Treatment decisions are based on fracture geometry, stability, and individual patient needs.
 Nonoperative principles include reduction, maintenance of reduction through casting or splinting, followed by protected motion.
Nonoperative principles include reduction, maintenance of reduction through casting or splinting, followed by protected motion.
 Operative treatment includes closed reduction with or without percutaneous pinning, external fixation, and open reduction and internal fixation.
Operative treatment includes closed reduction with or without percutaneous pinning, external fixation, and open reduction and internal fixation.
 Rehabilitation is an important aspect of caring for patients with hand fractures and joint injuries and involves splinting and restoring motion.
Rehabilitation is an important aspect of caring for patients with hand fractures and joint injuries and involves splinting and restoring motion.
 Secondary procedures may be considered when the desired outcome is not achieved. These include correction of malunion, tenolysis, and capsulotomy.
Secondary procedures may be considered when the desired outcome is not achieved. These include correction of malunion, tenolysis, and capsulotomy.
Introduction
Fractures of the phalanges and metacarpals are the most common fractures in the upper extremity and have been reported to account for 10% of all fractures.1 Appropriate diagnosis and treatment can minimize deformity and maximize function. Although many of these fractures can be managed nonoperatively, appropriate follow-up is crucial for a good outcome. These injuries can result in time away from work and activities and can be complicated by stiffness and weakness. The goal of the treating physician should be to minimize deformity and maximize function. Operative indications depend on multiple factors, including stability, location, geometry, configuration, and associated injuries, but ultimately, is chosen when the anticipated outcome is better than nonoperative management.2
Classification of fractures and dislocations
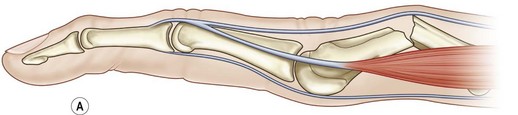
The angular deformity of the fracture is dependent upon the forces acting on the distal bones. Metacarpal fractures most commonly have an apex dorsal configuration secondary to the pull of the interosseous muscles, while fractures of the proximal phalanx tend to have apex volar configuration due to the interosseous muscles. Fractures of the middle phalanx have a variable deformity, depending of the location of the fracture. Those proximal to the insertion of the FDS have dorsal angulation due to flexion of the distal portion of the bone from the FDS, while fractures distal to the FDS insertion have apex volar angulation due to flexion of the proximal fragment (Fig. 7.1).
Pediatric fractures
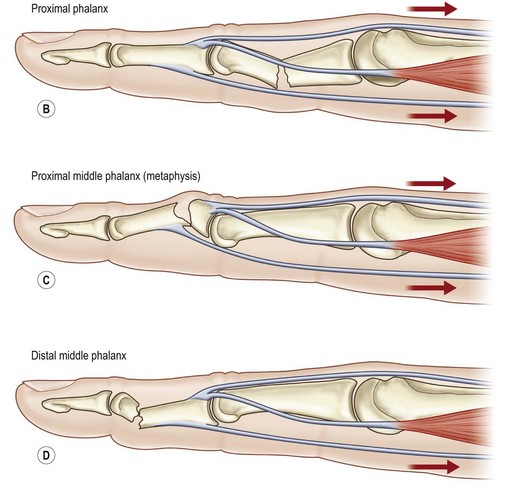
Pediatric fractures, or fractures in patients with open growth plates require special attention. The physes are located in the metacarpal neck regions in the index, long, ring, and small fingers and at the metacarpal base in the thumb. The physes of the phalanges are located at the base. Growth plate fractures are described by the Salter–Harris classification (Fig. 7.2) and (Table 7.1), with type II being the most common.
Table 7.1 Classification of Salter–Harris fractures
| Type 1 | Fracture is confined to the physis, often with normal radiographs |
| Type 2 | Fracture starts in the physis and extends through the shaft (away from the joint) |
| Type 3 | Fracture starts in the physis and extends into the joint |
| Type 4 | Fracture starts in the shaft and extends through the physis and into the joint |
| Type 5 | The physis is crushed, and there may be sheering through the physis |
Open fractures
Open fractures of the distal phalanx are treated with irrigation and debridement. If the circulation is intact and the patient is immunocompetent, antibiotics are not necessary. Fractures of other bones in the hand are treated with antibiotics in addition to irrigation and debridement. Cephalosporins are generally used and with crush injuries or heavy contamination, an aminoglycoside is added. Bite wounds (human or animal) should have penicillin added to cover anaerobes (Eikenella in human bites) and Pasteurella in animal bites (see Ch. 16).
Diagnosis
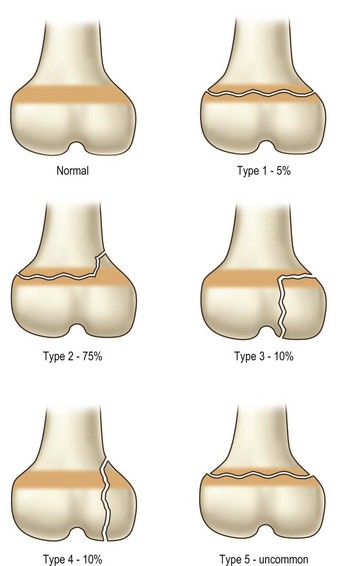
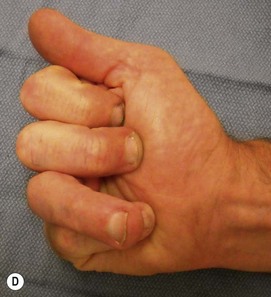
The diagnosis of hand injuries begins with a history, including hand dominance and occupation as well as the mechanism of injury. The appearance of the hand should be evaluated with the fingers extended as well as flexed. The alignment of the digits may appear normal with the fingers in extension, only to notice a rotational deformity when the digits are flexed (Fig. 7.3).
Treatment: fingers
Phalangeal fractures and dislocations
Fractures of the distal phalanx are one of the most common fractures encountered.3 They can involve the tuft, shaft, or base, often extending into the articular surface of the DIP joint. Tuft fractures are often associated with nail bed injuries and repair of the nail bed often reduces and stabilizes the fracture. Shaft fractures are often stable and patients may function well after healing with a fibrous union. For those cases where the fibrous union is symptomatic, correction of the nonunion/fibrous union can be performed.
DIP joint
Bony mallet fractures involve the dorsal aspect of the base of the distal phalanx. The dorsal aspect contains the terminal extensor tendon and the goal of treatment should be to allow healing of a congruent joint without an extension lag. Most of these can be treated with a splint, maintaining the alignment of the joint.4,5 These fractures tend to have palpable and sometimes visible prominence along the dorsal aspect of the finger following healing, even when the radiographic alignment is anatomical, but this typically does not adversely affect their function. Fractures with volar subluxation of the distal phalanx should be reduced and often require pinning of the joint to maintain the reduction.6 Several techniques have been described, but all involve reduction of the joint surface.7–9 Attempted screw placement into the fragment is difficult, even when the fragment appears large on radiograph, and often results in fragmentation of the dorsal bone. Surgical treatment of stable fractures without subluxation is generally reserved for patients who cannot wear the splint continuously during the healing process, as complications such as pin breakage, pin tract infections and subsequent osteomyelitis can occur and the risks must be carefully considered.
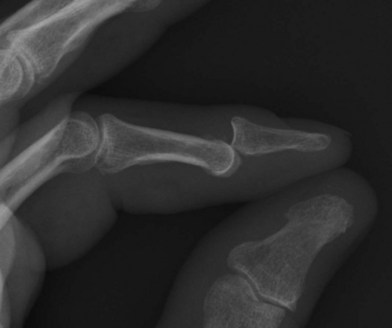
DIP joint dislocations are typically in a dorsal direction (distal phalanx is dorsal to the middle phalanx) (Fig. 7.4). Acute dislocations can often be managed by closed reduction. Flexing the wrist and MCP joints to take the tension off the flexor tendons, and applying distal pressure to the base of the distal phalanx will often reduce the joint. If this is unsuccessful, it is often due to tissue interposed in the joint – most commonly the volar plate – and an open reduction is necessary.10 This can be completed through a volar zig-zag incision or midlateral incisions. The joint is exposed and any intervening tissue is removed, taking care to avoid damaging the articular cartilage, and the joint is reduced. Late presentation of DIP joint dislocations will usually require open reduction, using the same technique. Following reduction, these injuries are typically stable and early motion can be started using a dorsal blocking splint.
PIP joint injuries
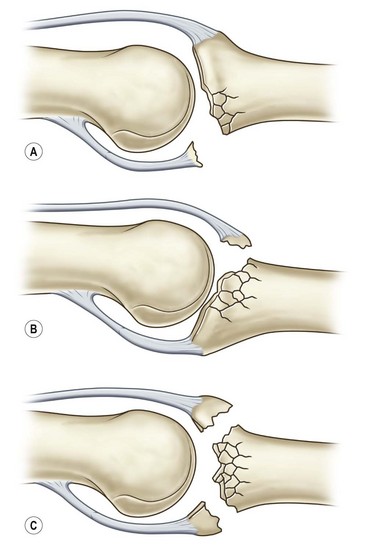
Injuries involving the PIP joint can involve the volar base of the middle phalanx, the head of the proximal phalanx, a pure dislocation, or any combination of these. Fractures involving the base of the middle phalanx include dorsal base fractures (involving the insertion of the central slip of the extensor mechanism), the volar base, resulting dorsal subluxation of the middle phalanx, avulsion of the collateral ligaments, or pilon type of fracture involving the dorsal and volar margins, with a depressed central articular fragment (Fig. 7.5). Fractures involving the proximal phalanx head can involve one or both condyles and can occur with or without proximal extension.
Pure dislocations result from hyperextension and an axial load. They are often dorsal dislocations and are managed similar to the DIP joint, with an initial trial of closed reduction (with the wrist and fingers flexed and distal pressure on the base of the middle phalanx). When successful, a dorsal blocking splint and early active flexion can produce good results. When reduction cannot be completed by closed means, open reduction is indicated, either through a volar or mid-lateral approach.11
Volar dislocations are less common, but can lead to late deformities if not recognized and treated.12 The central slip is often injured and can result in late boutonniere deformities. Following reduction, splinting the PIP joint in extension and active flexion of the DIP joint will allow gliding of the lateral bands. Active flexion can be started following three weeks, as further immobilization of the PIP joint may result in permanent stiffness. Irreducible dislocations are due to an interposed central slip or collateral ligament and require open reduction through a dorsal approach, allowing direct inspection of the central slip.
Middle phalanx base articular fractures
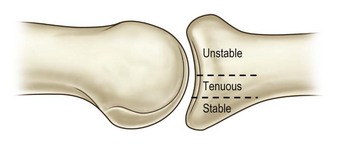
Fracture dislocations of the PIP joint result from an axial load in a dorsal direction or longitudinal direction when the finger is slightly flexed. These injuries are classified according to the amount of the articular surface involved. Fractures involving <30% of the articular surface of the base of the middle phalanx are typically stable and can be managed nonoperatively. Fractures involving 30–50% of the articular surface are tenuous and often are unstable. Fractures involving >50% are unstable and result in dorsal subluxation of the middle phalanx (Fig. 7.6).13
Lateral radiographs should be carefully evaluated for the “V sign”, indicative of dorsal subluxation (Fig. 7.7). The two condyles of the proximal phalanx should be superimposed and the base of the middle phalanx should be collinear with the head of the proximal phalanx. There should be a smooth curvature of the joint surface, with a consistent space between the proximal and middle phalanx. If there is convergence of the joint space creating a dorsal “V”, the patient may be able to flex the digit at the PIP joint, but this occurs through a hinge process rather than rotation, and the joint surface will degenerate.
A variety of techniques have been described, including extension block pinning,14,15 open reduction and internal fixation,16 volar plate arthroplasty,17,18 replacement arthroplasty,19,20 and external fixation.21–23 All of these techniques have case reports or small series illustrating good outcomes, but there are no prospective studies indicating one technique is better than others for a particular injury.
Hints and tips
External fixation
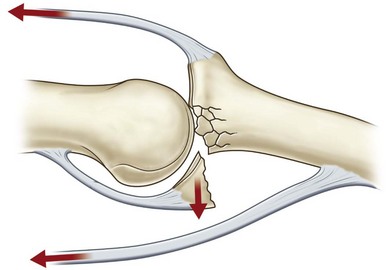
A variety of devices have been described for management of PIP joint fracture dislocations.21–24 The common principle is to produce distraction across the joint, allowing alignment to be maintained through ligamentotaxis. In addition, some devices provide a volar directed force on the middle phalanx to assist in maintaining alignment. They all allow immediate PIP joint motion. Careful attention should be paid to the fragments along the volar base of the middle phalanx as dorsal subluxation can recur if these do not heal in proper position (the volar lip of the base of the middle phalanx is a restraint to dorsal subluxation, so healing of the fracture fragments must recreate the normal curvature).
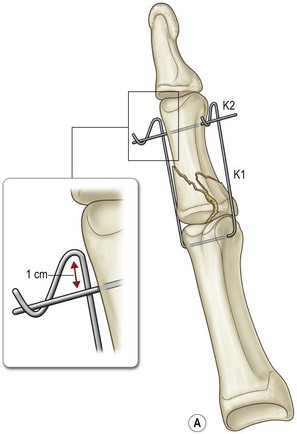
External fixation systems can be fabricated from K-wires with or without the use of rubber bands or commercially available devices can be used. Figure 7.10 illustrates and example of a PIP joint fracture dislocation in the small finger managed with an external fixator fabricated from K-wires.
Technique of external fixation
A 0.045-inch K-wire is inserted through the head of the proximal phalanx, perpendicular to the joint surface (Fig. 7.8). A second 0.045-inch K-wire is inserted through the distal shaft of the middle phalanx, parallel to the DIP joint surface. The proximal wire is bent distally along the radial and ulnar aspects, paralleling the digit. Distal to the second wire, a dorsal proximal bend is created, followed by a dorsal distal bend. The bends should be at the same level on both the radial and ulnar sides. This creates a groove in the proximal wire for the distal wire to be positioned, allowing slight distraction across the joint, which will aid the reduction via ligamentotaxis. Increasing or decreasing the first bend on the proximal wire can adjust the distraction across the joint. This can be performed under local anesthesia and immediate motion is initiated. The fixator is left in place for approximately six weeks and rehabilitation focuses on motion of the PIP and DIP joints. The joint surface will remodel over time.
Internal fixation
Internal fixation of middle phalanx base fractures can be demanding, but good results can be obtained. Postoperative rehabilitation is critical to a good outcome, so the patient must be compliant or the result can be a good radiograph with a stiff nonfunctional finger. Larger fragments can often be stabilized with small screws, reconstructing the volar base of the middle phalanx (Fig. 7.9). Dorsal fragments can be stabilized with screws or K-wires to reinsert the central slip. Comminution at the base of the middle phalanx creates a greater challenge and the surgeon should be prepared for this as often what appears as a large piece on X-ray is found to be multiple smaller pieces. If the articular surface can be reduced, a cerclage wire may be used to hold the bone fragments in place (Fig. 7.10).25 This may provide adequate stability to allow early motion.
The volar plate arthroplasty was described by Eaton and Malerich in 198018 and involves removing the comminuted portion of bone along the volar aspect of the base of the middle phalanx, creating a trough parallel to the dorsal surface of the middle phalanx, and advancing the volar plate to resurface the joint. The volar plate is attached to the bone, either through drill holes or with a permanent suture at the lateral aspect. The joint is temporarily pinned in slight flexion. At 3 weeks, the pin is removed and motion is begun.17 The volar plate serves to prevent dorsal subluxation of the middle phalanx. The results with this technique can be unpredictable as stiffness and recurrent dorsal subluxation can occur. Long-term follow-up of Dr Eaton’s patients have been published with good results,26 but there are few recent reports of this procedure.
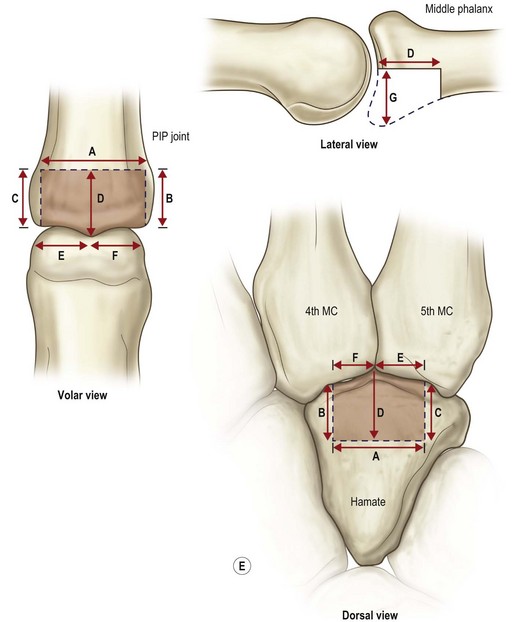
More recently, the hemi-hamate replacement arthroplasty has been described (Hastings et al. ASSH annual meeting, 1999) and subsequently published. The dorsal distal portion of the hamate has similar anatomy to the volar base of the middle phalanx. Osseous cuts must be precise and the curvature of the volar base of the middle phalanx must be reproduced or persistent dorsal subluxation will occur. This can be rigidly fixed and early motion can be instituted. Published series have shown promising results.20,27
Technique of HHRA
The procedure can be performed under regional or general anesthesia. The finger is approached from the volar aspect with a Bruner incision from the palmodigital crease to the DIP flexion crease (Fig. 7.11). Skin flaps are elevated and retracted. The digital neurovascular bundles are freed so they are not under tension when the joint is exposed. A radial or ulnar based flap of the flexor sheath is created between the A-2 and A-4 pulleys. The collateral ligaments are released from the middle phalanx, leaving a small stump for later repair, and the volar plate is released from fragments at the base of the middle phalanx. The neurovascular bundles are inspected to make sure they will not tether as the joint is exposed. The flexor tendons are retracted and the joint is shot gunned open exposing the joint. If resistance is encountered, it is usually due to the collateral ligaments; these are inspected, ensuring complete release from the middle phalanx.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree