Guttate Hypopigmentation
Electra Nicolaidou
Andreas Katsambas
BACKGROUND
Idiopathic guttate hypomelanosis (IGH) is a common acquired skin disorder, characterized by the presence of well-defined, round to oval, porcelain white macules a few millimeters in diameter. The lesions are usually noticed on the extensor surface of the upper and lower extremities, and their prevalence increases with age. The pathogenesis of the disorder is not clear, although chronic sun exposure seems a strong contributing factor.
IGH is very common with a reported prevalence of 87% in patients older than 40 years. The prevalence is higher with advancing age and similar among males and females.1 Lesions may appear quite early in life, even before the age of 20 years.2 IGH is described in all races and skin types.
The lesions of IGH are asymptomatic, but many affected patients seek medical care to confirm the benign nature of the disorder and to discuss the aesthetic improvement of the lesions. Many dermatologists choose to reassure the patients and offer no treatment. Recent studies have, however, used several treatment modalities with good results.
PRESENTATION
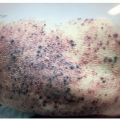
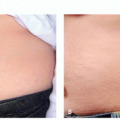
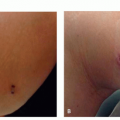
Idiopathic guttate hypomelanosis presents with well-demarcated, round to oval porcelain white macules with a diameter of 0.5 to 6 mm predominantly distributed on the extensor surfaces of the upper and lower extremities (Figure 2.2.1). Larger lesions have also been described.
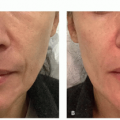
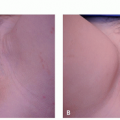
Lesions have a predilection for sun-exposed areas of arms and shins, but they can also occur on sun-protected sites. Involvement of the face has been described in 6% of patients.1 The number and size of the lesions increase with increasing age (Figure 2.2.2), and more than 100 lesions have been described in older individuals.
DIAGNOSIS
Clinical Diagnosis
Diagnosis of IGH is made clinically by the presentation of typical porcelain white small round to oval macules on sun-exposed extremities. The small, well-circumscribed
white lesions on arms and shins can easily be differentiated from other causes of hypopigmentation or depigmentation, such as vitiligo, postinflammatory hypopigmentation, pityriasis versicolor, and lichen sclerosus et atrophicus.
white lesions on arms and shins can easily be differentiated from other causes of hypopigmentation or depigmentation, such as vitiligo, postinflammatory hypopigmentation, pityriasis versicolor, and lichen sclerosus et atrophicus.
Histopathology
Decreased melanin pigment and reduced numbers of melanocytes have been reported in IGH lesions.2 Furthermore, small areas of retained melanin in the basal layer that alternate with greater areas of melanin loss have been proposed as a very specific finding for IGH in a recent study.3
Subtypes
No subtypes have been defined for this condition.
Differential Diagnosis
Vitiligo
Tinea versicolor
Lichen sclerosus et atrophicus
Dowling-Degos disease
Tuberous sclerosis
Pityriasis alba
Granuloma annulare
Sarcoidosis
PATHOGENESIS
The exact pathogenesis of IGH remains obscure. As it mainly occurs on sun-exposed areas, chronic ultraviolet (UV) exposure seems to play a pivotal role in the development of the lesions. However, IGH lesions are also found on nonexposed sites, suggesting that senile degeneration of the skin may also contribute to the pathogenesis of the disorder.5
TREATMENT
Idiopathic guttate hypomelanosis is a very common skin disorder, and an increasing number of patients seek medical care for the cosmetic improvement of the lesions. Many physicians consider IGH an insignificant disorder and, given the lack of a universally effective treatment, choose to just reassure and not treat the patients. This attitude is also reflected on the very small number of available studies for the treatment of such a common condition. However, we can no longer ignore the fact that we now have several treatment modalities that have produced satisfactory results in many patients.
Medical
Topical Calcineurin Inhibitors
The topical calcineurin inhibitors (TCIs) pimecrolimus and tacrolimus have been licensed for the treatment of atopic dermatitis, but they have also been used in a number of other skin disorders, including vitiligo. A stimulatory action on tyrosinase activity and expression, which eventually leads to melanin biosynthesis6 along with an enhancement of melanocyte proliferation and migration7 has been proposed as possible mechanism for the induction of repigmentation by TCIs.
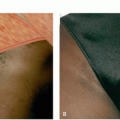
Both pimecrolimus and tacrolimus have been studied for the treatment of IGH. Pimecrolimus was used in a small study that included 4 patients. After 8 weeks of treatment, a 25% to 75% improvement was observed in 3 of 4 patients.8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree