I. MEETING THE PATIENT
A. ABCs (airway, breathing, circulation) of trauma for all injured patients
B. AMPLE (allergies, medications, past medical history, time of last meal, and events leading to injury) history, and details on exact mechanism of injury
C. Focused history: Handedness, vocation/avocations, smoking history, diabetes, or vascular diseases?
D. Examine the joint(s) proximal and distal to any injury.
E. Order appropriate X-rays, select other imaging studies as needed.
F. Tetanus prophylaxis and antibiotics if needed (open fractures)
II. TENDONS AND MUSCLES
A. Common abbreviations
1. BR: Brachioradialis
2. FCR/FCU: Flexor carpi radialis/ulnaris
3. FPL: Flexor pollicis longus
4. FDS/FDP: Flexor digitorum superficialis/profundus
5. ECRL/ECRB: Extensor carpi radialis longus/brevis
6. ECU: Extensor carpi ulnaris
7. EDC: Extensor digitorum communis
8. EIP: Extensor indicis proprius
9. FDM/EDM: Flexor/extensor digiti minimi (or EDQ, extensor digiti quinti)
10. EPL/EPB: Extensor pollicis longus/brevis
11. PL: Palmaris longus (absent in 15% of people)
12. PB: Palmaris brevis
13. PT: Pronator teres
14. PQ: Pronator quadratus
15. AdP: Adductor pollicis
16. APL/APB: Abductor pollicis longus/brevis
17. ADM: Abductor digiti minimi
18. ODM: Opponens digiti minimi
B. Flexor tendons
1. Five flexor tendon zones. See Chapter 40.
2. Flexor muscles originate largely at the medial epicondyle of the humerus, with some deeper compartment muscles originating on radius and ulna.
3. Superficial: PT, FCR, FCU, PL; Intermediate: FDS; Deep: FDP, FPL
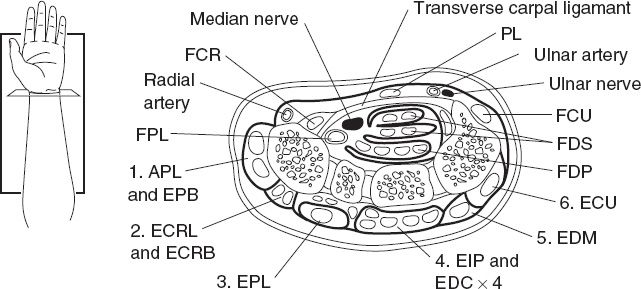
4. Carpal tunnel contains median nerve and nine tendons: FDP(4), FDS(4), and FPL (Fig. 38-1)
a. FDS is superficial to the FDP in carpal tunnel
b. FDS MF and RF are volar to FDS IF and SF
5. FDS
a. Muscle bellies are innervated by median nerve and divide in forearm: Less power, but better independent function than FDP (note: 15% of people do not have independent FDS to SF because FDS to ring and small fingers may be conjoined).
______________
*Denotes common in-service examination topics
Figure 38-1. Cross section through the wrist, including extensor tendon compartments 1 to 6. APL, abductor pollicis longus; ECRB, extensor carpi radialis brevis; ECRL, extensor carpi radialis longus; ECU, extensor carpi ulnaris; EDC, extensor digitorum communis; EDM, extensor digiti minimi; EIP, extensor indicis proprius; EPB, extensor pollicis brevis; EPL, extensor pollicis longus; FCR, flexor carpi radialis; FCU, flexor carpi ulnaris; FDP, flexor digitorum profundus; FDS, flexor digitorum superficialis; FPL, flexor pollicis longus; PL, palmaris longus.
b. Tendon splits into radial and ulnar slips prior to inserting into the volar base of the middle phalanx.
c. FDP passes between the two FDS slips, also known as “Camper’s chiasm”
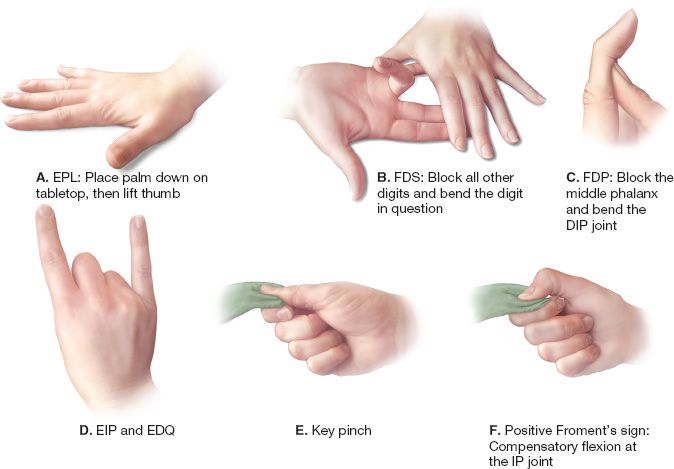
d. Test: Lay the hand flat on table and palm up. Hold other fingers in extension (blocks FDP), test active flexion at each proximal interphalangeal joint (PIPJ). Also test against resistance.
6. FDP
a. Dually innervated (IF/MF median n, RF/SF ulnar n.)
b. Common muscle belly affords more power but less independent function—IF branches off first, but can only get ~30 degrees of IF flexion before other digit FDPs begin to engage
c. Inserts into proximal volar aspect of the distal phalanx.
d. Test: PIPJ held in extension (pressure on middle phalanx), test active dorsal interphalangeal joint (DIPJ) flexion
7. FPL
a. Inserts into distal phalanx of the thumb
b. Test: Check active flexion of interphalangeal joint (IPJ) with metacarpophalangeal blocked (pressure on proximal phalanx). Also check against resistance.
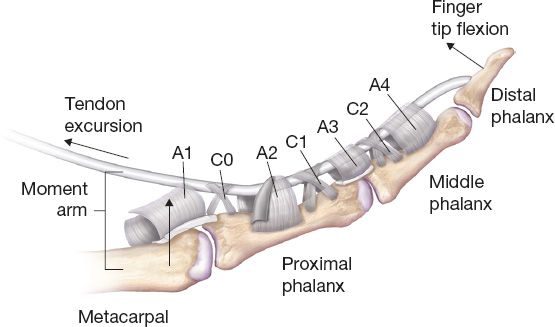
8. Pulleys: Prevent tendon bowstringing, increase mechanical effectiveness of pull across joints (Fig. 38-2)
a. Fingers have five annular pulleys (A1 to A5)
i. A2 (over proximal phalanx) and A4 (over distal phalanx) are usually considered most critical to finger function
ii. Others over joints—A1 (MPJ), A3 (PIPJ), and A5 (DIPJ)
b. Fingers also have three cruciate pulleys—C1 (between A2/A3), C2 (between A3/A4), and C3 (between A4/A5)
c. Thumb has three pulleys: A1 (MPJ), A2 (IPJ), and oblique (over proximal phalanx). Oblique pulley is most mechanically important.
C. Extensor tendons
1. Nine extensor tendon zones. The odd-numbered zones (1 to 7) lie over joints, with the even-numbered zones in between (see Chapter 40).
2. Extensor muscle mass (aka “mobile wad”) originates largely at the lateral epicondyle
3. Superficial: EDC, EDM, ECU; Deep: APL, EPB, EPL, EIP; Lateral/radial: ECRL, ECRB, BR
Figure 38-2. Flexor sheath pulley system. A1–A5, annular pulleys; C1–C3, cruciate pulleys.
4. Junctura tendinae: Interconnect tendons on back of the hand. May mask an extensor tendon rupture, as pull from another finger can be transmitted via juncturae to the distal extensor tendon of the injured finger.
5. Dorsal wrist compartments (listed radial to ulnar)
a. 1: APL, EPB
b. 2: ECRL, ECRB
c. 3: EPL (which then hooks around Lister tubercle to reach the thumb)
d. 4: EDC, EIP
e. 5: EDM
f. 6: ECU
6. EIP, EDM
a. These tendons are ulnar to their accompanying EDC tendons
b. Test: Independent extension of the IF or SF with other fingers flexed
7. EPL: Test: Check the ability to raise the thumb up with the hand prone and flat on table
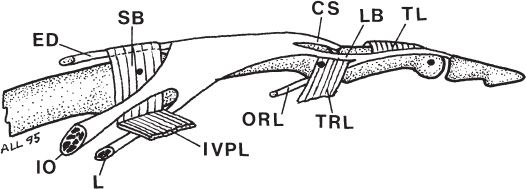
8. Extensor mechanism (Fig. 38-3)
a. EDC (plus EIP and EDM) expands over MPJ to form extensor hood for each digit. Most extrinsic tendon function translated to the MPJ.
b. Sagittal bands help stabilize the extensor tendon across the MPJ and form a “bucket handle” with insertions on volar plate
c. The lumbrical and interosseous tendons join the hood laterally to add MPJ flexion and provide IPJ extension
d. The extensor hood divides into three components over the proximal phalanx
i. Central slip inserts on the base of the middle phalanx for PIPJ extension
ii. Two lateral bands continue distally and fuse, inserting on the base of the distal phalanx (terminal tendon) for DIPJ extension
e. Oblique retinacular ligament (of Landsmeer)
i. Cord that runs from flexor tendon sheath at the proximal phalanx to the terminal. extensor tendon.
ii. When PIP joint is flexed, ligament relaxes allowing DIP flexion.
iii. PIP extension tightens ligament facilitating DIP extension, thus linking motion of PIP and DIP joints.
iv. Contracture causes Boutinierre deformity.
f. Transverse retinacular ligament.
i. with PIP flexion, pull lateral bands volarly over PIP.
Figure 38-3. Extensor tendon anatomy in the digit. CS, central slip; ED, extensor digitorum; IO, interosseous; L, lumbrical; LB, lateral band; ORL, oblique retinacular ligament; SB, sagittal band; TL, triangular ligament; TRL, transverse retinacular ligament; VPL, volar plate ligament.
ii. with PIP extension, prevents excessive dorsal translation of lateral bands.
iii. attenuation leads to dorsal translation of lateral bands and a resulting Swan Neck Deformity.
D. Intrinsic muscles
1. AdP: Test for key pinch (thumb to side of IF) by having the patient hold a piece of paper deep in the web space and resist the paper from being pulled away; if FPL takes over (DIPJ flexes), this is a positive “Froment’s sign” and implies AdP function is absent or diminished (compare to the opposite side)
2. Thenar: Opponens pollicis (OP), APB, flexor pollicis brevis (FPB) (dual innervation)
3. Hypothenar: ODM, FDM, ADM, PB
4. Interosseous muscles
a. Three palmar and four dorsal
b. Test for abduction/adduction of fingers (and to resistance)
c. Palmar interossei adduct IF/RF/SF and dorsal interossei abduct IF/MF/RF/SF. [Think PAd and Dab.]
d. Innervated by the ulnar nerve
5. Lumbricals
a. Origin of each lumbrical is on the radial side of FDP tendon in the palm.
b. In the palm, the radial digital nerve runs volarly on the muscle belly of the lumbrical to that digit.
c. Lumbricals are innervated by the same nerve as the FDP they originate from—IF/MF by median and RF/SF ulnar.
6. Intrinsic tightness test
a. With the wrist neutral, hyperextend the MPJ to relax the extrinsics
b. Measure passive flexion of PIPJ (“intrinsic tightness”)
i. Mild: 60 to 80 degrees
ii. Moderate: 20 to 59 degrees
iii. Severe: <20 degrees
7. Extrinsic tightness test
a. With wrist neutral, flex the MPJ to relax the intrinsics
b. Check passive PIP motion, which will indicate “extrinsic tightness”
III. VASCULATURE
A. Arterial supply
1. Radial artery supplies the deep palmar arch, which gives off princeps pollicis which branches to proper digital artery to the thumb and radialis indices to index finger.
2. Ulnar artery supplies the superficial palmar arch, which provides the common digital arteries and individual branch to ulnar side of small finger.
3. *The radial artery is usually dominant, but ulnar dominance and codominance are common (and some studies indicate ulnar dominance is more common).
4. *“Kaplan’s cardinal line” is a line drawn across the palm from the first web space to the hook of the hamate, indicating approximate location of the superficial palmar arch. Deep arch is 1 cm proximal.
5. Dorsal Carpal Arch:
a. Fed from radial, ulnar and interosseous arteries.
b. Gives rise to dorsal metacarpal arteries.
B. Venous drainage
1. Dorsal (subcutaneous) venous network and palmar venous arch
2. Drain to cephalic vein (originates radially) and basilic vein (originates on the dorsoulnar aspect of the hand)
C. Allen test
1. Compress radial and ulnar arteries at the wrist, have the patient make a tight fist (to exsanguinate hand) and then relax; release one vessel to check patency of the palmar arch and blood supply to the hand via that artery. Repeat for the other.
2. A digital Allen test can be done to isolate the radial or ulnar vessel of a finger
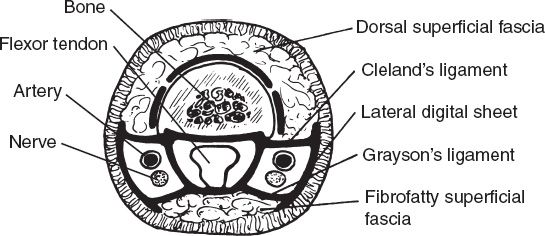
D. Relationship between paired arteries and nerves
1. In the palm: Arteries are volar to nerves
2. In the digits: Arteries are dorsal to nerves (Fig. 38-4)
E. Capillary refill should be 2 to 3 seconds; check nail bed or eponychial fold
IV. NERVES
A. Radial nerve anatomy
1. Enters the forearm between the BR and the ECRL/ECRB (innervates these three muscles)
2. Divides (1 to 3 cm distal to lateral epicondyle, deep to BR)
a. Posterior interosseous nerve
i. Passes between the heads of the supinator, innervates (in order, proximal to distal) the supinator, EDC, ECU, EDM, APL, EPB, EPL, and EIP
ii. Sensory branch to the wrist capsule (deep within the fourth dorsal compartment of the wrist)
b. Superficial radial nerve
i. Exits between BR and ECRL tendons approximately two-third down the forearm
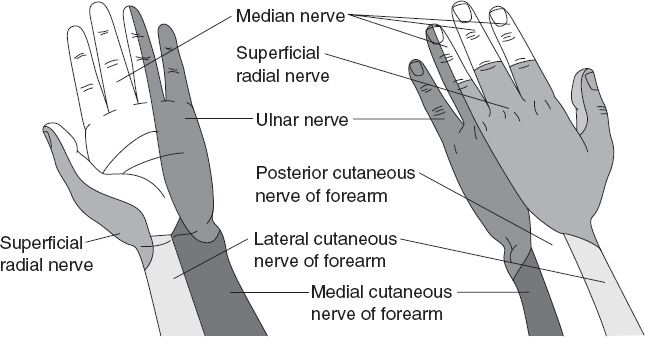
ii. Provides sensory to dorsum of the thumb, first web space, dorsal IF, MF, and radial RF up to the PIPJs (Fig. 38-5)
B. Median nerve anatomy
1. Enters forearm lateral to the brachial artery, emerging between the heads of the PT; innervates the PT, FCR, FDS, and PL
2. Branches (at junction of the two heads of PT, ~6 cm distal to elbow)
a. Anterior interosseous nerve (AIN)
i. Innervates (in order) FPL, PQ, radial two FDPs (IF and MF)
ii. Sensory to wrist capsule
Figure 38-4. Cross section of the digit.
Figure 38-5. Cutaneous sensory innervation of the hand, volar and dorsal surfaces.
iii. Runs with anterior interosseous artery on interosseous membrane
b. Remainder of median nerve runs between FDS and FDP. Gives palmar cutaneous (sensory) branch ~5 cm proximal to the wrist, then enters the carpal tunnel and splits again
i. Recurrent motor branch: Innervates Lumbricals (2), OP, APB, and FPB (lumbricals, opponens pollicis, abductor pollicis, flexor pollicis brevis—abductor pollicis brevis, flexor pollicis brevis, opponens pollicis, and lumbricals is in order of innervation)
ii. Sensory: Digital nerves (thumb, IF, MF, and radial RF) (Fig. 38-5)
C. Ulnar nerve anatomy
1. *Enters the forearm behind the medial epicondyle through the cubital tunnel under Osborne’s band/ligament; innervates FCU and ulnar two FDPs (RF and SF)
2. Travels under FCU to the wrist, gives off dorsal sensory branch ~6 to 8 cm proximal to ulnar head, providing sensation to the dorsum of SF and ulnar RF (Fig. 38-5). Then enters Guyon’s canal and branches again
a. Deep branch: Innervates ADM, FDM, ODM, deep head of FPB, all interosseous muscles, ulnar lumbricals (2), and AdP (terminal branch)
b. Superficial branch: Innervates PB then provides sensory palmar digital nerves to SF and ulnar RF
3. Median nerve cross-innervation can mask an ulnar nerve injury
a. *Martin–Gruber anastomosis: An anatomic variant in which the median nerve crosses over to contribute to the ulnar nerve. The two most common variations are
i. Median nerve in the proximal forearm contributes to the ulnar nerve in the distal forearm.
ii. AIN contributes to the ulnar nerve
b. Riche–Cannieu anastomosis: More distal, ulnar fibers contribute to the median nerve branches in the palm
D. “Quick and simple” nerve exam (Fig. 38-6)
1. Median nerve: Sensation at the tip of IF (light touch and two-point discrimination); ability to make “OK” sign: Demonstrates FPL, FDP, and OP
2. Ulnar nerve: Sensation at the tip of SF; ability to abduct/adduct/cross fingers. Test AdP (see below)
3. Radial nerve: Sensation dorsal first web space; give “thumbs up” (EPL)
Figure 38-6. Specific hand exam techniques. Specific movements are used to isolate and test the functions of the hand.
V. BONE AND JOINTS
A. Wrist
1. Radius and ulna articulate with each other and with the carpus.
2. Conceptually, the radius rotates around the fixed ulna at the wrist, sliding distally with pronation.
B. Carpus
1. Eight bones: radial to ulnar—proximal row: Scaphoid, lunate, triquetrum, pisiform; distal row: Trapezium, trapezoid, capitate, hamate. Mnemonic: “Some Lovers Try Positions That They Cannot Handle”
2. Pisiform is a sesamoid bone imbedded in the FCU tendon.
3. Radiocarpal and midcarpal joints stabilized by ligaments
a. All ligaments are intracapsular
b. The interosseous ligaments are intra-articular as well
c. Ligament integrity is critical for the normal wrist motion and stability, as no tendons insert directly on the carpal bones but rather attach through these ligaments and joint capsules.
4. Normal alignment: The capitate is collinear with the lunate and the third metacarpal.
5. Gilula’s lines
a. Arcs formed by the outlines of the carpal bones, seen on AP radiographs of the wrist
b. The proximal row forms the proximal arc, and the proximal edge of the distal row forms the distal arc
c. The arcs should be smooth and continuous
6. Scapholunate interval: On AP view of the wrist, if space between the scaphoid and the lunate is >2 to 3 mm, this indicates possible scapholunate dissociation (may need to compare with contralateral side radiograph)—“Terry Thomas sign”
7. *Scapholunate angle: Measured on lateral radiograph. Normal is 30 to 60 degrees.
a. Angle >60 degrees is indicative of possible dorsal intercalated segment instability deformity
b. Angle <30 degrees indicated possible volar intercalated segment instability deformity
C. Fingers
1. Five metacarpals, 14 phalanges (3 per finger, 2 in thumb)
2. “Protected splinting position” with the wrist gently extended, thumb in palmar abduction, and fingers with MPJ flexed to 70 degrees, PIPJ and DIPJ fully extended
a. A cam effect is created over the ovoid contour of the metacarpal head. As a result, the collateral ligaments are tight in flexion but lax in extension and must be protected from shortening by flexing the MPJ.
b. At the IPJ the issue is different
i. When flexed, the check rein ligaments coordinate the volar plate sliding proximally. In this position, the plate can become adherent to the tendon or periosteum and result in flexion contracture.
ii. When flexed, the extensor mechanism is stressed. Prolonged stress (especially with surrounding inflammation) can result in disruption of transverse retinacular ligaments, allowing lateral bands to slip, and causing boutonniere deformity.
3. Joint mechanics (see Chapter 39)
D. Normal ranges of motion (approximate)
1. Finger MPJ: 0 to 45 degrees hyperextension, 90 degrees flexion
2. Finger PIPJ: 0 degrees extension, 100 degrees flexion
3. Finger DIPJ: 0 degrees extension, 70 to 80 degrees flexion
4. Thumb MPJ: 10 degrees hyperextension, 55 degrees flexion, 90 degrees in full range of radial adduction/abduction
5. Thumb IPJ: 15 degrees hyperextension, 80 degrees flexion
6. Wrist: 70 degrees extension, 75 degrees flexion, 20 degrees radial deviation and 35 degrees ulnar deviation
7. Forearm: 70 degrees pronation, 85 degrees supination
VI. TOURNIQUET USE
A. Never place a digital tourniquet without an obvious reminder to remove it (e.g., hemostat and sterile glove) to avoid digital loss.
B. Blood pressure cuffs make good arm tourniquets in the ER. Arm tourniquet should be wide to distribute pressure.
C. Try to wait on inflating the arm tourniquet until you have done an exam. Minimize cycles of placing/removing a tourniquet during the acute evaluation of a traumatized limb. If possible, use direct pressure to stop bleeding until exam is complete.
D. Tourniquet pressure should be 125 to 150 mmHg above systolic pressure (usually set around 230 to 250 mmHg). Always inflate fully!
E. Limit continuous tourniquet time to 2 hours to prevent permanent damage and minimize patient discomfort from tourniquet.
1. *Nerves are the most vulnerable to pressure/hypoxia
2. Blood flow should be returned to the ischemic part for 5 minutes for every 30 minutes of ischemia (i.e., deflate tourniquet for 20 minutes every 2 hours)
3. Do not progressively loosen a tourniquet: Either have it fully inflated, or let it down completely and use pressure to control bleeding as needed
VII. NERVE BLOCKS
A. See Chapter 10 for details about local anesthetics
B. Median nerve
1. Needle at distal wrist crease between PL and FCR; enter at 45 degree angle to the forearm; often a “pop” is felt when deep fascia is penetrated.
2. If unsure of depth, insert until paresthesias occur or bone is encountered, then withdraw slightly and inject 3 to 5 cc local anesthetic.
C. Ulnar nerve
1. Place the needle just proximal to the ulnar styloid; enter behind the FCU tendon with the needle directed from ulnar to radial in the coronal plane.
2. Once needle is just beyond FCU, inject anesthetic (3 to 5 cc).
3. Must inject dorsally on the wrist to get dorsal sensory branch.
D. Radial nerve
1. Must block a wide area
2. Start proximal to the radial styloid and inject the subcutaneous tissue.
3. Extend the field block volar and dorsal around the distal forearm.
E. Digital block
1. Dorsal approach
a. Subcutaneous wheal over extensor tendon to block dorsal nerves.
b. Injections just proximal to each web space: Advance needle until the tip approaches the palmar skin, inject slowly while withdrawing.
2. Volar approach
a. Subcutaneous wheal directly over the flexor tendon
b. Slightly deeper on each side, near the digital neurovascular bundles
3. Sheath approach
a. One injection: Insert needle volar, just distal to distal palmer crease, down into the flexor tendons
b. With slight pressure on the plunger, withdraw needle slowly until there is a loss of resistance = injection into potential space of flexor sheath
c. Sometimes fluid wave can be felt distally in the finger over the sheath
d. Reliably results in digital anesthesia, but is not as effective in cases of sheath violation (e.g., distal amputation)
VIII. INCISIONS ON THE HAND
A. When planning incisions, avoid crossing flexion creases at a right angle
1. Mid-axial incisions: with the finger fully flexed, mark the radial and ulnar extent of the flexion crease at each finger joint. Connect these dots.
2. Bruner incisions: Incisions on the flexor surface that diagonally connect mid-axial point to mid-axial point.
B. Extensor surface with less risk of scar contracture limiting function. Longitudinal, curvilinear, and transverse incisions usually all acceptable.
PEARLS
1. Develop a system for the hand exam that goes through the key anatomical components and use it every time—avoid shortcuts and stay organized so nothing gets missed
2. Always document neurovascular exam BEFORE injecting local anesthetic, and if possible before inflating a tourniquet
3. Test function against RESISTANCE—may detect a partial injury that is otherwise compensated
4. Whenever in doubt, compare the injured hand to the uninjured one to help identify abnormalities
5. Always incorporate a “reminder” when applying a tourniquet
QUESTIONS YOU WILL BE ASKED
1. What structures on the extensor surface of the finger might mask an extensor tendon injury?
Junctura tendinae.
2. What is maximum tourniquet time? How long must you release the tourniquet if the case is longer than the maximum and you wish to use another tourniquet run?
a) 2 hours.
b) 5 minutes for every 30 minutes of tourniquet time.
3. What is the standard protected position for splinting the hand and wrist? Why?
a) Intrinsic plus with thumb in palmar abduction.
b) See Section V, subsection C.
4. What is the last muscle innervated by the ulnar nerve? How is it tested?
a) Adductor pollicus
b) Key pinch/Froment sign. See Section II, subsection D.
5. In the finger, how are nerve and artery related in position?
a) Nerve is volar to artery (opposite orientation in the palm).
6. Relative position of extensor indicis and the corresponding extensor digitorum to the index finger?
EIP is ulnar to EDC tendon.
7. Of the different pulleys in the flexor system, which are the most important to preserve? Why?
a) A2 and A4.
b) Prevent bowstringing of the tendon overlying the proximal (A2) and middle (A4) phalanx.
As a chapter mostly focused on anatomy, much of the content should be reviewed before any hand/upper extremity trauma case.
THINGS TO DRAW
1. Cross section of the carpal tunnel
2. Bruner incision pattern on a digit
3. Identify and mark Kaplan’s cardinal line
Recommended Readings
Mazurek MT, Shin AY. Upper extremity peripheral nerve anatomy: current concepts and applications. Clin Orthop Relat Res. 2001;(383):7–20. PMID: 11210971.
Moore KL, Dalley AF and Agur AMR. Clinically Oriented Anatomy. Lippincott, Baltimore, 2009.
< div class='tao-gold-member'>