Key Points
- ▪
Exponential increase in interest in lymphedema surgery will continue to define new surgical techniques and improve effective treatment protocols.
- ▪
Combination of surgical and nonsurgical treatment protocols may prove useful in treatment protocol efficacy.
- ▪
Patient-centered outcomes, such as quality of life parameters and patient satisfaction should be included as outcome measures when validating treatment protocols.
- ▪
Emerging technologies in the diagnosis and treatment of lymphedema will improve future treatment plans and methods.
- ▪
Surgical prevention of lymphedema using microsurgical techniques may eliminate the chronic and debilitating morbidity of symptomatic lymphedema.
Introduction
Lymphedema Milestones in Diagnosis and Treatment
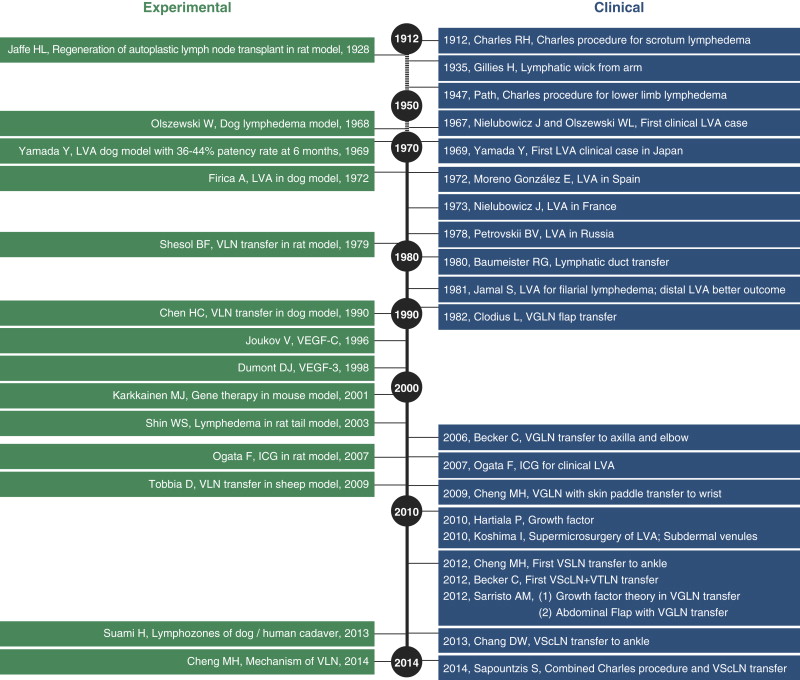
The surgical and microsurgical treatment of lymphedema is rapidly evolving with new techniques, improved outcomes reporting, and descriptions of more effective treatment strategies. Moving forward within the specialty, a thorough understanding of previous developmental milestones related to anatomy, basic science research, diagnosis, and multimodal treatment will help to refine future development pathways. There are 210 publications relating to lymphedema from 2003 to 2013 queried on PubMed as of April 20, 2014, including 35 on lymphovenous anastomosis (LVA), 26 on physiotherapy, 23 on risks/causes, 20 on quality of life, 15 on vascularized lymph node (VLN) transfer, 14 indocyanine green (ICG) studies, and 13 on diagnosis, among others. The milestones for the development of lymphedema research and the significant reported clinical experiences in the surgical treatment and microsurgical approaches are comprehensively described in the previous chapters and summarized in Figure 24.1 . Rapid recent research interests and clinical inquiry are notable along the timeline of events. In addition, the circulation of normal lymphatic fluid with the available principles of lymphedema surgery is briefly outlined in Figure 24.2 . These surgical approaches can be categorized into two groups:
- 1.
nonphysiologic methods including partial (liposuction or wedge excision) and total excision techniques
- 2.
physiologic methods, including LVA and VLN transfer.
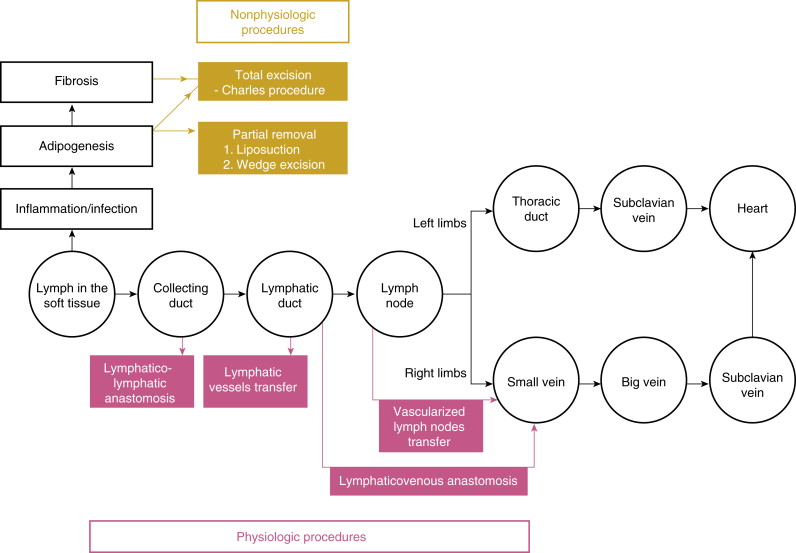
From this schematic, one can learn the physiology of these surgical procedures, and choose the right procedure for the appropriate patient, with the ability to have an effective outcome. Nonphysiologic procedures may decrease the lymphatic fluid production load and remove byproducts of excess lymph fluid, but likely require lifetime compression garments to prevent recurrence of lymphedema and excess limb volume. In correctly selected patients, physiologic procedures may allow for the elimination of compression garments, which has a significant impact on quality of life. As the specialty continues to define surgical success, factors outside of limb circumference changes will become increasingly important to recognize. The overall goal of all lymphedema surgical procedures is to improve patient functionality and quality of life. Patient-reported outcome measures may have a greater impact on the definition of surgical success. Development of a comprehensive and multifactorial outcomes assessment method will not only allow individual physicians to define success in their individual practice, but will create a common language between specialties to facilitate improvements in multidisciplinary patient care delivery.
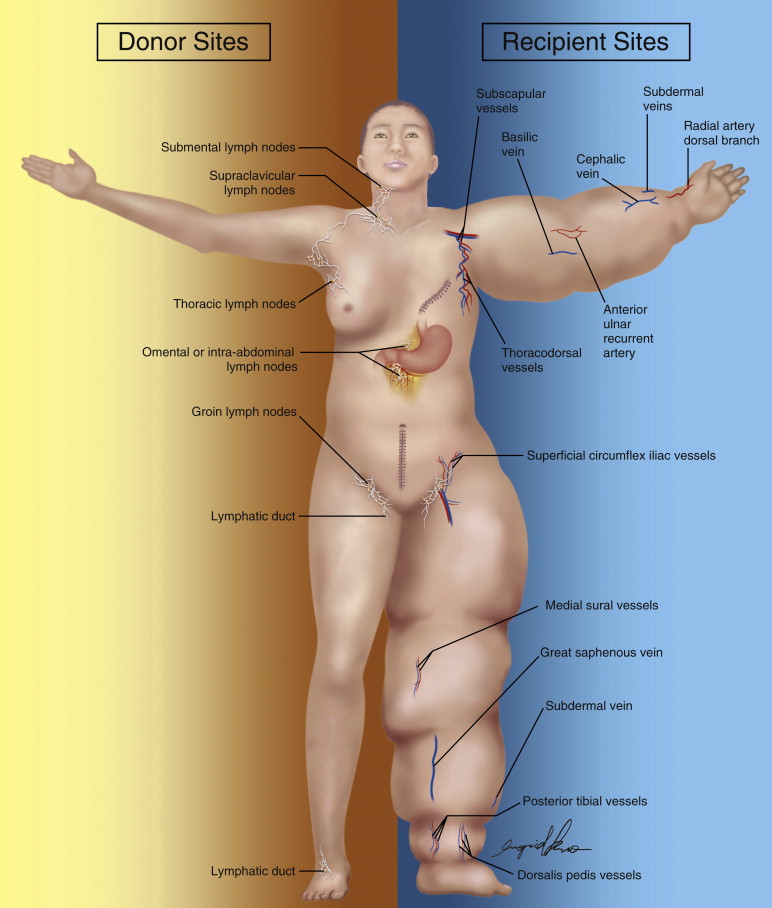
The available evidence-based surgical treatment options are summarized in Figure 24.3 . The right body half represents available donor sites and the left body half shows available recipient sites for microsurgical procedures. As our understanding of lymph node basins and physiologic processes related to these procedures expand, increasing options will become available. More studies and improved methodologies regarding donor site morbidity and the indications and outcomes of various lymph node transplantation procedures are mandatory. Recipient sites for both microsurgical procedures are outlined as well. The functional subdermal venules are most available in the forearm and wrist close to the cephalic vein in the upper limb, or on the leg and ankle close to the great saphenous vein in the lower limb for LVA. And, experience has shown that there are variable recipient sites available for VLN transfer on the lymphedematous limb. Combined procedures in lymphatic microsurgery have also been introduced as an effective way to provide maximal patient benefit in fewer surgeries. Although adding layers of complexity to these surgeries, less recurring operative morbidity may result in higher quality of life and increased functional recovery. Further critical evaluation of these techniques will shed light on to their effectiveness.