Hair Growth Disorders: Introduction
|
Introduction
The importance of human hair in view of social communication and sexual attraction is enormous. Thus, diseases that lead to hair loss (alopecia), structural hair shaft defects or excessive hair growth on the body are often accompanied by diminished sense of personal well-being and self-esteem, leading to depressive moods and withdrawal from social interims.
In this chapter, we discuss the biologic basis and clinical presentation of hair growth disorders, give definitions (eTable 88-0.1), explain key management principles, and provide practical advice for diagnosis, therapy and patient management.
Effluvium: | Active process of hair shedding |
Alopecia: | Loss of hair, reduced hair density (scalp or body) |
Terminal hair: | Large hair follicle with a thick, medullated hair shaft >30 μm, roots are located in the subcutaneous fat |
Vellus hair: | Very small colorless non-medullated hair (<30 μm, roots are located in the upper dermis), only a few mm long. Vellus hairs can be found on the entire body except for palms and sols in different densities, depending on the body site. |
Vellus-like hair: | Hair that evolves from a former terminal hair follicle that had been miniaturized (due to androgenetic alopecia or alopecia areata), very small colorless hair (<30 μm, roots are located in the dermis), fibrous tissue (fibrous streamer) replaces the former terminal follicle below the root down to the subcutaneous fat |
Intermediate hair: | Hair in a transition stage from terminal to vellus-like due to a miniaturization process (∼50–30 μm, roots are located in the deeper dermis) |
Lanugo hair: | First hair produced in utero, pigmented, around 2–3 cm long, lanugo hairs are usually shed between week 32–36 of gestation but can be still present at birth in one third of children |
Hirsutism: | Growth of terminal hair on the body in a male distribution in women |
Hypertrichosis: | Increased growth of terminal hair or growth of lanugo hair on the body in an androgen-independent pattern |
Canities: | Graying of hair |
Canities subita: | Sudden (over night) graying of hair, appears in diffuse alopecia areata, when white hairs are spared by the inflammation and remain on the scalp while dark hair falls out very quickly |
Poliosis: | Localized white hair |
Cicatricial alopecia: | Irreversible hair loss, with loss of follicular ostia, and potentially skin atrophy |
Hair cycle: | Life-long cyclic transformation of hair follicles, which begins in utero |
Anagen: | Active growth phase, duration and growth rate depend on the body site (around 3–6 years on the scalp) |
Telogen: | Resting period, the hair shaft does not grow longer; duration depends on the body site (around 3 months on the scalp) |
Catagen: | Apoptosis driven regression phase between anagen and telogen |
Exogen: | Process of hair shaft shedding |
Anagen hair: | Hair with a pigmented root (except in white hair) and an inner root sheath (shows the form of a golf club when examined under the microscope) |
Telogen hair: | Club hair with a depigmented rounded proximal end |
Two frequently applied terms of alopecia and effluvium need to be characterized. While effluvium typifies the process of hair shedding, alopecia characterizes the final result of this. Both terms are nonspecific; they do not give etiological information of the underlying hair loss (see eTable 88-0.1).
Disorders that result in alopecia can be grouped into diffuse, patterned and focal hair loss as well as into scarring (synonym: cicatricial) and nonscarring forms. Scarring forms are characterized by permanent destruction of hair follicular stem cell structure resulting in loss of hair producing capabilities. In contrast, in nonscarring alopecia the hair follicle is not ultimately destroyed and subsequent hair regrowth follows periods of hair shedding. In both, scarring and non scarring alopecia, distribution of hair loss can occur in a diffuse pattern over the whole scalp or be circumscribed, affecting only a few, more or less demarcated areas. Alopecia can also be due to improper or missing follicle development. These rare inherited hair abnormalities can be focal (e.g., aplasia cutis congenita, see Chapter 107) or diffuse (e.g., ectodermal dysplasia, see Chapter 142).
Hair growth disorders caused by structural hair shaft defects can be acquired or inherited. While acquired hair shaft defect are accompanied by increased hair breakage and are usually due to hair grooming practices, inherited hair shaft defects can be grouped into disorders with or without increased hair breakage. Acquired hair shaft disorders are reversible when trigger factors are stopped. Inherited hair shaft disorders cannot be cured, but tend to improve as the patient ages.
Principles of Hair Follicle Biology
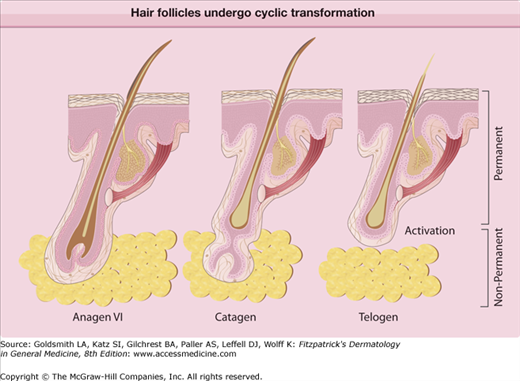
![]() Hair follicles are remarkably productive organs that undergo constant tissue remodeling. During its cyclic transformation, the hair follicle changes from a phase of rapid growth (anagen) to a resting period (telogen) via apoptosis-driven regression (catagen) (eFig. 88-0.1). Anagen is the phase of massive and rapid tissue transformation of the lower follicle. It can be divided in seven stages: (1) growth of the dermal papilla and onset of mitotic activity in the overlying epithelial cells; (2) envelopment of the dermal papilla by bulb matrix cells and early differentiation; (3) full differentiation of bulb matrix cells into all follicular components; (4) reactivation of matrix melanocytes; (5) emergence of the hair shaft and dislodging of the old telogen hair in the dermis; (6) emergence of the new hair shaft from the skin surface; and (7) stable growth.
Hair follicles are remarkably productive organs that undergo constant tissue remodeling. During its cyclic transformation, the hair follicle changes from a phase of rapid growth (anagen) to a resting period (telogen) via apoptosis-driven regression (catagen) (eFig. 88-0.1). Anagen is the phase of massive and rapid tissue transformation of the lower follicle. It can be divided in seven stages: (1) growth of the dermal papilla and onset of mitotic activity in the overlying epithelial cells; (2) envelopment of the dermal papilla by bulb matrix cells and early differentiation; (3) full differentiation of bulb matrix cells into all follicular components; (4) reactivation of matrix melanocytes; (5) emergence of the hair shaft and dislodging of the old telogen hair in the dermis; (6) emergence of the new hair shaft from the skin surface; and (7) stable growth.
![]() The length of the anagen phase varies depending on the body site. Terminal hairs on the scalp show an anagen phase of approximately 3–6 years.1 Catagen is marked by an extensive destruction of the lower follicle. Matrix and lower outer root sheath cell stop proliferating abruptly and undergo apoptosis. Melanocytes stop producing pigment before the matrix cell proliferation stops, which leads to an unpigmented proximal end of the telogen hair. This transitional period lasts 2–4 weeks. Once the involution of catagen is complete and a club hair is formed, the follicle has entered telogen and has lost one third of its original length. The dermal papilla has disintegrated, except for a few cells; the inner root sheath is gone. The distal outer root sheath closes around the fully keratinized hair shaft. The telogen phase of terminal scalp hair lasts around 3 months on the scalp. It is followed by the shedding of the hair shaft, called exogen.2,3 Normally up to 90% of the hair follicles are in anagen while, around 10% are in telogen and 1%–2% in catagen.
The length of the anagen phase varies depending on the body site. Terminal hairs on the scalp show an anagen phase of approximately 3–6 years.1 Catagen is marked by an extensive destruction of the lower follicle. Matrix and lower outer root sheath cell stop proliferating abruptly and undergo apoptosis. Melanocytes stop producing pigment before the matrix cell proliferation stops, which leads to an unpigmented proximal end of the telogen hair. This transitional period lasts 2–4 weeks. Once the involution of catagen is complete and a club hair is formed, the follicle has entered telogen and has lost one third of its original length. The dermal papilla has disintegrated, except for a few cells; the inner root sheath is gone. The distal outer root sheath closes around the fully keratinized hair shaft. The telogen phase of terminal scalp hair lasts around 3 months on the scalp. It is followed by the shedding of the hair shaft, called exogen.2,3 Normally up to 90% of the hair follicles are in anagen while, around 10% are in telogen and 1%–2% in catagen.
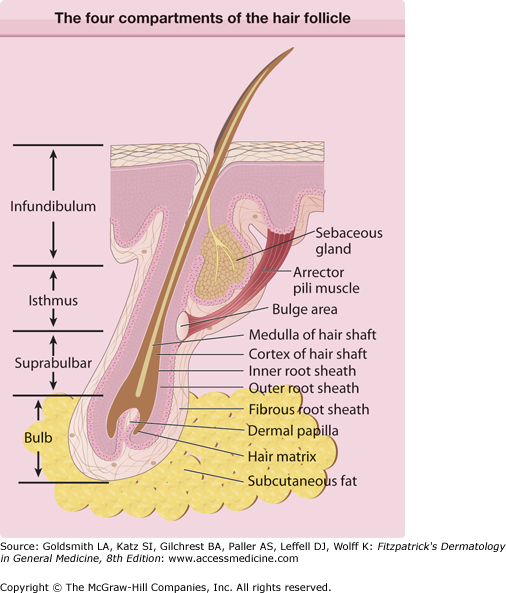
![]() A hair follicle can functionally and anatomically be divided in four compartments: (1) infundibulum, (2) isthmus, (3) suprabulbar, and (4) bulb region (eFig. 88-0.2). The infundibulum extends from the epidermis to the opening of the excretory duct of the sebaceous gland. The epithelium of the infundibulum is continuous with the epidermis and shows a similar appearance; its cells seem to have a higher proliferative capacity and they can regenerate the epidermis after wounding or injury. The infundibulum is formed like a funnel; its lumen normally contains the hair shaft, keratin material and sebum, and sometimes, apocrine secretion (pubic hair), lipophilic yeast, and Demodex mites (sebaceous follicles on the face).
A hair follicle can functionally and anatomically be divided in four compartments: (1) infundibulum, (2) isthmus, (3) suprabulbar, and (4) bulb region (eFig. 88-0.2). The infundibulum extends from the epidermis to the opening of the excretory duct of the sebaceous gland. The epithelium of the infundibulum is continuous with the epidermis and shows a similar appearance; its cells seem to have a higher proliferative capacity and they can regenerate the epidermis after wounding or injury. The infundibulum is formed like a funnel; its lumen normally contains the hair shaft, keratin material and sebum, and sometimes, apocrine secretion (pubic hair), lipophilic yeast, and Demodex mites (sebaceous follicles on the face).
![]() The isthmus extends from the opening of the sebaceous duct to the insertion of the arrector pili muscle. The outer root sheath of the isthmus, in contrast to the interfollicular epidermis, has no granular layer and its cells contain an increased amount of glycogen. Above the insertion of the arrector pili muscle, the inner root sheath of a growing (anagen) hair follicle disintegrates. From this point to the opening of the sebaceous gland, the outer root sheath shows a special type of keratinization, called trichilemmal keratinization. Cysts that arise from this area are called trichilemmal cysts.4 The inferior part of the isthmus, at the point of the insertion of the arrector pili muscle, is called the bulge are. The bulge is composed of biochemically distinctive keratinocytes that posses the characteristics of epithelial stem cells.1,5
The isthmus extends from the opening of the sebaceous duct to the insertion of the arrector pili muscle. The outer root sheath of the isthmus, in contrast to the interfollicular epidermis, has no granular layer and its cells contain an increased amount of glycogen. Above the insertion of the arrector pili muscle, the inner root sheath of a growing (anagen) hair follicle disintegrates. From this point to the opening of the sebaceous gland, the outer root sheath shows a special type of keratinization, called trichilemmal keratinization. Cysts that arise from this area are called trichilemmal cysts.4 The inferior part of the isthmus, at the point of the insertion of the arrector pili muscle, is called the bulge are. The bulge is composed of biochemically distinctive keratinocytes that posses the characteristics of epithelial stem cells.1,5
![]() The suprabulbar region undergoes dramatic changes during hair cycling. It extends from the bulge area to the hair bulb. In growing hair follicles (anagen) it is comprised of three layers: (1) the outer root sheath, (2) inner root sheath, and (3) hair shaft. The inner root sheath is fully keratinized and its innermost cuticle cells interlock with the cuticle cells of the hair shaft, which therefore is tightly anchored in the skin during anagen.
The suprabulbar region undergoes dramatic changes during hair cycling. It extends from the bulge area to the hair bulb. In growing hair follicles (anagen) it is comprised of three layers: (1) the outer root sheath, (2) inner root sheath, and (3) hair shaft. The inner root sheath is fully keratinized and its innermost cuticle cells interlock with the cuticle cells of the hair shaft, which therefore is tightly anchored in the skin during anagen.
![]() The bulb is the deep, bulbous portion of the follicle that surrounds the dermal papilla. The bulb contains the matrix keratinocytes, which rapidly proliferate to generate the hair shaft. This rate of proliferation is one of the highest of any tissue in the body. Therefore, it is not surprising that these epithelial cells are exquisitely vulnerable and sensitive to any kind of internal and external influences like stress, drugs, hormones and immunologic or physical injury.6–8
The bulb is the deep, bulbous portion of the follicle that surrounds the dermal papilla. The bulb contains the matrix keratinocytes, which rapidly proliferate to generate the hair shaft. This rate of proliferation is one of the highest of any tissue in the body. Therefore, it is not surprising that these epithelial cells are exquisitely vulnerable and sensitive to any kind of internal and external influences like stress, drugs, hormones and immunologic or physical injury.6–8
![]() Hair matrix keratinocytes undergo terminal differentiation while being infused with melanin granules produced by specialized melanocytes of the hair follicle pigmentary unit.9,10 Two different types of melanin can be distinguished: (1) eumelanin, which is brown or black, and (2) pheomelanin, which is yellow or red.11–15 Differences in hair color are not a result of the number of melanocytes. Rather, they are largely the result of differences in the amount and types of melanin produced and the macromolecular structure and packaging of melanin.13,14 Furthermore, hair color may vary both in time and site. For example, scalp hair may be blonde in childhood and become brown or black in adolescence, before becoming white again in middle or old age; beard or pubic hair may be red and the scalp hair black or dark brown in the same individual.12,14,16
Hair matrix keratinocytes undergo terminal differentiation while being infused with melanin granules produced by specialized melanocytes of the hair follicle pigmentary unit.9,10 Two different types of melanin can be distinguished: (1) eumelanin, which is brown or black, and (2) pheomelanin, which is yellow or red.11–15 Differences in hair color are not a result of the number of melanocytes. Rather, they are largely the result of differences in the amount and types of melanin produced and the macromolecular structure and packaging of melanin.13,14 Furthermore, hair color may vary both in time and site. For example, scalp hair may be blonde in childhood and become brown or black in adolescence, before becoming white again in middle or old age; beard or pubic hair may be red and the scalp hair black or dark brown in the same individual.12,14,16
![]() Hair follicle formation starts in utero during the 12th and 15th week of pregnancy. By week 22, hair follicle formation is completed and the fetus is covered with downy, lightly pigmented, nonmedullated hair, called lanugo hair, which grows up to a length of 2–3 cm. This hair shows a synchronous hair cycle and grows in two phases. The first lanugo hair is shed in the 7th–8th month of pregnancy, the second set of lanugo hair is shed by the time of birth up to 3 months of age.2 After that, hair follicles produce fine, nonmedullated vellus hair that only grows a few mm long. After lanugo hairs are shed, the growth cycle is asynchronous, meaning that each follicle develops its own cycle and the hair does not fall out at the same time. Hair follicles on the scalp produce a pigmented, thicker, longer hair type, which is not fully medullated at the time of birth. By age 2, thick, completely medullated terminal hairs replace these hairs.2 Terminal hair on the scalp shows an anagen phase of around 3–6 years. Not every hair follicle on the scalp produces terminal hairs. The ratio of terminal to vellus hair (T:V) ranges from 1.7:1 to 6.0:1.17,18
Hair follicle formation starts in utero during the 12th and 15th week of pregnancy. By week 22, hair follicle formation is completed and the fetus is covered with downy, lightly pigmented, nonmedullated hair, called lanugo hair, which grows up to a length of 2–3 cm. This hair shows a synchronous hair cycle and grows in two phases. The first lanugo hair is shed in the 7th–8th month of pregnancy, the second set of lanugo hair is shed by the time of birth up to 3 months of age.2 After that, hair follicles produce fine, nonmedullated vellus hair that only grows a few mm long. After lanugo hairs are shed, the growth cycle is asynchronous, meaning that each follicle develops its own cycle and the hair does not fall out at the same time. Hair follicles on the scalp produce a pigmented, thicker, longer hair type, which is not fully medullated at the time of birth. By age 2, thick, completely medullated terminal hairs replace these hairs.2 Terminal hair on the scalp shows an anagen phase of around 3–6 years. Not every hair follicle on the scalp produces terminal hairs. The ratio of terminal to vellus hair (T:V) ranges from 1.7:1 to 6.0:1.17,18
![]() A normal scalp contains approximately 100,000 terminal hairs. Hair density and hair shaft thickness varies depending on ethnicity. The term Caucasian or Indo-European comprised a vast diversity of different ethnic subgroups originating from Europe, North Africa and western (as well as south and middle) Asia. Therefore this group shows a tremendous variability in hair shaft shape and caliber. In general, Caucasian hair has a slightly flattened or oval cross section with a diameter ranging from 50 to 90 μm.15,19 In Europeans, hair shaft diameters can range from approximately 50–120 μm. Blondes tend to have more hair (∼120,000), and redheads less (∼80,000).20–23 The term African hair refers to hair of people who live in Africa or people who trace their ancestry to indigenous inhabitants of Africa (in particular Sub-Saharan Africa). This includes people who were displaced in the African diaspora resulting from the Atlantic Slave Trade such as African-Americans, African-Canadians, Afro-Latin Americans, Afro-Caribbeans, and black British. African hair is highly characteristic in shape. African hair is less dense compared to Caucasian hair considerably flattened, grooved and frequently vary in diameter along one single shaft. It tends to be highly twisted, with random reversal in twist direction. Hair of people originating from East Asia (China, Korea, and Japan) is usually referred to as Oriental or Asian hair. It generally shows a lower density and a greater diameter, ranging from 100 to 130 μm.23,24
A normal scalp contains approximately 100,000 terminal hairs. Hair density and hair shaft thickness varies depending on ethnicity. The term Caucasian or Indo-European comprised a vast diversity of different ethnic subgroups originating from Europe, North Africa and western (as well as south and middle) Asia. Therefore this group shows a tremendous variability in hair shaft shape and caliber. In general, Caucasian hair has a slightly flattened or oval cross section with a diameter ranging from 50 to 90 μm.15,19 In Europeans, hair shaft diameters can range from approximately 50–120 μm. Blondes tend to have more hair (∼120,000), and redheads less (∼80,000).20–23 The term African hair refers to hair of people who live in Africa or people who trace their ancestry to indigenous inhabitants of Africa (in particular Sub-Saharan Africa). This includes people who were displaced in the African diaspora resulting from the Atlantic Slave Trade such as African-Americans, African-Canadians, Afro-Latin Americans, Afro-Caribbeans, and black British. African hair is highly characteristic in shape. African hair is less dense compared to Caucasian hair considerably flattened, grooved and frequently vary in diameter along one single shaft. It tends to be highly twisted, with random reversal in twist direction. Hair of people originating from East Asia (China, Korea, and Japan) is usually referred to as Oriental or Asian hair. It generally shows a lower density and a greater diameter, ranging from 100 to 130 μm.23,24
![]() The hair shaft has numerous functions such as UV-protection, isolation, sensation, and dispersion of skin secretions. Among these, its function as an instrument of psychological, social and sexual communication is the predominant one in human civilization. Therefore, it is not surprising that major, widely visible loss or ungainly growth of these instruments of communication is distressing, can shatter self-esteem, and can cause withdrawal and depression.25,26
The hair shaft has numerous functions such as UV-protection, isolation, sensation, and dispersion of skin secretions. Among these, its function as an instrument of psychological, social and sexual communication is the predominant one in human civilization. Therefore, it is not surprising that major, widely visible loss or ungainly growth of these instruments of communication is distressing, can shatter self-esteem, and can cause withdrawal and depression.25,26
Diagnostic Techniques for Evaluating Hair Growth Disorders
A thorough patient history is critical for the development of an initial differential diagnosis and for the relationship with the patient. The patient should be asked about the duration and pattern of the hair problem. Was the problem present at birth, did it evolve gradually over time starting at a certain age or was there a rapid onset? A hair problem that is present at birth leads more to a genetic disorder; certain conditions are more common in children, such as tinea capitis, alopecia areata, or trichotillomania. For example, a rapid onset of hirsutism can lead to the diagnosis of an androgen-secreting tumor. A gradual thinning of fronto-parietal scalp hair fits more to the diagnosis of androgenetic alopecia (AGA) (see eTable 88-0.2). Patients with hair loss should be asked if the hair is shedding or thinning and if the hair is coming out “by the root” or if it is breaking off. A patient history includes the family history as well as questions about current and past medication, pregnancy, menses, menopause, thyroid function, diet, past and present health, surgeries, accidents, physical or emotional stress events and hair care practices.
Pathogenetic Principle | Clinical Effect (Examples) |
|---|---|
Disturbed hair follicle cycling | Effluvium (telogen effluvium, alopecia areata, androgenetic alopecia, chemotherapy-induced alopecia) |
Unwanted hair follicle transformation | Patterned hair loss (androgenetic alopecia) Hirsutism Hypertrichosis |
Defective hair follicle regeneration | Cicatricial alopecia (lichen planopilaris, traction alopecia, radiation-induced alopecia, folliculitis decalvans, chronic discoid lupus erythematosus) |
Structural hair shaft defect | Hair shaft disorders (monilethrix, pili torti, trichothiodystrophy) |
Improper/missing hair follicle development | Aplasia cutis congenita Ectodermal dysplasias |
Combinations of the above |
The global examination of the scalp should first of all assess the overall pattern of the hair problem. It is important to determine density and distribution and if the hair loss is focal or global. Furthermore, the presence of scaling, erythema, erosions, crust or pustules and the presences or absence of follicular ostia should be noted. The clinical examination should also involve the nails, since some disorders, for example alopecia areata, lichen planopilaris (LPP), or ectodermal dysplasia can also affect finger and toe nails. Excessive body hair is oftentimes shaved or epilated. The extent of unwanted terminal hair growth can be evaluated by a patient self-assessment with the help of images (see Section “Hirsutism”).
The pull test is a useful ancillary, qualitative test for the assessment of the ongoing activity of hair loss. The examiner grasps approximately 50–60 hairs and tugs at them from proximal to distal end. Removal of six hairs indicates a positive pull test and active shedding. However, the test can be considered positive if three hairs can be pulled out in several different areas of the scalp. The proximal ends can be examined against a white (for dark hair) or black (for light hair) background. A blunt tip indicates hair breakage; a tapered tip can indicate regrowth or miniaturized hairs. The proximal end of the hair shafts may also be examined with a light microscope to determine, if the hairs break off (blunt ends) or came out as club hairs (telogen hair).
A scalp biopsy is necessary, particularly when confirming the diagnosis of scarring alopecia. A scalp biopsy should also be considered for the differential diagnosis of TE, diffuse alopecia areata and AGA. The following recommendations were developed at the consensus meeting on cicatricial alopecia in February 2001: one 4-mm punch biopsy including subcutaneous tissue should be taken from a clinically active area, processed for horizontal sections and stained with hematoxylin and eosin. Elastin (acid alcoholic orcein), mucin, and periodic acid-Schiff (PAS) stains may provide additional information. A second 4-mm punch biopsy from a clinically active disease affected area should be cut vertically into two equal pieces. One-half provides tissue for transversely cut routine histological sections; the other half can be used for direct immunofluorescence (DIF) studies.1,27 Usually only one biopsy from the affected area is necessary for the diagnosis of a nonscarring alopecia; the samples are preferably processed with horizontal sections.
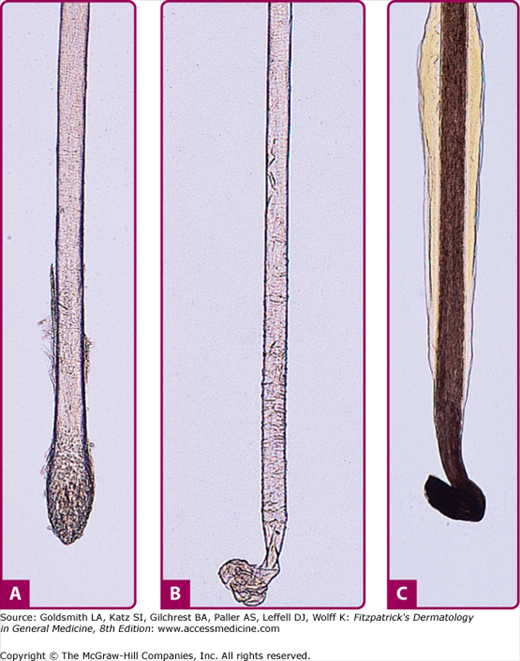
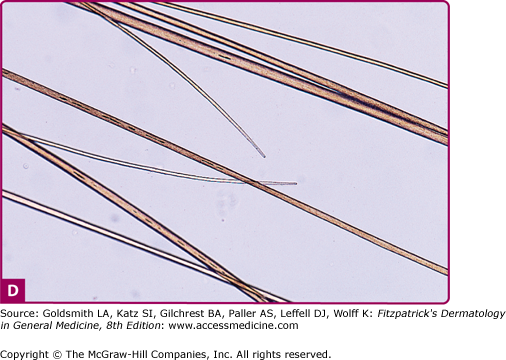
This technique is a simple method of quantifying hair loss by comparing the proportion of anagen to catagen and telogen hairs. For accurate measurement, patients should avoid washing their hair 3–4 days prior the test. Also perms, dyes, or straightening of hair can alter results and have to be avoided at least 6 weeks prior. A group of about 25–50 hairs should be grasped with a needle holder close to the scalp and plucked sharply in the direction of the hair. The proximal ends of the hair shafts are place on a glass slide in a drop of water and covered with a cover slip. Alternatively, a solution of 1% dimethylcinnamaldehyde in 0.5 N hydrochloric acid can be used, which stains the anagen hairs red due to the presence of protein bound citrulline in the inner root sheath. The roots are than examined by light microscopy with 100-fold magnification. Ten to twenty percent of telogen hair can be regarded as normal (the percentage of anagen hairs is slightly higher in women and children compared to men); a telogen count over 35% is highly suspicious for a TE. By repeating the trichogram over a time period, a hair loss condition can be followed and treatment results can be measured28 (Fig. 88-1).
Figure 88-1
A. Telogen club hairs have a cornified, depigmented, rounded-up bulb without an attached root sheath. B. Loose anagen hair obtained by hair pull: Ruffled cuticle and no attached root sheath. Anagen hairs are recognized clinically by their pigmented, somewhat distorted, malleable bulb. Anagen hairs should not normally be found in a hair pull in patients with alopecia areata. C. Comparison with a normal anagen hair obtained by hair pluck. D. A newly growing anagen hair has a tapered distal tip rather than the blunt distal end of hairs that have been cut or trimmed or ends that are intrinsically broken. (From Ralf Paus, Elise A. Olsen, Andrew G. Messenger: Fitzpatrick’s Dermatology in General Medicine. 7th ed. Copyright © The McGraw-Hill Companies, Inc. All rights reserved, with permission.)
Investigation of plucked hairs for spores allows establishing the diagnosis of tinea capitis. In this case the hair should be mounted in 5% potassium hydroxide and gently heated.
![]() One of the earliest noninvasive techniques of measuring hair density was devised by Bouhanna, who used camera attachments to create a “phototrichogram,” an ultra close-up photograph of hair exiting the scalp. The technique was later combined with digital image analysis.28–32 A phototrichogram involves clipping of hair to a defined length in one or two areas of the scalp. After 3 days, the scalp areas are usually dyed with black hair dye and a close up picture is taken. With the help of digital imaging it is now possible to determine, the percentage of growing (anagen) hair and the hair density per cm2.
One of the earliest noninvasive techniques of measuring hair density was devised by Bouhanna, who used camera attachments to create a “phototrichogram,” an ultra close-up photograph of hair exiting the scalp. The technique was later combined with digital image analysis.28–32 A phototrichogram involves clipping of hair to a defined length in one or two areas of the scalp. After 3 days, the scalp areas are usually dyed with black hair dye and a close up picture is taken. With the help of digital imaging it is now possible to determine, the percentage of growing (anagen) hair and the hair density per cm2.
![]() A more modern noninvasive technique to measure scalp hair density is videodermoscopy.33,34 Videodermoscopy allows evaluating the scalp in 20–100-fold magnification, hair and scalp disorders can be easily diagnosed and when combined with digital image analysis it allows to measure hair density and thickness of the hair shaft without shaving, clipping or dyeing (Table 88-1 and eTable 88-1.1).
A more modern noninvasive technique to measure scalp hair density is videodermoscopy.33,34 Videodermoscopy allows evaluating the scalp in 20–100-fold magnification, hair and scalp disorders can be easily diagnosed and when combined with digital image analysis it allows to measure hair density and thickness of the hair shaft without shaving, clipping or dyeing (Table 88-1 and eTable 88-1.1).
|
|
Androgenetic Alopecia
AGA or pattern hair loss is by far the most common type of hair loss in men and women. Male pattern hair loss (MPHL) (also known as male AGA, male balding) is an androgen-dependent, genetically determined trait. Female pattern hair loss (FPHL) (or female androgenetic alopecia) is believed to be the same entity. However, the requirement of androgens is less clear-cut than in men and the distribution of hair loss is generally different.35,36 In both, men and women, AGA is characterized by a progressive decline in the duration of anagen, an increase in the duration of telogen and miniaturization of scalp hair follicles.
|
Epidemiology
Estimates of the prevalence of AGA vary widely. Most men will develop some degree of recession of the hairline during their lifetime. A progression to at least type III (see Fig. 88-2) is seen in around 50% of men and women beyond 40 years of age.37–40,41 The risk of male pattern baldness depends on the family history in the father, the mother, or the maternal grandfather.42,43 Men whose father had hair loss were twice as likely to have hair loss as men whose father showed no hair loss.
Ethnic variation in the incidence of AGA has been reported. AGA seems to be four times less frequent in men of African ancestry,44 around three times less frequent in Korean men45 and approximately 1.5 times less frequent in men originating form China, Japan or Thailand.46,47
FPHL is less common than MPHL but shows a similar age-related increase in frequency and severity. However, the condition can start as early as the prepubertal period both in men and women (Fig. 88-3). Around 40% of Caucasian women have developed some degree of FPHL at age 70.35,48 FPHL seems to be less frequent in Asian women.45
Etiology and Pathogenesis
The underlying causes of patterned hair loss have yet to be determined. In men, MPHL appears to result from a combination of androgen hyperactivity, a genetic predisposition to hair loss-related sensitivity to androgen action as well as an androgen-independent genetic predisposition. For females, the condition known as female pattern hair loss (FPHL) may have a more complex etiology. However, androgen action combined with genetic sensitivity to those actions seems to play a dominant role in most cases, and indeed these factors may be present generally in FPHL.
In AGA, large, pigmented hairs, called terminal hairs, are gradually replaced by fine (nearly invisible) colorless vellus hairs.1,39 This transformation follows a progressive course with each hair cycle in the following manner. Scalp hair develops in three phases40,49: (1) a growth phase, or anagen, of approximately 2–6 years; (2) a short (2–3 weeks) phase, catagen, which actually represents the termination of anagen; and (3) transition to the telogen phase. A telogen hair does not grow and is shed from the follicle after about 12 weeks. The transition to catagen results in decreased levels of anagen-maintaining cytokines within the hair follicle. MPHL and FPHL exhibit a progressive decrease in anagen duration with each cycle, producing shorter, thinner hairs.38 Finally, the interval between late telogen hair shedding (exogen) and new hair growth with initiation of anagen increases, resulting in more follicles without hair and an apparent reduction in scalp hair density.37
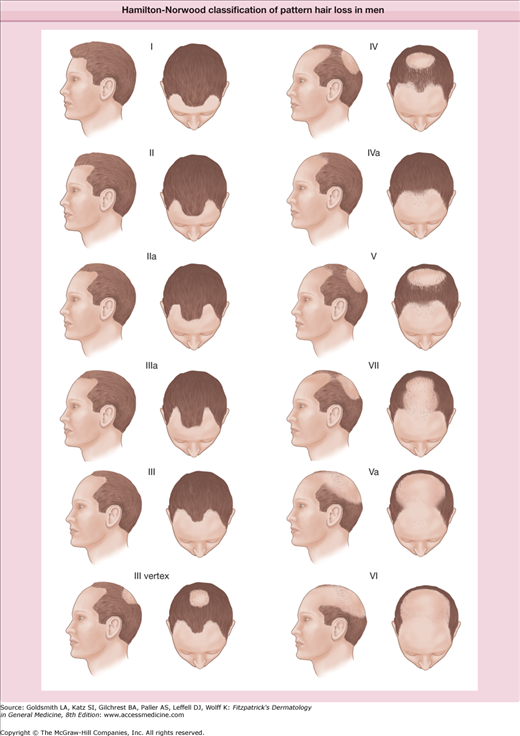
![]() The dependence of MPHL on male sex hormones has been considered since ancient times. Egyptian texts discussed the matter in social terms and also provided herbal remedies for its treatment. Greek authors Hippocrates and Aristotle observed the absence of baldness in eunuchs, although of course they were not able to evoke the relevant endocrine physiology. Testosterone was first identified in the scientific literature as a causal factor for MPHL by James Hamilton in 1942.50 This anatomist was able to observe intact hairlines in males castrated before puberty, and cessations of hairline recession in those castrated after puberty. Administration of testosterone to castrati was seen to induce hair loss that was arrested, but not reversed, when testosterone was no longer given. These observations suggest that normal physiological levels of circulating androgens and/or androgen precursors are necessary for producing MPHL in certain predisposed individuals, with genetics being the likely factor for predisposition. The same author also proposed a seven-stage classification system, termed the Norwood–Hamilton scale after modifications by the former in 1974 that ranked hair loss patterns by severity of hairline recession. It is worth noting that since this time attempts to connect levels of testosterone with baldness have not produced positive correlations.51,52
The dependence of MPHL on male sex hormones has been considered since ancient times. Egyptian texts discussed the matter in social terms and also provided herbal remedies for its treatment. Greek authors Hippocrates and Aristotle observed the absence of baldness in eunuchs, although of course they were not able to evoke the relevant endocrine physiology. Testosterone was first identified in the scientific literature as a causal factor for MPHL by James Hamilton in 1942.50 This anatomist was able to observe intact hairlines in males castrated before puberty, and cessations of hairline recession in those castrated after puberty. Administration of testosterone to castrati was seen to induce hair loss that was arrested, but not reversed, when testosterone was no longer given. These observations suggest that normal physiological levels of circulating androgens and/or androgen precursors are necessary for producing MPHL in certain predisposed individuals, with genetics being the likely factor for predisposition. The same author also proposed a seven-stage classification system, termed the Norwood–Hamilton scale after modifications by the former in 1974 that ranked hair loss patterns by severity of hairline recession. It is worth noting that since this time attempts to connect levels of testosterone with baldness have not produced positive correlations.51,52
![]() Testosterone is the major circulating hormone, synthesized in the gonads from the weaker androgens dihydroepiandrosterone sulfate and androsterone, which are produced in the adrenal glands. However, 5α-dihydroxytestosterone (DHT) is thought to be the principal agent causing MPHL. DHT is made by the action of 5α-reductase on testosterone, bind five times more potently to the androgen receptors (ARs),49,53 and is localized around hair follicles.54 Balding scalp has been shown to contain higher levels of 5α-reductase as well as DHT when compared to nonbalding scalp.55,56 Also, men born with a genetic deficiency of one of the isoforms (type II) of 5α-reductase exhibit type II pseudohermaphroditism but do not develop AGA; their circulating T levels are normal or slightly higher but DHT levels are suppressed.57,58 Finally, an irreversible inhibitor of 5α-reductase, the synthetic azo-steroid finasteride, as well as its close pharmacological relative dutasteride, potently reduce DHT concentrations in scalp and serum59 and are an efficacious treatments for AGA.27
Testosterone is the major circulating hormone, synthesized in the gonads from the weaker androgens dihydroepiandrosterone sulfate and androsterone, which are produced in the adrenal glands. However, 5α-dihydroxytestosterone (DHT) is thought to be the principal agent causing MPHL. DHT is made by the action of 5α-reductase on testosterone, bind five times more potently to the androgen receptors (ARs),49,53 and is localized around hair follicles.54 Balding scalp has been shown to contain higher levels of 5α-reductase as well as DHT when compared to nonbalding scalp.55,56 Also, men born with a genetic deficiency of one of the isoforms (type II) of 5α-reductase exhibit type II pseudohermaphroditism but do not develop AGA; their circulating T levels are normal or slightly higher but DHT levels are suppressed.57,58 Finally, an irreversible inhibitor of 5α-reductase, the synthetic azo-steroid finasteride, as well as its close pharmacological relative dutasteride, potently reduce DHT concentrations in scalp and serum59 and are an efficacious treatments for AGA.27
![]() Androgens generate cellular responses by diffusing through the outer membrane and binding to the intracellular-located AR. The bound hormone-receptor complex diffuses through the nuclear membrane and ligates to promoter DNA sequences of androgen-regulated genes, altering expression of these genes and hence affecting cellular metabolism. Depending on the site on the skin, the result may be enhancement or suppression of hair growth; the latter may occur through androgen-induced apoptosis in dermal papilla cells. As well, sensitivity to androgen signaling is regulated through AR activation. Genetically male individuals lacking a functional AR do not develop masculine characteristics such as male genital development and body hair growth, including the beard. MPHL is also not observed in those persons with a functional AR lack, such as in a mutation in the AR gene27; all this is in spite of normal or even elevated circulating androgen levels. Conversely, balding scalp has been demonstrated to exhibit enhanced AR expression compared to nonbalding scalp.55,60
Androgens generate cellular responses by diffusing through the outer membrane and binding to the intracellular-located AR. The bound hormone-receptor complex diffuses through the nuclear membrane and ligates to promoter DNA sequences of androgen-regulated genes, altering expression of these genes and hence affecting cellular metabolism. Depending on the site on the skin, the result may be enhancement or suppression of hair growth; the latter may occur through androgen-induced apoptosis in dermal papilla cells. As well, sensitivity to androgen signaling is regulated through AR activation. Genetically male individuals lacking a functional AR do not develop masculine characteristics such as male genital development and body hair growth, including the beard. MPHL is also not observed in those persons with a functional AR lack, such as in a mutation in the AR gene27; all this is in spite of normal or even elevated circulating androgen levels. Conversely, balding scalp has been demonstrated to exhibit enhanced AR expression compared to nonbalding scalp.55,60
![]() The role of androgen hypersecretion, in situ enzyme activity and ARs in FPHL is still not completely understood. Androgens in women come from 3 different sources: (1) the adrenal gland, usually as a byproduct of cortisol biosynthesis (zona fasciculata), and not so much from the zona reticularis, since these cells seem to be only mature during puberty61; (2) the ovaries and (3) the peripheral compartment. The skin, especially the pilosebaceous unit composed of sebaceous gland and hair follicle, can synthesize androgens either de novo from cholesterol or by local conversion of circulating weaker androgens to more potent ones.62 Six enzymes are involved in androgen metabolism in the skin. These are: (1) steroid sulfatase; (2) 3β-hydroxysteroid dehydrogenase/Δ5–4-isomerase (Δ5–3βHSD); (3) 17β-hydroxysteroid dehydrogenase (17βHSD); (4) 5α-reductase; (5) 3α-hydroxysteroid dehydrogenase (3α-HSD); and (6) aromatase. Steroid sulfatase metabolizes dehydroepiandrostenone sulfate (DHEA-S) to dehydroepiandrostenone (DHEA). Isoenzyme I of Δ5–3βHSD converts DHEA to androstenedione in human skin and is mainly located in the sebaceous glands62; androstenedione can be activated by 17βHSD to T. Eight isoforms of 17βHSD are known.62 In hair follicles 17βHSD is found in the outer root sheath cells. 5α-reductase irreversibly converts T to DHT, the most potent naturally occurring androgen in the skin. Isoenzyme I can predominately be found in the sebaceous gland, while isoenzyme II occurs in the hair follicle epithelium.62 3α-HSD exists in 3 isoforms. It catabolizes active androgens to compounds that do not bind the intracellular AR,62 such as 3α-androstanediol. Aromatase is localized in the inner and outer root sheath as well as in the sebaceous gland. It can convert testosterone and androstenedione to estradiol and estrone55 and may play a “detoxifying” role by removing excess androgens.62 It has been shown that the concentration of aromatase is five times higher in female scalp skin, compared to male scalp skin.55 These findings could explain the differences in male and female patterns of balding and the sparing of the frontal hairline.
The role of androgen hypersecretion, in situ enzyme activity and ARs in FPHL is still not completely understood. Androgens in women come from 3 different sources: (1) the adrenal gland, usually as a byproduct of cortisol biosynthesis (zona fasciculata), and not so much from the zona reticularis, since these cells seem to be only mature during puberty61; (2) the ovaries and (3) the peripheral compartment. The skin, especially the pilosebaceous unit composed of sebaceous gland and hair follicle, can synthesize androgens either de novo from cholesterol or by local conversion of circulating weaker androgens to more potent ones.62 Six enzymes are involved in androgen metabolism in the skin. These are: (1) steroid sulfatase; (2) 3β-hydroxysteroid dehydrogenase/Δ5–4-isomerase (Δ5–3βHSD); (3) 17β-hydroxysteroid dehydrogenase (17βHSD); (4) 5α-reductase; (5) 3α-hydroxysteroid dehydrogenase (3α-HSD); and (6) aromatase. Steroid sulfatase metabolizes dehydroepiandrostenone sulfate (DHEA-S) to dehydroepiandrostenone (DHEA). Isoenzyme I of Δ5–3βHSD converts DHEA to androstenedione in human skin and is mainly located in the sebaceous glands62; androstenedione can be activated by 17βHSD to T. Eight isoforms of 17βHSD are known.62 In hair follicles 17βHSD is found in the outer root sheath cells. 5α-reductase irreversibly converts T to DHT, the most potent naturally occurring androgen in the skin. Isoenzyme I can predominately be found in the sebaceous gland, while isoenzyme II occurs in the hair follicle epithelium.62 3α-HSD exists in 3 isoforms. It catabolizes active androgens to compounds that do not bind the intracellular AR,62 such as 3α-androstanediol. Aromatase is localized in the inner and outer root sheath as well as in the sebaceous gland. It can convert testosterone and androstenedione to estradiol and estrone55 and may play a “detoxifying” role by removing excess androgens.62 It has been shown that the concentration of aromatase is five times higher in female scalp skin, compared to male scalp skin.55 These findings could explain the differences in male and female patterns of balding and the sparing of the frontal hairline.
![]() Sex hormone-binding globulin (SHBG) is the main transport protein for circulating T and estradiol. SHBG is produced in liver cells and to some degree in the brain, uterus, placenta and vagina. SHBG levels are regulated by a delicate balance of inhibiting and enhancing factors. High androgen levels decrease the production of SHBG, whereas estrogen and thyroxine increase SHBG. As well, insulin-like growth factor-1 (IGF-1) can suppress SHBG. Only unbound testosterone and estradiol are biologically active; hence, the lower the SHBG blood levels, the higher the bioavailability of these androgens. Conditions characterized by low SHBG levels include polycystic ovary syndrome (PCOS), diabetes and hypothyroidism. Vexiau et al showed that SHBG levels are inversely correlated to the degree of hair loss in women with FPHL.63
Sex hormone-binding globulin (SHBG) is the main transport protein for circulating T and estradiol. SHBG is produced in liver cells and to some degree in the brain, uterus, placenta and vagina. SHBG levels are regulated by a delicate balance of inhibiting and enhancing factors. High androgen levels decrease the production of SHBG, whereas estrogen and thyroxine increase SHBG. As well, insulin-like growth factor-1 (IGF-1) can suppress SHBG. Only unbound testosterone and estradiol are biologically active; hence, the lower the SHBG blood levels, the higher the bioavailability of these androgens. Conditions characterized by low SHBG levels include polycystic ovary syndrome (PCOS), diabetes and hypothyroidism. Vexiau et al showed that SHBG levels are inversely correlated to the degree of hair loss in women with FPHL.63
![]() It has been shown that hyperandrogenemia can lead to patterned hair loss in susceptible women. Women with marked androgen excess, typically displaying such symptoms as hirsutism and irregular menses, often develop a condition resembling MPHL with deep bitemporal recession and vertex thinning.64–66 Irregular hormone profiles and hyperandrogenemia was shown in 82%–87% of women with FPHL and hirsutism or oligomenorrhea.63,66 This type of balding, which may be referred to as AGA, is treatable with androgen antagonists and 5α-reductase inhibitors.32 These findings suggest that androgen hypersecretion plays a key role in the development of patterned hair loss in at least some women. However, the majority of women with FPHL show no clinical signs of hyperandrogenism and several studies have shown normal testosterone and DHEA-S levels in this group of patients.64–66 Vexiau et al (2000) found abnormal hormone profiles in 67% of women with FPHL and no clinical signs of hyperandrogenism after implementation of the β1–24 corticotropin stimulation test.63 Interestingly, 5α-androstane-3α,17β-diol glucuronide levels were found to be elevated in this patient group; this metabolite is a C19 steroid and reflects the transformation of androgen precursors, mainly of adrenal origin, in women.67 Increased levels of 5α-androstane-3α,17β-diol glucuronide indicate both splanchnic and extrasplanchnic 5α-reductase hyperactivity.63,68 Hence, T and DHEA-S may not be sufficient markers to recognize slight hormonal irregularities that may lead to FPHL. Therefore, the importance of androgen secretion and enzyme activity in the development of FPHL should not be underestimated even when no clinical signs of hyperandrogenism are present. On the other hand, all FPHL cases may not share the same pathogenesis32,69 and may be a combination of androgen-dependent and -independent disease.1,32
It has been shown that hyperandrogenemia can lead to patterned hair loss in susceptible women. Women with marked androgen excess, typically displaying such symptoms as hirsutism and irregular menses, often develop a condition resembling MPHL with deep bitemporal recession and vertex thinning.64–66 Irregular hormone profiles and hyperandrogenemia was shown in 82%–87% of women with FPHL and hirsutism or oligomenorrhea.63,66 This type of balding, which may be referred to as AGA, is treatable with androgen antagonists and 5α-reductase inhibitors.32 These findings suggest that androgen hypersecretion plays a key role in the development of patterned hair loss in at least some women. However, the majority of women with FPHL show no clinical signs of hyperandrogenism and several studies have shown normal testosterone and DHEA-S levels in this group of patients.64–66 Vexiau et al (2000) found abnormal hormone profiles in 67% of women with FPHL and no clinical signs of hyperandrogenism after implementation of the β1–24 corticotropin stimulation test.63 Interestingly, 5α-androstane-3α,17β-diol glucuronide levels were found to be elevated in this patient group; this metabolite is a C19 steroid and reflects the transformation of androgen precursors, mainly of adrenal origin, in women.67 Increased levels of 5α-androstane-3α,17β-diol glucuronide indicate both splanchnic and extrasplanchnic 5α-reductase hyperactivity.63,68 Hence, T and DHEA-S may not be sufficient markers to recognize slight hormonal irregularities that may lead to FPHL. Therefore, the importance of androgen secretion and enzyme activity in the development of FPHL should not be underestimated even when no clinical signs of hyperandrogenism are present. On the other hand, all FPHL cases may not share the same pathogenesis32,69 and may be a combination of androgen-dependent and -independent disease.1,32
![]() A person with MPHL is likely to have a family history of this trait.70 Other findings have contributed to the long-held view that AGA has a genetic basis. Twin studies have shown that monozygotic twins have a high incidence of AGA in both members of the pair (concordance rates 80%–90%)71,72; with less concordance among nonidentical twins. Differences in AGA prevalence among ethnic groups, with Caucasians exhibiting the highest rates, also suggests a genetic role in MPHL.
A person with MPHL is likely to have a family history of this trait.70 Other findings have contributed to the long-held view that AGA has a genetic basis. Twin studies have shown that monozygotic twins have a high incidence of AGA in both members of the pair (concordance rates 80%–90%)71,72; with less concordance among nonidentical twins. Differences in AGA prevalence among ethnic groups, with Caucasians exhibiting the highest rates, also suggests a genetic role in MPHL.
![]() The mode of inheritance is less clear. The common view among the public that MPHL is inherited from the maternal grandfather has its roots in a 1916 study that concluded an autosomal dominant nature of inheritance.73 More recently, the finding that variation in a single allele of the steroid metabolism gene CYP17 on chromosome 10q24.3 is associated with polycystic ovary syndrome in females and AGA in males has lent support to this theory, although the role of the insulin gene in this association identifies this hormone as a possible participant in AGA.74,75 On the other hand, other investigators have observed a strong concordance between fathers and sons with AGA, suggesting paternal inheritance.36,76 Additionally, other findings argue against an autosomal dominant pattern: severity of baldness among the general male population is normally, rather than bimodally, distributed, and the frequency of MPHL in the general male population (40%–60%) is much higher than what would be expected if only a single gene were involved.77 Therefore a polygenic mode of inheritance has been proposed as the most likely scenario,76,77 possibly with roles played by genes passed on by either, or both, the mother and father.
The mode of inheritance is less clear. The common view among the public that MPHL is inherited from the maternal grandfather has its roots in a 1916 study that concluded an autosomal dominant nature of inheritance.73 More recently, the finding that variation in a single allele of the steroid metabolism gene CYP17 on chromosome 10q24.3 is associated with polycystic ovary syndrome in females and AGA in males has lent support to this theory, although the role of the insulin gene in this association identifies this hormone as a possible participant in AGA.74,75 On the other hand, other investigators have observed a strong concordance between fathers and sons with AGA, suggesting paternal inheritance.36,76 Additionally, other findings argue against an autosomal dominant pattern: severity of baldness among the general male population is normally, rather than bimodally, distributed, and the frequency of MPHL in the general male population (40%–60%) is much higher than what would be expected if only a single gene were involved.77 Therefore a polygenic mode of inheritance has been proposed as the most likely scenario,76,77 possibly with roles played by genes passed on by either, or both, the mother and father.
![]() Several studies have attempted to elucidate the identity of the genes involved in AGA. The significant role of DHT would suggest the genes encoding the enzymes involved in its production would play important roles in MPHL. The above-mentioned observation that pseudohermaphrodites lacking a functioning gene for the type II isoform of 5α-reductase do not develop AGA lends credence to this hypothesis58; however, a more recent study investigating the two 5α-reductase isoform genes could not find a role for them in AGA inheritance.
Several studies have attempted to elucidate the identity of the genes involved in AGA. The significant role of DHT would suggest the genes encoding the enzymes involved in its production would play important roles in MPHL. The above-mentioned observation that pseudohermaphrodites lacking a functioning gene for the type II isoform of 5α-reductase do not develop AGA lends credence to this hypothesis58; however, a more recent study investigating the two 5α-reductase isoform genes could not find a role for them in AGA inheritance.
![]() Polymorphism in the gene encoding ornithine decarboxylase was found to be associated with AGA, in that the presence of both the major and the weaker allele was found in men with MPHL.78 Ornithine decarboxylase is an enzyme known to behave as a regulator of the hair cycle; hence, it is a promising candidate for investigations into the cause of AGA, at both the cellular and the genetic levels.
Polymorphism in the gene encoding ornithine decarboxylase was found to be associated with AGA, in that the presence of both the major and the weaker allele was found in men with MPHL.78 Ornithine decarboxylase is an enzyme known to behave as a regulator of the hair cycle; hence, it is a promising candidate for investigations into the cause of AGA, at both the cellular and the genetic levels.
![]() The father-to-son inheritance observed in MPHL suggests an involvement of genes on the Y chromosome. Most of the genes on the Y chromosome are contained in a region that does not recombine; a study investigating a common polymorphism in this region found that AGA was not associated with this set of genes.79 However, the smaller region that does recombine with the X chromosome may yet contain genes involved in AGA and should be studied in this respect.
The father-to-son inheritance observed in MPHL suggests an involvement of genes on the Y chromosome. Most of the genes on the Y chromosome are contained in a region that does not recombine; a study investigating a common polymorphism in this region found that AGA was not associated with this set of genes.79 However, the smaller region that does recombine with the X chromosome may yet contain genes involved in AGA and should be studied in this respect.
![]() The early finding of a maternally linked mode of inheritance for AGA has prompted some to focus on adrenoleukodystrophy. This condition is linked to a mutation on the X chromosome and the finding that AGA is rare in its sufferers suggests that the gene involved is a suitable candidate for investigation into its contribution to the polygenic mode of inheritance for MPHL.80
The early finding of a maternally linked mode of inheritance for AGA has prompted some to focus on adrenoleukodystrophy. This condition is linked to a mutation on the X chromosome and the finding that AGA is rare in its sufferers suggests that the gene involved is a suitable candidate for investigation into its contribution to the polygenic mode of inheritance for MPHL.80
![]() The gene for the AR is located on band q12 of the X chromosome; hence, involvement of this gene in AGA would explain the maternal component of its inheritance. A higher expression of this gene has been found in balding scalp compared to nonbalding scalp,81 perhaps due to mutations in and around the gene site. Polymorphism in the AR has been found to be associated with AGA79,82; indeed, the A allele was found to have a protective effect against pattern balding.82 Additionally, it has been found that the potency of androgens in their actions on the hair follicle is regulated by the AR gene.83 Men suffering of Kennedy disease, a neurodegenerative condition characterized by a partial functional lack in the AR receptor caused by expansion of a repeat sequence on the AR gene, are highly unlikely to develop AGA and indeed have thicker hair in general.27 Overall, it has been suggested that variation in the AR gene is the most important factor governing the occurrence of AGA.
The gene for the AR is located on band q12 of the X chromosome; hence, involvement of this gene in AGA would explain the maternal component of its inheritance. A higher expression of this gene has been found in balding scalp compared to nonbalding scalp,81 perhaps due to mutations in and around the gene site. Polymorphism in the AR has been found to be associated with AGA79,82; indeed, the A allele was found to have a protective effect against pattern balding.82 Additionally, it has been found that the potency of androgens in their actions on the hair follicle is regulated by the AR gene.83 Men suffering of Kennedy disease, a neurodegenerative condition characterized by a partial functional lack in the AR receptor caused by expansion of a repeat sequence on the AR gene, are highly unlikely to develop AGA and indeed have thicker hair in general.27 Overall, it has been suggested that variation in the AR gene is the most important factor governing the occurrence of AGA.
![]() Single-nucleotide polymorphism (SNP) analysis has identified many other candidate genes as participants in AGA.84 One SNP correlated with AGA, rs1652, has been found on the AR receptor gene.85 Recent investigations have focused much attention on the p11.22 gene locus on chromosome 20. A highly significant association has been found between AGA and 5 SNP’s at this site.84 Richards et al found risk alleles at this locus and on the AR receptor gene confer a sevenfold risk of AGA.86
Single-nucleotide polymorphism (SNP) analysis has identified many other candidate genes as participants in AGA.84 One SNP correlated with AGA, rs1652, has been found on the AR receptor gene.85 Recent investigations have focused much attention on the p11.22 gene locus on chromosome 20. A highly significant association has been found between AGA and 5 SNP’s at this site.84 Richards et al found risk alleles at this locus and on the AR receptor gene confer a sevenfold risk of AGA.86
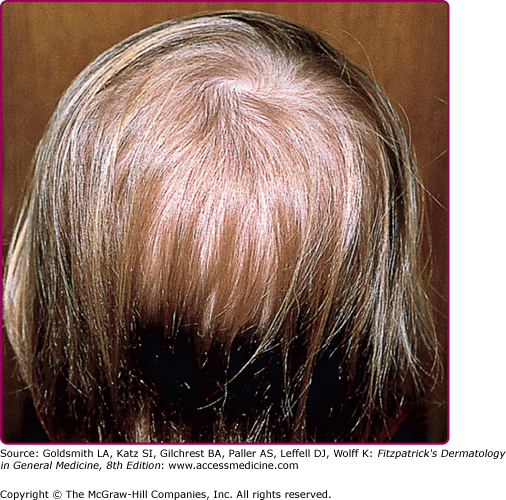
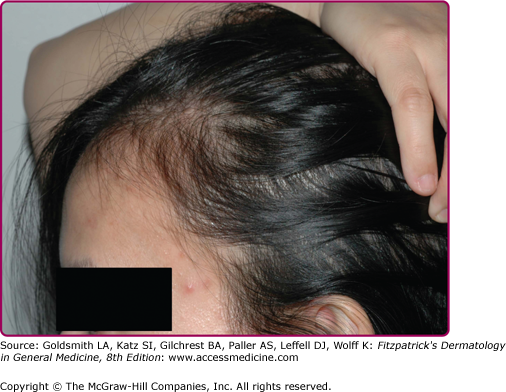
![]() While the incidence of FPHL (25%–38%) in the general population is lower than that of MPHL, societal attitudes towards appearance make the female condition more psychologically serious to its sufferers. The pattern, age of onset (although this almost always follows puberty), final degree of hair loss, and response to pharmacological treatment vary greatly between individuals, and hence caution must be taken when attributing any single underlying cause to what may be a number of variant conditions. In general, the term FPHL refers to any decrease in scalp hair density occurring with age. It should be noted that the diagnosis of FPHL can oftentimes be complicated by the presence of a condition of separate etiology, and different clinical presentation and time course (not age-related), known as TE, described below. The observed patterns of balding are not the same as seen in men: usually, but not always, the hair loss is restricted to the crown and is more diffuse, i.e., it does not show clearly defined recession lines as in MPHL.35,87,88 Also, the frontotemporal recession/vertex balding pattern commonly exhibited by men is not as often seen in women, although it not rare or unusual to see this pattern in FPHL. A frontal fringe of 1–3 cm intact hair, and/or a “Christmas tree pattern” of hair loss on the top of the scalp are more typically seen in women.
While the incidence of FPHL (25%–38%) in the general population is lower than that of MPHL, societal attitudes towards appearance make the female condition more psychologically serious to its sufferers. The pattern, age of onset (although this almost always follows puberty), final degree of hair loss, and response to pharmacological treatment vary greatly between individuals, and hence caution must be taken when attributing any single underlying cause to what may be a number of variant conditions. In general, the term FPHL refers to any decrease in scalp hair density occurring with age. It should be noted that the diagnosis of FPHL can oftentimes be complicated by the presence of a condition of separate etiology, and different clinical presentation and time course (not age-related), known as TE, described below. The observed patterns of balding are not the same as seen in men: usually, but not always, the hair loss is restricted to the crown and is more diffuse, i.e., it does not show clearly defined recession lines as in MPHL.35,87,88 Also, the frontotemporal recession/vertex balding pattern commonly exhibited by men is not as often seen in women, although it not rare or unusual to see this pattern in FPHL. A frontal fringe of 1–3 cm intact hair, and/or a “Christmas tree pattern” of hair loss on the top of the scalp are more typically seen in women.
![]() The progression of patterned hair loss in both genders is the result of a gradual transformation of pigmented, thick scalp hair (terminal hair) into fine, colorless, almost invisible vellus-like hair follicles.36 Hair follicles are grouped in follicular units (FUs) that form during the fetal period. Follicular units usually consist of two to four terminal hair follicles and one to two vellus hair follicles. It is assumed that the FU formation starts with one, so-called primary follicle, followed by the development of associated secondary follicles and later, tertiary follicles. Yazdabadi et al found a reduction in terminal hair follicles in each FU in women with diffuse AGA. They hypothesized that a hierarchy of susceptibility to the miniaturization process exists amongst the hair follicles within an FU.89
The progression of patterned hair loss in both genders is the result of a gradual transformation of pigmented, thick scalp hair (terminal hair) into fine, colorless, almost invisible vellus-like hair follicles.36 Hair follicles are grouped in follicular units (FUs) that form during the fetal period. Follicular units usually consist of two to four terminal hair follicles and one to two vellus hair follicles. It is assumed that the FU formation starts with one, so-called primary follicle, followed by the development of associated secondary follicles and later, tertiary follicles. Yazdabadi et al found a reduction in terminal hair follicles in each FU in women with diffuse AGA. They hypothesized that a hierarchy of susceptibility to the miniaturization process exists amongst the hair follicles within an FU.89
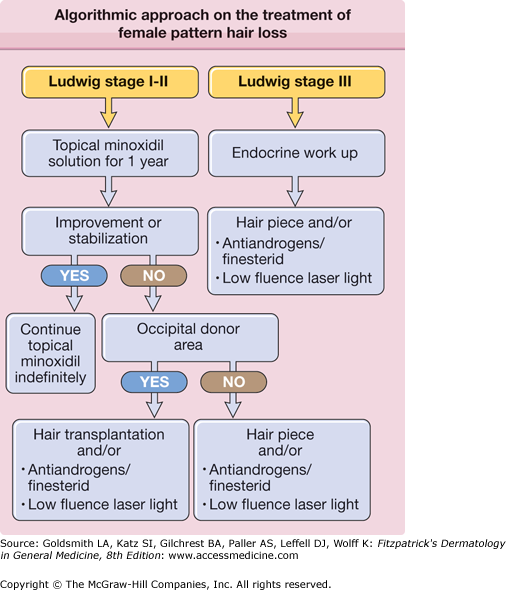
The identification of AGA is usually not difficult if the alopecia occurs in a classical clinical pattern. In 1951, Hamilton produced the first grading scale for MPHL. The Hamilton scale ranges from type I to VIII. Whereas type I represents the prepubertal scalp with terminal hair growth on the forehead and all over the scalp, type II and III show gradual frontal mostly M-shaped recession of the hairline, type IV, V and VI show additional gradual thinning in the vertex area, type VII and VIII show a confluence of the balding areas and leave hair only around the back and the sides of the head.50,90 In 1975 Norwood modified the classification, and included variations on the middle grades III a, IV a and V a, that show a more prominent gradual receding of the middle portion of the frontal hairline and type III vertex which is characterized by a loss of hair mainly in the tonsure area and a frontotemporal recession which never exceeds that of type III.91 (Fig. 88-4). In 1977, Ludwig introduced a classification for pattern of AGA in women, characterized by a diffuse loss of hair on the crown and persistence of the frontal hairline.92 In 1994, Olsen noted that women with AGA did not necessarily present with diffuse hair loss over the entire top but rather may have increasing hair loss towards the front, called frontal accentuation or Christmas tree pattern (Fig. 88-5). Women can also show a male pattern of distribution, as well as men can show a more female pattern.1
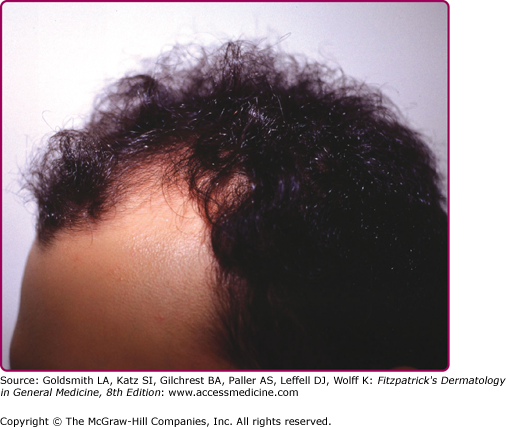
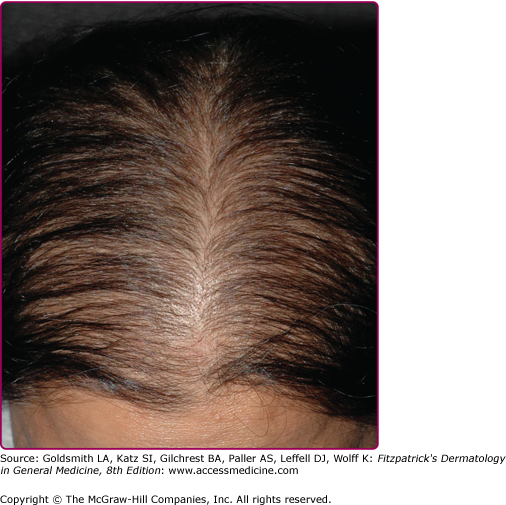
Figure 88-5
Pattern hair loss in women. A. Different phenotypic expressions. B. Characteristic frontal accentuation (widened hair part). (From Wolff K, Goldsmith LA, Katz SI, Gichrest BA, Paller AS: Fitzpatrick’s Dermatology in General Medicine. 7th ed. Copyright © The McGraw-Hill Companies, Inc. All rights reserved, with permission.)
A thorough scalp exam together with the patient history usually allows a definitive diagnosis.
Standardized global scalp photography, especially of the part area, is very helpful as a qualitative assessment of the progression of the hair loss and as therapy control. A pull test and a trichogram can give information on the ongoing activity of the condition. Videodermoscopy and phototrichogram techniques can be used for therapy control.
The diagnosis can be more difficult if the hair loss is more diffuse over the entire scalp or if it occurs together with other hair loss conditions such as TE, diffuse alopecia areata or mild forms of cicatricial alopecias. A scalp biopsy allows a definitive diagnosis, since it provides information on histological features, the number of terminal and vellus hair per area and the number of anagen and telogen hair.
In women, a laboratory test for ferritin and thyrotrophin-stimulating hormone (TSH) are recommended to rule out sources for and underlying TE. An extensive laboratory workup for androgens is not recommended for a routine visit. Women with irregular periods and/or other signs of androgen excess should be at least checked for free and total testosterone as well as DHEA-S. The best time for the blood work is in the morning of one of the days of her menstrual cycle. She also must be off the pill for at least one cycle.
An increased risk of coronary heart disease and insulin resistance has been correlated for early vertex balding, especially in young men with hypertension, obesity, and dyslipidemia.93–95 Early vertex balding has also been correlated with an increased risk of prostate cancer.96,97
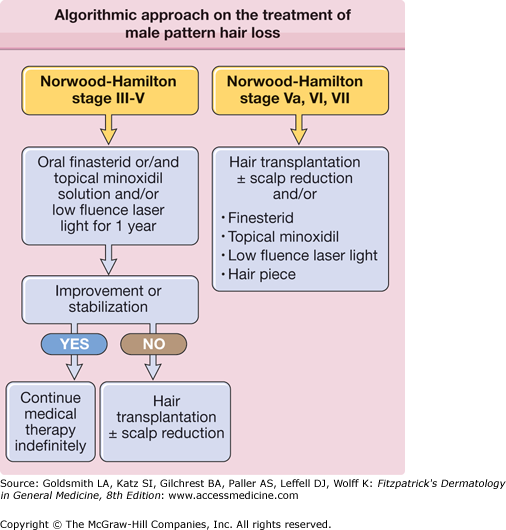
AGA is a progressive condition with a decrease in hair density of approximately 6% of hair fiber per year.40 However, increased shedding can occur periodically and the extent of hair loss depends on the genetic predisposition. Currently two pharmaceutical treatments are approved for the therapy of AGA in men: oral finasteride and topical minoxidil.
Minoxidil is a biologic response modifier, which has been shown to halt AGA in many patients and regrow hair to a certain extent. Minoxidil, a piperidinopyrimidine derivative, was noted to cause hypertrichosis when administered orally as an antihypertensive. It is now used as a 2% and a 5% topical treatment in a lotion or foam preparation.
The mechanism of action is not fully understood. A direct effect on the hair follicle cells may be responsible for the effects of minoxidil. It has been shown to have a mitogenic effect on epidermal cells leading to prolonged survival time and induced increased proliferation of hair follicles in vitro.98–100 A possible mechanism of action involves a change in calcium homeostasis of cells, as minoxidil is converted to minoxidil sulfate, a potassium channel agonist. Increased potassium channel permeability leads to impaired entry of calcium into cells, thus decreasing epidermal growth factors and enhancing hair growth.101
Several clinical trial have shows the efficacy of topical minoxidil. An increase in hair counts probably reflects reversal of miniaturized hairs to thicker, more highly visible terminal hairs. Although studies have been performed on the vertex scalp, the drug also works on the frontal scalp, especially if hairs have not completely miniaturized to vellus-like hairs. Moderate to dense regrowth could be seen in up 30%–45% of patients.41 Some patients experience an increased shedding in the first 4–6 weeks of application. This positive sign seems to indicate anagen induction with earlier “molting” of telogen hairs from the follicles. The patient should be educated and prepared for this possible side effect to improve compliance. Observed side effects include contact dermatitis in 6.5% of patients and facial hypertrichosis in 3%–5% of women.102 Most patients do not have a true contact allergy to minoxidil but an irritation from propylene glycol. The 2% lotion with less propylene glycol, other vehicles with butylene glycol or the foam may then be used. To discriminate, which component causes the dermatitis, a patch test or testing the product on the volar forearm (repeated open application test) may be helpful.
Only minimal amounts of minoxidil are systemically absorbed and serum levels are too low to have hemodynamic effects in normotensive or hypertensive patients. Nevertheless, less than one in thousand patients may experience tachycardia and decreased blood pressure. Patients with hypotension or heart problems should be cautious and use the medication with approval from their cardiologist. The cardiac effects suggested in earlier studies could not definitely be linked to minoxidil and may be due to increased incidence of coronary artery disease in subsets of men with AGA.93
Topical minoxidil solution is used twice daily (1ml or 25 drops bid). It is also available in a 5% foam. If the hair has been shampooed, the hair and scalp should be at least towel-dry. The lotion or foam should stay on the scalp for at least 4 hours before the next shampoo. The patient should be informed that this is a lifelong treatment. It takes 4–6 months before the medication starts working and that the maximum effect can be expected after 1 year.
Finasteride is a synthetic azo-steroid that has been used for the treatment of AGA in men since 1997. It is a potent and highly sensitive selective 5α-reductase type-2 inhibitor.59 It binds irreversibly to the 5α-reductase isoenzyme 2 and inhibits the conversion of testosterone to DHT. Finasteride has a pharmacological half-life of around 8 hours. The administration of 1 mg finasteride daily reduces the concentration of DHT in scalp skin by 64%, serum DHT is reduced by 68%.59 The dose response curve is nonlinear and therefore higher doses do not lead to significantly increased suppression of DHT or greater clinical benefits.103 In placebo-controlled studies, a significant hair count increase in men with vertex alopecia or frontal AGA could be shown after 6 and 12 months.104,105 Finasteride stabilizes hair loss in 80% of patients with vertex hair loss and 70% of patients with frontal hair loss. The chance of mild to moderate regrowth is 61% on the vertex and 37% on the frontal scalp.106 After 24 months of continuous use, 66% of the patients experienced a certain amount of hair regrowth in the vertex area (approximately 10%–25% of the hair the patient lost previously).107 Most of the patient showed no further hair loss and only a few patients continued to lose hair. Continued use beyond 2 years does not promote continued hair regrowth. Instead the hair density stabilizes with the retention of the newly acquired hair.107 If successful, the treatment should be continued indefinitely because the balding process continues once treatment ceases.38 Finasteride was found to be well tolerated with side effects occurring in fewer than 2% of patients. The side effects included decreased libido in 1.8% of the recipients versus 1.3% in the placebo group, erectile dysfunction in 1.3% of the recipients versus 0.7% in the placebo group and decreased ejaculate volume in 0.8% of the recipients versus 0.4% in the placebo group.108,109 Finasteride 1 mg daily does not affect spermatogenesis or semen production in men aged 19–41 years of age.110 The effect on prostate volume and serum prostate specific antigen (PSA) in younger men was small and reversible after discontinuation of the drug.110 Finasteride can decrease PSA levels by 50% in older men.111 Therefore a baseline PSA should be taken in men over 40 and the family doctor should be advised to double the PSA value while patients are taking finasteride.106 Long term side effects of 1 mg finasteride daily are yet unknown. A placebo controlled study over 7 years carried out in 9,060 men 55 years of age or older, taking 5mg finasteride per day or placebo, showed that finasteride prevents or delays the appearance of prostate cancer, but a slightly higher risk of high-grade prostate cancer.
Finasteride is not approved for the use in women and its efficacy in FPHL is still controversial. A multicenter double-blind, placebo-controlled, randomized study of finasteride 1 mg/day in postmenopausal women with FPHL showed no differences in anagen:telogen ratio and the terminal hair:miniaturized hair ratio. However, Camacho et al reported hair regrowth using finasteride 2.5 mg/day in 41 women with FPHL and SAHA (seborrhea, acne, hirsutism, and alopecia).39,49
Dutasteride is an inhibitor of type I and II 5α-reductase. It is approved at a dose of 0.5 mg daily for the treatment of symptomatic benign prostatic hyperplasia. Some studies have shown great efficacy in the treatment of MPHL and FPHL.112–115 However, dutasteride is not FDA approved for use in androgenetic alopecia. More studies are necessary for the evaluation of the safety profile of this drug.
The antiandrogen cyproterone acetate (CPA) is a synthetic derivative of 17-hydroxyprogesterone. It acts as an AR antagonist with weak progestational and glucocorticoid activity.62 It also inhibits the steroidogenic enzyme 21-hydroxylase, reducing the production of aldosterone and to a lesser extent 3-β-hydroxysteroid dehydrogenase, both of which are needed to synthesize cortisol. CPA is available in Europe, Canada and South America. It is usually combined with ethinyl estradiol as a birth control pill. CPA is not approved by the FDA for the treatment of AGA. For the treatment of FPHL a regimen with 100 mg CPA daily on days 5–15 of the menstrual cycle and 50 μg of ethinyl estradiol on days 5–25 or 50 mg CPA daily on days 1–10 of the cycle and 35 μg of ethinyl estradiol on days 1–21 have been suggested.116 In a randomized 12 months clinical trial in 66 women, 33 women with FPHL used topical minoxidil 2% plus combined oral contraceptive whereas 33 women received CPA 52 mg daily plus ethinyl estradiol 35 μg for 20 days of the cycle. The later combination result in greater hair density in women with hyperandrogenism.117 Side effects from CPA are irregular menstrual cycles, weight gain, breast tenderness, loss of libido, depression, nausea. Since CPA is an antiandrogen, its use in men is obsolete, unless a gender change is desired.
Spironolactone is a synthetic 17-lactone drug, which is a renal competitive aldosterone antagonist with a mild antiandrogenic effect by blocking the AR and preventing its interaction with DHT. The maximum androgen suppression is reached after 4–12 months; dosages of 200 mg daily are required. Spironolactone may have a preventative effect in FPHL and may reduce shedding in individuals without hyperandrogenism.118 However, Spironolactone is not approved by the FDA for the treatment of FPHL and, sd sn antiandrogen, should not be used in men. The main side effect is menstrual irregularities, which may be mitigated by decreasing the dose to 50–75 mg/day and adding oral contraceptives or after 2–3 months of therapy. Spironolactone is contraindicated in patients with renal insufficiency, hyperkalemia, pregnancy, abnormal uterine bleeding, and women with genetic predisposition of breast cancer.116,118
In Europe topical 17α- or 17β-estradiol are commercially available for the treatment of FPHL. Studies showed an increased in anagen and decreased telogen rates after topical treatment compared with placebo treatment.119 The underlying pathways of 17α-estradiol induced hair regrowth are unknown. Niiyama et al showed that 17α-estradiol is able to diminish the amount of DHT formed by human hair follicles after incubation with testosterone while increasing the concentration of weaker steroids.119,120 Recently, it has been shown that hair follicles in women with FPHL express more aromatase activity as compared to male hair follicles. Under the influence of 17α-estradiol, an increased conversion of testosterone to 17β-estradiol and androstenedione to estrone takes place in hair follicles derived from the occiput, which might explain the beneficial effects of estrogen treatment in FPHL. Woman who were taking aromatase inhibitors were shown to develop FPHL more rapidly.121 Another theory about the effectiveness of estradiol is the systemic induction of SHBG and therefore the reduction of free, bioavailable testosterone.63 Since estradiol is absorbed through the scalp skin, systemic side effects must be considered, and it cannot be used in men.
Laser sources have become very popular in medical and nonmedical areas. Manufacturers and suppliers often guarantee hair regrowth and various devices are available without prescription. The only FDA approved low-fluence laser light device is the Hair Max Laser Comb® (Lexington international, LLC, Boca Raton, FL, United States of America) (FDA approval as a medical device). Paradoxical hair growth has occurred in patients undergoing laser hair removal when relatively low energy fluences were used. The mechanism of action of this phenomenon is unknown. One theory suggests an increase in blood flow in the dermal papilla.122–124 Low-level laser light sources appear to be safe to use in the treatment of hair loss. More studies are necessary to understand the mechanism of action and to evaluate the efficacy of these devices.
Hair restoration is the most successful and permanent treatment for AGA in suitable candidates. It includes hair transplantation (HT) and, in skillful hands, scalp-reduction surgery. Suitable candidates for HT are those with reasonable expectations, a donor supply that is adequate to cosmetically improve the recipient area coverage and those without contraindications for surgery. The most dramatic change in cosmetic appearance is achieved in patients with stages Hamilton–Norwood VI and VII, and in patients with anterior accentuation of balding (subtypes IIIa and IVa, “Christmas tree pattern”).
With recent advancements in technique and combination with medical treatment, more patients may benefit from the surgical option. Larger numbers of smaller grafts are moved per session, and results have thus become very natural.125,126 It is possible and advisable to distribute small grafts in between preexisting hairs and thus account for future hair loss. Rational use of the donor area with strip harvesting or FU extraction makes several sessions possible in many patients if they experience progressive hair loss.
HT is based on the principle of donor dominance as shown by androgen-independent follicles retaining their properties when they are transplanted into androgen-dependent areas. The donor supply is limited by the area of the strip (size of the “safe zone,” scalp elasticity) and the density of donor hair.
HT is an outpatient procedure and may take up to 10 hours, depending on various factors, especially the number of grafts. Tumescence anesthesia is used for the donor and recipient areas, sometimes combined with nerve blocks. The most commonly used technique is strip harvesting. It allows for a relatively fast removal of large numbers of hairs leaving a fine line as a scar, which can be minimized with special harvesting and wound closure techniques. The strip is dissected into FUs (“families” of hairs growing together in one connective tissue sheath) under magnification these grafts are then carefully and strategically placed in the balding areas. The recipient side is prepared with small needles or spears, according to the size of the graft. A recent technique involves separately harvesting individual FUs using very small blunt punches (follicular unit extraction (FUE). This procedure is usually more time consuming but avoid a long scar in the occipital area. Follicular unit extraction is indicated in patients who desire to wear a very short hairstyle.
Scalp prostheses are practical for patients who are not candidates for hair restoration surgery, women with extensive hair loss and/or patients without satisfying improvement after using medical therapy. Wigs and hairpieces can provide excellent cosmetic results, especially when they are custom made. It is usually easier to overcome the reluctance to wear a scalp prosthesis if the hair piece blends in nicely with the preexisting hair and is comfortable to wear. Women tend to be less reluctant to wear a wig or hairpiece, especially if the patient is exposing her natural hairline (Figs. 88-6 and 88-7).
