Guidelines and Patient Selection Criteria for Nipple and Skin-Sparing Mastectomy
Costanza Cocilovo
Maurice Y. Nahabedian
History
Over the past few years, nipple-sparing mastectomy (NSM) has been increasing performed and requested by more and more patients. At present, most major breast centers are performing NSM with favorable outcomes in the vast majority of patients. Initial questions regarding safety and efficacy have been answered; however, the present focus is centered around the evolving guidelines for NSM based on tumor characteristics as well as breast volume and dimensions.
The Halsted radical mastectomy was first performed in 1894. In the 1960s, Patey described the modified radical mastectomy (MSM) that achieved comparable local recurrence risk. In 1991 as plastic surgeons began performing immediate breast reconstruction, skin-sparing mastectomy (SSM) became the standard. SSM had the same recurrence risk as MSM (1). Early clinical trials performed in the 1990s demonstrated that the nipple areolar complex (NAC) was involved in 5% to 12% of cases, a relatively low number (2). However, at the time, the technique did not achieve wide acceptance because of the concerns regarding oncologic safety. It was 2002 before Veronese published his 20-year data demonstrating that breast conservation with NAC preservation was oncologically equivalent to mastectomy (3).
Indications
As NSM has increased in incidence and popularity, a variety of studies have clarified the indications and risks associated with NSM. Morimoto reported a direct relationship between nipple involvement, tumor diameter, and distance to the tumor. Forty-one percent of T2 tumors and 78% of tumors greater than 5 cm had nipple involvement (4). Luttges found that tumors within 1 to 2 cm of the nipple had a 36% incidence of nipple involvement versus 13% if the distance is between 2 and 3 cm (5). Nipple involvement was 19.4% when tumor was less than 4 cm away and 3.7% when it was greater than 4 cm (6). In 2006, Sacchini et al. reported that NSM may be considered for tumors less than 2.5 cm, greater than 4 cm from the nipple with negative axilla, and no lymphovascular invasion or extracapsular extension (7).
In the setting of NSM, the terminal duct units are left behind in the NAC and are not associated with breast size or obesity. Interestingly, the highest recurrence rates are found in younger-age women and lactating women but the retroareolar region was still not a common area for recurrence. Studies have demonstrated that the lateral quadrant and axillary tail are more common areas of recurrence compared to the NAC (8). In 2012 Murthy and Chamberlain summarized 10 series of NSM ranging in number from 42 to 579 mastectomies which showed a nipple recurrence risk of 0% to 1.6% (9).
Contraindications
Absolute contraindications to NSM include evidence of NAC involvement, locally advanced breast cancer with skin involvement, and inflammatory breast cancer and bloody nipple discharge (10). Things to consider but are no longer exclusion criteria when determining if a patient is a candidate for NSM include tumor size, tumor-to-nipple distance, positive nodes, prior chest wall radiation, smoking, diabetes, and obesity. All of these are no longer considered an absolute exclusion criterion. Other potential contraindications include significant ptosis and potentially stretch marks on the skin. Coopey et al. reported feeling comfortable with a majority of women undergoing mastectomy because of the low local recurrence risk of 2.6% with 2-year follow-up and no recurrence in the nipple. They report that any tumor size and any distance to the nipple are safe as long as the margin is clear (10). Schneider et al. reported a favorable experience with a subset of 19 patients with large ptotic breasts (11).
Preoperative Planning
The physical examination is a critical component in determining candidacy for NSM. Optimal preoperative planning is based on the tumor location and size as well as breast volume, degree of ptosis, and likelihood of maintaining viability of the NAC. In general, ideal candidates for NSM include women with mild-to-moderate breast volume in which the bra cup size ranges from A to C. In women with mammary hypertrophy or grade 3 ptosis, NSM may be fraught with complications such as delayed healing, partial necrosis or total necrosis. In these patients, a premastectomy procedure such as a reduction mammaplasty or mastopexy can be considered as initially described by Spear (12). In this scenario, a partial mastectomy and oncoplastic reduction mammaplasty is performed followed 1 to 3 months by the NSM.
When considering NSM, it is important to assess prior breast surgery, location of scars, and prior history of radiation therapy. In general, prior breast operations do not preclude NSM, unless the incisions are extensive and have violated the perfusion to the NAC. Prior radiation therapy and a history of smoking will potentially compromise the circulation to the NAC following the mastectomy and may increase the likelihood of necrosis.
Operative Technique
Patient Selection
The operative technique of NSM will vary from surgeon to surgeon; however, there are technical details that will be common to all. The choice of incision will be based on surgeon and patient preference but also upon tumor location. In general, the majority of NSMs are preformed through an inframammary incision but can also be performed through a vertical incision extending from the inferior areolar edge to the inframammary fold (IMF), a lateral incision from the lateral areolar edge to the anterior axillary line, as well as a supra-areolar incision either at or slightly above the areolar edge. Figures 16-1 to 16-3 illustrate a woman following NSM through an inframammary incision.
Tumors that are located laterally or superolaterally are typically approached through a lateral incision. Another advantage of this incision is in the unfortunate event that the NAC has to be removed due to positive margins. In this case, the lateral incision is extended around the NAC
in an elliptical fashion. In the event of a positive NAC margin following the IMF approach for the NSM, excision of the NAC is usually performed vertically, thus creating an inverted T incision. Figures 16-4 to 16-6 illustrate a woman following NSM and postoperative radiation.
in an elliptical fashion. In the event of a positive NAC margin following the IMF approach for the NSM, excision of the NAC is usually performed vertically, thus creating an inverted T incision. Figures 16-4 to 16-6 illustrate a woman following NSM and postoperative radiation.
 FIGURE 16-1 Preoperative photograph of a woman with right breast cancer scheduled for unilateral nipple-sparing mastectomy through an inframammary incision. |
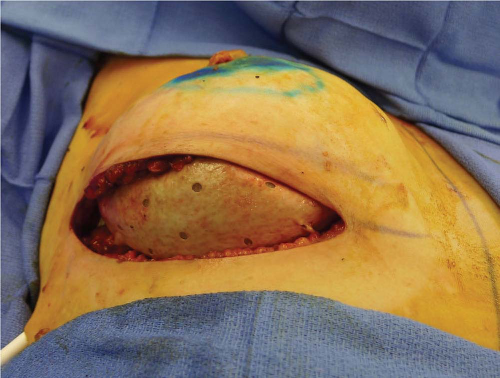 FIGURE 16-2 Intraoperative photograph demonstrating the inframammary approach with a prepectoral prosthetic device. |
 FIGURE 16-3 Postoperative photograph following excellent volume and contour symmetry with nipple viability. |
The decision making for NSM is more complex in the setting of mammary hypertrophy or severe breast ptosis. In these patients in whom the risk of nipple areolar necrosis is high, alternative strategies can be considered and discussed preoperatively. They include performing a mastopexy or oncoplastic reduction mammaplasty prior to NSM, preserving the NAC on a de-epithelized inferior dermal mastectomy skin flap, and free nipple graft. The preoperative discussion points will be elaborated upon.
 FIGURE 16-5 Postoperative image 1 month following right radiation therapy.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





