Chapter 39 Hamstring Tendon Interference Screw Fixation
Biomechanical and Biological Considerations
The concept of interference screw fixation involves the parallel insertion of the screw to the graft in the tunnel, which allows compression of the graft to the bony tunnel wall and biological graft incorporation. Graft fixation using interference screws presents the “gold standard” when using a bone–patellar tendon–bone (BPTB) graft. This type of fixation combines high initial construct stiffness and early bony graft incorporation.1 These factors are generally required to allow for an accelerated rehabilitation, which has been demonstrated to improve clinical outcome.2 Soft tissue grafts, however, do not provide attached bone blocks for interference fit fixation. Additionally, tendon–bone healing generally takes longer for bony graft incorporation compared with bone–bone healing (4 to 6 weeks versus 6 to 12 weeks).3–7 Thus fixation of soft tissue grafts requires improved mechanical and biological boundary conditions for graft fixation compared with grafts with attached bone blocks.
Biomechanical Boundary Conditions
Ideally, a graft fixation construct should be similar in strength and stiffness to the native human anterior cruciate ligament (ACL). Current fixation techniques demonstrate a wide range of in vitro measured graft fixation loads (200N to 1200N). However, today evidence is still limited regarding real in vivo requirements for initial construct strength.8 Noyes et al calculated that the ACL is loaded up to 454N during activities of daily living,9 but other authors reported a high amount of good and excellent results with fixation types whose failure load is far below that anticipated value.10–12 For soft tissue graft fixation using biodegradable interference screws, failure loads of 250N to 800N have been demonstrated depending on screw length and insertion torque.13–15
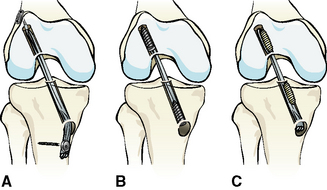
Graft fixation generally is divided into anatomical (aperture or joint line fixation), nonanatomical, and semi-anatomical (Fig. 39-1), according to the location of fixation in relation to the joint line. Graft fixation directly at the joint line (site of the native ACL insertion) is called anatomical, whereas an extracortical fixation (e.g., staples, fixation buttons) is called nonanatomical. For example, transfixation devices or tibial interference screws that are not deeply inserted provide an intraosseous and thus a semi-anatomical mounting of the graft.
This classification is important because the site of graft fixation determines the length of the complete graft fixation construct. The length of the native ACL is between 2.8 and 3.7 cm. Reconstruction of the anteromedial bundle of the ACL results in an intraarticular graft length of only approximately 2.5 to 3.2 cm. Using femoral and tibial nonanatomical fixation devices, the length of the graft fixation construct can easily reach 10 to 15 cm (see Fig. 39-1). In correlation to the distance between the fixation devices, reversible elastic longitudinal deformations of the graft have been demonstrated. This phenomenon also is known as the “bungee-cord effect.” Furthermore, sagittal intratunnel graft motion (reversible) might occur due to anteroposterior translation of the graft during knee flexion and extension using a nonanatomical or semianatomical graft fixation technique (“windshield-wiper effect”).15,16 Thus a long distance between the femoral and tibial fixation device results in low construct stiffness and graft–tunnel motion.
Additionally, indirect and direct graft fixation should be distinguished (see Fig. 39-1). The concept of indirect graft fixation implicates the use of linkage material between graft and fixation device (e.g., suture loop of Endobutton fixation), whereas direct fixation means anchoring of the graft without any additional material except the fixation device itself (e.g., interference screws, staples, transfixation devices). Longitudinal irreversible graft deformation might occur using indirect fixation techniques due to stretch-out of linkage material (e.g., suture loop of Endobutton fixation) or suture attachment at the graft tissue.13,17,18
Longitudinal and sagittal graft–tunnel motion inhibits constant graft–tunnel contact at the tunnel entry site and thus compromises bony graft incorporation at the site of the native ACL insertion.5,19 Furthermore, graft–tunnel motion might lead to graft laceration at the tunnel entry site during dynamic loading20 and is a factor responsible for the development of tunnel enlargement.16 Although current literature is not consistent concerning the correlation between tunnel enlargement and postoperative knee stability16,21,22 in revision ACL reconstruction, tunnel enlargement is of clinical importance and should therefore be prevented.
According to these considerations, interference screw fixation offers high construct stiffness and prevents intratunnel graft motion because it allows for direct and anatomical graft fixation at the level of the joint line combined with adequate initial fixation strength.5,23 Recent clinical data support the belief that clinical outcome can be improved with anatomical joint line fixation using interference screws for hamstring tendon grafts.24
Biological Boundary Conditions
In addition to correct tunnel placement, graft incorporation represents the main factor for long-term survival of an ACL reconstruction and is mainly influenced by the type of fixation. The surgical target is to create biological (and biomechanical) boundary conditions that allow for the restitution of a native ACL insertion site anatomy.5 The normal ACL insertion site consists of four zones (so-called direct ligament insertion). The first zone comprises the ligament, the second is characterized by fibrocartilage, the third zone consists of a mineralized cartilage tidemark, and the fourth is where the mineralized cartilage tidemark inserts into the subchondral bone plate.5 The design of this complex insertion anatomy allows distribution of longitudinal and shear forces from the ligament into the subchondral bone plate. The development of a direct ligament insertion at the level of the joint line has been demonstrated histologically in an animal model using anatomical soft tissue graft fixation with compression at the tunnel entry site (interference screws).25 In contrast, the use of a nonanatomical fixation technique in the same model showed the development of an indirect type of ligament insertion or only a delayed formation of a direct type of insertion.25 In indirect insertions, the surface of the ligament connects with the periosteum whereas the deeper layers connect to bone via Sharpey fibers (e.g., medial collateral ligament). This is of inferior mechanical competence compared with the direct ligament insertion.5
Thus it is reasonable to assume that neutralization of graft-tunnel motions using anatomical and direct interference screw fixation obviously improves osseous graft incorporation by means of the development of a native ACL insertion anatomy.25
Interference Screws
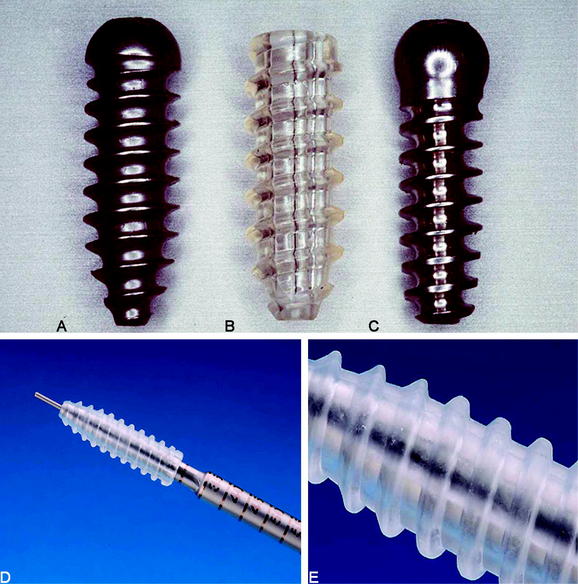
Metallic interference screws initially were developed for fixation of grafts with attached bone blocks. These screws are threaded sharply to achieve good starting conditions for screw insertion and secure graft fixation. The use of this type of interference screw for soft tissue graft fixation might lead to laceration of the graft tissue during screw insertion, especially if high insertion torque is generated. Thus different round-threaded interference screws have been developed for soft tissue graft fixation.26,27 The first round-threaded metallic interference screw for direct fixation of soft tissue grafts was developed by L. Pinczewski, the round-headed cannulated interference screw (RCI)10,26 (Fig. 39-2). More recently, biodegradable interference screws have been developed and biomechanically as well as clinically tested for fixation of BPTB and soft tissue grafts.27,28 Soft tissue graft fixation using biodegradable interference screws was first described by Stähelin and Weiler.29
Biodegradable interference screws have been demonstrated to be advantageous compared with metallic screws by means of undistorted radiological imaging, uncompromised revision surgery, and minimized risk of graft laceration. However, one might consider that most currently available biodegradable interference screws do not show complete degradation and subsequent osseous replacement of the former implant site because they consist of slow degrading and high-molecular poly-L-lactide.27 Thus the use of intermediate degrading stereo-co-polymeric materials such as poly-(L-co-D,L-lactide) are preferable.27,30
The newest screw generations are sharply threaded just at the tip for easy starting conditions of the screw, followed by a blunt threading to prevent tissue laceration (see Fig. 39-2). Biodegradable as well as metallic interference screws are distributed in different sizes (diameter and length). Thus precise matching of graft and tunnel diameters can easily be performed.
Mechanical studies have shown that a tight fit among the screw, the graft, and the tunnel is essential for sufficient fixation strength.13,31–33 When deciding to oversize a screw to improve fixation strength (particularly at the tibial site), an increased length has been demonstrated to be superior to an increased diameter.13,34 Furthermore, an oversized screw diameter increases the insertion torque in contrast to a longer screw. We therefore recommend increasing screw length instead of using massively oversized screws in diameter (e.g., Delta screws) to avoid violating the tendon tissue.
In summary, hamstring tendon interference screw fixation offers the following advantages:
Technical Considerations
Graft Preparation
Because preservation of the gracilis tendon has been demonstrated to be beneficial35,36 and due to the fact that anatomical joint line fixation requires only a short graft (at least 7 cm) (Fig. 39-3), the use of a four-stranded semitendinosus tendon graft should be routinely achieved. To gain a sufficient length of the semitendinosus tendon, the tendon can be harvested including the periosteal distal insertion of the tendon. In most cases this results in a tendon length of at least 28 cm. If the semitendinosus tendon is very short (less than 26 cm) or thin, one can additionally harvest the gracilis tendon to create a four- or five-stranded semitendinosus/gracilis tendon graft.
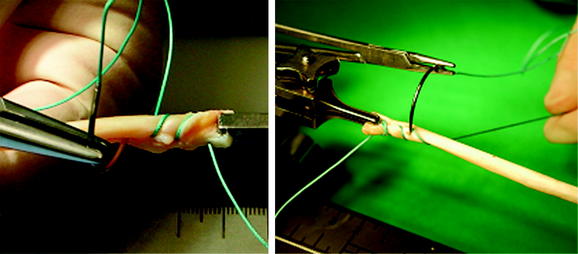
The four-stranded graft is prepared with the help of a suture board while arthroscopic preparation of the knee is performed. The proximal and distal endings of the semitendinosus tendon are armed with #2 polyester sutures in a whipstitch fashion (Fig. 39-4). Care has to be taken to pull all slack out of each suture pass. Then the construct should be manually tensioned to allow potential slippage to be taken out of the construct (Fig. 39-5). The tendon is then looped over itself using the so-called “W-technique,” and a polyester passing suture is brought through each loop (Fig. 39-6). The looped tendons are then pulled through a graft sizer (Fig. 39-7). The resulting diameter of the graft is usually between 7 and 9 mm. A tight fit of the graft in the tunnel generally is required to improve fixation strength and graft incorporation. The diameter of the graft is a given value, which needs to be known before tunnel creation. When hybrid fixation (see later discussion) is used, sizing of the graft in increments of 1 mm is sufficient; if interference screw fixation is used solely, we recommend sizing in increments of 0.5 mm33 to allow for the required tight fit. A marking suture using #0 absorbable suture has to be set 2 cm from the femoral end of the graft to show the surgeon if the graft is inserted deep enough into the femoral tunnel. The side effect of the suture is that good passage of the graft in the tunnel is ensured, and twisting of the graft around the screw during its insertion is prevented (see later discussion; see also Fig. 39-3).