Diffuse Hair Loss
Hypotrichosis simplex is characterized by progressive global loss of scalp hair starting during childhood. This autosomal dominant disorder affects both sexes equally; eyebrows and body hair is unaffected by the condition. The pathogenesis is of hypotrichosis simplex is not fully understood. In two families with hypotrichosis simplex, a gene defect in the corneodesmosin gene (adhesin protein) was found84,127 (Fig. 88-8).
A failure in normal follicle development in utero can results in a reduction or absence of hair follicles. These developmental disorders are often associated with ectodermal defects. These hereditary syndromes, most frequently show abnormalities of bones, central nervous system, teeth or eyes (see Chapter 142). The most common ectodermal dysplasia, hypohidrotic ectodermal dysplasia, which is characterized by sparse hair, abnormal teeth and reduced or absent sweating, is due to a mutation in the ectodysplasin signaling pathway.128 This pathway is involved in the early embryogenic formation of the hair follicle.129–131 Ectodermal dysplasias with hair disorders are discussed in Chapter 142.
Atrichia with papular lesions is an autosomal dominant hair disorder that presents in infancy. Hair is usually present at birth but alopecia develops within the first year of life. Several years after the development of alopecia, papular follicular cysts often appear.132 Mutations either in the hairless gene or the gene encoding the vitamin D receptor can lead to this phenotype. Hair follicle formation in utero appears to be normal, but massive apoptosis in the hair bulb during the first catagen phase leads to a separation of the dermal papilla from the base of the hair follicle and consequent failure to reenter anagen. The follicular epithelium than undergoes a cystic change. If universal hair loss occurs during the first month of life, atrichia with popular lesions and alopecia areata universalis should be considered as differential diagnosis. If universal alopecia is seen in the family, gene testing and genetic counseling should be considered.
The term short anagen hair syndrome applies to a poorly understood clinical presentation of short fine hair in children.87 The hair fails to grow long due to a shortened anagen phase. Hair density and hair shafts seem to be normal. The condition may improve after puberty. Short anagen hair can be inherited autosomal dominant or can occur sporadically.
Loose anagen syndrome is characterized by an easy epilation of anagen hair. The hair appears to grow slowly and can be pulled out without pain. Hair density can appear normal or reduced and some children may display demarcated areas of incomplete alopecia. The typical patient with loose anagen hair syndrome is 2–5 years of age. The condition more frequently affects girls and hair is most often light blond. The hair loss tends to get better without any treatment once the child grows older. Microscopic examination of gently pulled hair can make the diagnosis; 80%–100% of the hairs are anagen hairs with a ruffled cuticle and no inner root sheath. However, the hair loss can cycle, and it may be hard to gather enough hair with a gentle pull, necessitating collection by the parent at home and later microscopic evaluation. Loose anagen hair syndrome can be familial, sporadic or associated with other developmental defects such as Noonan syndrome or hypohidrotic ectodermal hyperplasia.133 It is also seen in association with HIV.134 Hair shaft abnormalities, alopecia areata and trichotillomania have to be considered in the differential diagnosis. (See Fig. 88-9.)
Telogen Effluvium
The second most common cause of hair loss in women after FPHL is TE. The latter presents as a nonpatterned increase in shedding of terminal hairs, diffusely over the entire scalp, and can produce an apparent thinning of hair in severe cases.135 While both genders can experience TE, attitudes toward hair loss result in a greater proportion of females who complain. TE can copresent with AGA, particularly in early-onset situations, and this can complicate diagnosis and treatment. TE differs from AGA in that it is not androgen-sensitive, does not appear to be inherited and, since it does not involve a terminal- to vellus-hair transition, does not decrease matrix cell volumes or hair shaft diameters.136 TE also tends to be related to external causes and is often reversed when the exogenous stimuli are removed.
|
The pathophysiology underlying TE is best characterized as a premature shift of hairs from the anagen (growth) phase into the catagen (resting) and telogen (terminal) phases. However, there are variants: anagen may be prolonged, or telogen may instead be shortened or prolonged. Which type of shift occurs depends on the stimulus producing the shift, with the main clinical difference being the latency of effluvial onset following the stimulus.
The hair loss that commonly occurs following pregnancy is generally seen 2 or 3 months postpartum, although some individuals can exhibit longer times to onset. While this is classic TE, the mechanism has been shown to involve a delayed transition from anagen to catagen/telogen, which results in a simultaneous shedding of large numbers of terminal hairs.137 This hair does eventually regrow; however, the returning hair may show changes in texture, color and curliness, and may not attain its previous length. As such, pregnancy (parturition or abortion) may in some cases produce permanent changes in anagen length.136
Other perturbations can produce TE, usually involving premature termination of the anagen phase. Some women experience transient TE 2–3 months after discontinuing or changing oral contraceptive medication; the delayed onset of TE in these cases distinguishes it from the anagen effluvium (AE) initiated by certain drugs (see below). In the 1970’s, the popularity of fad “crash” diets resulted in many cases TE about 3 months after initiation of these spartan regimens, depending on the severity of weight loss. Sudden deprivation of amino acids and other dietary factors most likely produced the condition, and the hair tended to regrow following cessation of the diets.136 Surgical procedures, psychological traumas, and febrile illness have all been reported to produce TE events.
Drugs are widely reported to produce temporary hair loss. This is usually, but not necessarily, of the AE variety, since, depending on the causal agent, the time course and severity may suggest a diagnosis of TE to be appropriate. Agents producing TE include cimetidine, enalapril and captopril, imiquimod, metoprolol and propranolol,138–141 lithium,142 l-dopa143 trimethadione,144 and bromocriptine.145 The hair loss from administration of etretinate146 and isotretinoin are problems, more of the AE, as is hair loss that sometimes follows renal dialysis, possibly with hypervitaminosis A.136 Finally, hair loss occurring following environmental contamination or poisoning, for example with selenium, arsenic, thallium, mercury, and lead, displays an AE-like rapid onset, probably involving a cytotoxicity mechanism.
TE is characterized by a fairly sudden onset of massive shedding. Anagen hairs are prematurely shifted into telogen hairs and the normal anagen/telogen ratio of 90:10 can switch to 70:10. Women often present with the “bag sign”: bringing in bags with hair that they have collected every day or over a couple of days (Fig. 88-10). More than 300 telogen hairs can be shed every day. The global examination of the scalp may show a reduction in hair density especially in the temporal area. The pull test is usually positive (3 or more hairs can be pulled out on different parts of the scalp). A trichogram or phototrichogram can be use to quantify the amount of telogen hair. A scalp biopsy may be helpful to distinguish the condition from diffuse alopecia areata or AGA.
Chronic Telogen Effluvium (CTE) was first proposed in 1996 as a means of distinguishing the abrupt-onset, short-acting type TE, usually caused be exogenous triggers or parturition, from a more durable condition (CTE) that may not be so clearly related to any external event.147
A few conditions have been proposed to be underlying stimuli for CTE. While “crash” diets have been pinpointed as potential triggers for acute TE, chronic malnutrition can analogously lead to CTE. Protein deficiency is the likely mechanism in this type of balding. It is less clear whether zinc148 or biotin deficiencies are also correlated with chronic diffuse hair loss. Although controversial, iron deficiency, as evidenced by decreased serum ferritin and anemia, may be a trigger for CTE.27,149,150,151 Hypothyroidism has also been associated with CTE (Box 88-2).
|
CTE can most commonly be seen in women. Patients report ongoing massive shedding or recurrent episodes of shedding. As a rule of thumb, any diffuse hair shedding lasting longer than 6 months after any triggering event, or after withdrawal from suspected causal drugs, should be considered CTE. The clinical examination can show a normal or reduced hair density. Regrowth of tapered new anagen hair can usually be found. The pull test may be moderately positive. A trichogram or phototrichogram can be used to confirm and quantify the diagnosis. A scalp biopsy is very helpful for the confirmation of the diagnosis and to distinguish the condition other forms of alopecia. Since other types of hair loss disorders, chiefly FPHL/MPHL and alopecia areata, may copresent with TE and CTE, clinicians may be advised to assay serum iron and thyroid hormone concentrations in order to eliminate iron deficiency and hypothyroidism as treatable causes for the patient’s baldness.152
(Box 88-3)
Both acute and CTE usually resolve once trigger factors are eliminated. However, in CTE triggers may be difficult to identify. Women with TE are often most concerned about complete baldness. The patient has to be reassured that the condition does not lead to complete baldness and that the hair likely grows back around 6 months after removal of the initiating trigger. The patient should understand that the condition is reversible, but that the shedding may persist for a few weeks or months once the initiation factor is eliminated.
The removal of the cause is the major goal in the treatment of TE. Iron supplementation is recommended if the ferritin level is less than 70 ng/mL.150,153 Borderline hypothyroidism can be difficult to identify. Women, who complain about hair loss, depression, lack of energy, mental fatigue, cold intolerance, weight gain or/and constipation are suspicious for the diagnosis of hypothyroidism. TSH levels may fluctuate but are usually elevated, with normal or reduced thyroid hormone levels. If a thyroid dysfunction is suspected, the patient should be closely followed by an endocrinologist. Topical 2% or 5% minoxidil solution 1 mL twice daily can be helpful, especially in women with prolonged hair loss with unknown triggers or in patients with drug related hair loss who are unable to discontinue the initiating medication.
Anagen Effluvium
AE is a result of a disturbance of hair follicle matrix cells. The anagen phase is interrupted and the hair falls out 7–14 days after the initiating event without entering catagen or telogen. Two different types of AE can be distinguished: Dystrophic AE and Immediate anagen release. Dystrophic AE can be caused by chemotherapy, radiation, toxins or alopecia areata. Microscopic investigation of the hair bulbs, obtained from a hair pull test or trichogram, usually shows a tapered tip with the weakened hair shaft broken shortly above the bulb (“dystrophic hair”).1
Drugs used in chemotherapy quickly produce severe hair loss and even total baldness. A rapid onset undoubtedly indicates an immediate release from anagen hair. Immediate anagen hair release is characterized by an easy release of anagen hairs after gentle pulling. The anagen hair has a broom-shaped, pigmented bulb. Therapeutic agents that can cause immediate anagen hair shedding include vincristine, vinblastine, methotrexate, doxorubicin, and fluorouracil.
Normal appearing anagen hair with inner and outer root sheath can be found to some extent in every AE, but especially in bullous dermatosis of the scalp with sub- or intraepidermal blisters.
Once the initiating trigger is removed, the hair usually regrows after around 120 days. Cases of incomplete recovery following multiagent chemotherapy have been reported.1 Patients should be advised about scalp prostheses and other forms of head covering.
Nonscarring Focal Hair Loss
|
At any given time, approximately 0.2% of the world population is suffering from alopecia areata with an estimated lifetime risk of 1.7%.154,155 It is a common cause of abrupt-onset hair loss, but occurs less frequent than androgenic alopecia or TE. Both sexes are affected equally. Although it may occur at any age, incidence at younger age is higher. Alopecia areata is the most common form of alopecia seen in children. The familial occurrence is around 15% but expression of the disorder is variable among different family members. 5% of patients suffering from alopecia areata develop hair loss of their entire scalp hair (alopecia totalis), and 1% of patients develop loss of total body hair (alopecia universalis) at some point.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree