Gender-Affirming Surgery
Katherine M. Gast
William M. Kuzon Jr
DEFINITION
Gender dysphoria is the incongruence between anatomic sex and gender identity. It is estimated to affect 1.4 million Americans, or about 0.3% of the population. Male-tofemale transsexualism is 2 to 3 times more prevalent than female-to-male transsexualism.
ANATOMY
Male
Penis—superficial to deep (FIG 1)
Skin
Dartos (superficial) fascia
Buck (deep) fascia
Neurovascular bundle: deep dorsal vein, dorsal artery, paired dorsal penile nerves
Tunica albuginea (surrounds each corpus individually)
Erectile tissue: paired corpora cavernosa, corpora spongiosum surrounds the urethra
Arterial supply
Internal pudendal artery branches into the perineal artery to the perineum and scrotum.
Common penile artery branches to the bulbourethral artery, dorsal artery, and deep cavernosal artery.
Female (FIG 2)
Clitoris and clitoral hood
Labia minora and labia majora
Urethral meatus, just anterior to vestibule and introitus
Vagina
PATHOGENESIS
Considerable evidence now supports a biological basis for determining one’s gender identity.1,2,3,4. Gender dysphoria remains a diagnosis in the DSM-5. It is noted that it is not a mental disorder requiring psychiatric treatment but an incongruence between the biologically determined gender identity and the patient’s anatomic sex.
There are two separate types of gender dysphoria.
Gender dysphoria of adolescence and adulthood (ICD10 302.85) often begins in early childhood and persists into adolescence and adulthood.
It is important to recognize that gender dysphoria of childhood (ICD10 302.6) is distinctly different. In the majority of these children, gender dysphoria is temporally limited and they will “desist” by adolescence.
Because these two scenarios appear to be distinct, considerable expertise is required to diagnose and treat gender-expansive children.
When gender dysphoria of adolescence and adulthood is confirmed, puberty suppression is now the standard of care for young adolescents who exhibit significant distress with development of secondary sex characteristics. Puberty suppression is reversible and may or may not be followed by cross-hormone treatment.
It is also important to note that gender dysphoria is distinct from disorders of sexual development (DSD), where there are congenital anomalies of the genitalia and/or are hormonally determined abnormalities of secondary sex development.
This has been a source of confusion in the past when DSD children were often assigned the gender most congruent with their anatomy or with the anatomy most easily reconstructed surgically.
This resulted in inappropriate assignment of gender with patients opting to surgically transition to their natal gender later in life. These patients were not gender dysphoric.
The management of patients with anomalous genitalia or hormonal development requires specialized, multidisciplinary expertise, and patients presenting with a selfreported diagnosis of DSD require appropriate evaluation and referral.
PATIENT HISTORY AND PHYSICAL FINDINGS
Since plastic surgeons are not trained in the evaluation and management of gender dysphoria, internationally accepted standards of care (SOC) have been published by the World Professional Association for Transgender Health (WPATH). It is imperative that surgeons performing gender-affirming surgery are familiar with these guidelines and that they have in place mechanisms to assure that patients have met SOC before becoming surgical candidates.
Collaboration with local mental health providers who are familiar with this area is the most practical way of assuring the validity of the letters of readiness required by the SOC.
If that is not practical, then the surgeon must accept the responsibility of vetting the patient’s preparation for surgery, including compliance with SOC.
The WPATH SOC clinical guidelines address primary care, hormonal therapy, mental health services, and surgical treatment of transgender patients.
For chest surgery, patients must have one letter of readiness from a mental health professional, and 1 year of estrogen therapy is recommend for breast growth in male-to-female patients who desire breast augmentation.
For genital surgery, or “bottom” surgery, patients must have two letters of readiness, have completed 1 year of hormonal therapy, and have completed 12 months of a “real-life experience” of living in congruent gender in all circumstances.
Ongoing, regular visits with a mental health professional are recommended. The WPATH SOC are meant to be flexible guidelines and may be modified for individual patients.
Physical exam of male-to-female patients should document circumcision status, presence of any inguinal hernia, and examination of the testicles and spermatic cords. The central perineum must be examined for hair growth since this impacts surgical decision-making as described below.
Physical exam of female-to-male patients should focus on the suitability of free flap donor sites suitable to provide tissue for phallic construction. The radial forearm flap is the most common donor site, so an Allen test of bilateral upper extremities is important. Since the flap must be double rolled into a phallus, the thickness of subcutaneous tissue of the radial forearm flap, the anterior lateral thigh flap, and the superficial circumflex iliac perforator flap should be documented.
IMAGING
No diagnostic or radiologic studies are indicated.
SURGICAL MANAGEMENT
Penile Inversion Vaginoplasty
Preoperative Planning
Hair removal: For male-to-female patients undergoing vaginoplasty, electrolysis or laser hair removal must be performed to remove hair of the perineum from anus to base of penis in midline of the scrotum. The reason for this is the perineal flap is used to widen the introitus and line the inferior posterior aspect of the neovagina.
The perineal flap can be defatted and follicles scraped from the dermis, but this compromises blood supply of the tissue.
In the event of a rectal injury, well-vascularized tissue over the direct repair is advantageous to prevent rectovaginal fistula.
Hormone cessation: Estrogen therapy must be held 3 to 4 weeks prior to surgery. Estrogens are increase risk of perioperative thromboembolic disease. Hormones are resumed postoperatively when packing is removed and it can be determined that the patient will not require a repeat trip to the operating room. Spironolactone therapy may continue through the perioperative period.
Bowel prep: A standard bowel prep to cleanse the colon and rectum of stool is performed the day prior to surgery. The patient is kept on a clear liquid diet 24 hours prior to surgery and then nothing by mouth for 6 hours prior to general anesthetic. In the event of a rectal injury, a repair is more durable if stool is not encountered immediately postoperatively.
Positioning
Patient should be positioned in standard lithotomy position with sequential compression devices on bilateral lower extremities and pressure points appropriately padded. Arms can be tucked at patient’s sides with padding at elbow and wrist.
Patient should be prepped with Betadine including the lower abdomen, penis, scrotum, buttocks, and perineum.
Approach
Penile inversion vaginoplasty with the penis skin tube lining the neovagina is the most commonly performed technique worldwide. The neovagina is often lengthened with full-thickness skin graft (FTSG) from the scrotum to a goal length of 14 to 16 cm in the operating room. The scrotal skin is fashioned into the labia majora. A portion of the dorsal glans penis is left on a dorsal neurovascular pedicle to create a sensate neoclitoris. Prepuce skin of the penis may be used to construct the labia minora in uncircumcised patients.
Sigmoid colon vaginoplasty is a technique by which a segment of the colon is harvested by a general surgeon, secured to the sacrum to prevent prolapse, and then brought down into the pelvis and connected to the perineal reconstruction. Diversion colitis, excessive mucous discharge, and prolapse of the intestinal segment limit its widespread adoption as a primary method of vaginoplasty.
TECHNIQUES
▪ Penile Inversion Vaginoplasty
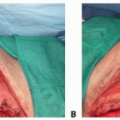
Creation of the Perineal Flap
The perineal flap is located anterior to the anus centered along the midline. The base of the flap is 3.5 cm wide and the flap is 10 cm in length. The flap is triangular shaped and is incised and raised ventral to dorsal with a 1-cm layer of subcutaneous fat, leaving it pedicled posteriorly adjacent to the anus (TECH FIG 1A). A vertical incision is then made through the scrotum up to the penile-scrotal junction. Dissection is carried down to the level of the bulbocavernosus muscle. The bulbocavernosus muscle is dissected free from overlying tissue along its length.
A Foley catheter is placed.
The origins of the bulbocavernosus muscles from the ischia are identified and dissected bilaterally circumferentially (TECH FIG 1B). The base of the bulbocavernosus muscles are clamped and divided on each side; 2-0 Vicryl suture ligatures are employed to control bleeding.
The prerectal space is then dissected by dividing the plane between the bulbocavernosus and anal sphincter. Sharp dissection through the perineal body using cautery is used initially to the level of the urogenital diaphragm (TECH FIG 1C).
Once the prerectal plane is entered, sharp and then blunt dissection is employed using digital dissection and a sponge stick following the Foley catheter.
At the level of the prostate, the rectoprostatic fascia (Denonvilliers fascia) is detached from the tail of the prostate, and dissection proceeds anterior to Denonvilliers. This is done bluntly with the aid of a sponge stick, which is advanced slightly and then swept from anterior to posterior. Dissection is carried out to the level of the peritoneum, approximately 15 cm in depth.
A moist sponge is placed in the neovaginal space. The rectum is filled with half-strength saline-Betadine solution. After 2 minutes, the laparotomy sponge is removed and inspected for Betadine. Bimanual examination with one finger in the rectum and one in the prerectal dissection and direct visualization of the anterior rectal wall is performed to ensure that no rectal injury occurred. The prostate is palpated and any abnormalities noted.
The levator ani muscles are incised for about ½ cm on each side to widen the space for the neovagina.
Orchiectomy
Bilateral orchiectomies are then performed in the usual fashion. The testicles are dissected free from the scrotal tissue in the plane just superficial to tunica vaginalis.
The spermatic chords are dissected to the external inguinal ring.
The vas deferens is separated from the remainder of the chord and ligated separately with 2-0 Vicryl ties, and the chord is suture ligated with 2-0 Vicryl at the level of the external ring. Careful attention must be paid to avoid retraction of bleeding vessels within the cord into the inguinal canal. The testicles are sent for pathologic examination.
Degloving of the penile shaft
Two centimeters proximal to the corona, the skin is incised circumferentially and the shaft of the penis is degloved in a plane just superficial to the Buck fascia with Metzenbaum scissors. The prepuce or dorsal penile skin is left adjacent to the glans to serve as a clitoral hood and may be used to construct labia minora in patients who have not undergone circumcision. The penis is degloved to its base, and the penile shaft is pulled through the incision in the perineum used to raise the posterior flap.
Raising the Neurovascular, Neoclitoral Flap
A “clitoral” flap is now raised from the dorsal area of the glans. A section of dorsal glans penis is marked out in an appropriate shape at the terminus of the dorsal neurovascular bundle. In addition, a portion of the distal dorsal and lateral penile skin is kept intact to serve as a clitoral hood. The 1-cm-wide portion of the glans will serve as the future neoclitoris. This may be shield shaped or M shaped and coned at inset.
The neurovascular bundle consisting of the dorsal penile arteries, veins, and nerve is raised as a flap by dissecting them off the underlying corporal bodies. Dissection is begun at the midshaft of the penis, incising the Buck fascia along the midaxis of the penis on either side. Dissection is carried to the level of the tunica albuginea.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree