The wrist consists of eight carpal (wrist) bones interposed between the forearm (radius and ulna) and the five metacarpal bones. The carpal bones may be divided into two rows of four bones each.
The proximal carpal row is composed of (from radial to ulnar) the scaphoid, lunate, triquetrum, and pisiform.
The distal carpal row is composed of (from radial to ulnar) the trapezium, trapezoid, capitate, and hamate.
Provided minimal bony constraint, the carpus is supported by the intrinsic (originate and insert within the carpus) and extrinsic (originate or insert outside the carpus) ligaments.
Within each row, adjacent bones are held together with intrinsic interosseous ligaments, while the rows of bones are connected by large capsular radiocarpal and intercarpal ligaments.
The specific ligaments comprising the proximal row interosseous ligaments are the scapholunate and lunotriquetral interosseous ligaments. Each is “C” shaped, covering the dorsal, proximal, and palmar regions of the respective joints.
The interosseous ligaments can be divided into three regions, each with unique gross and histologic as well as mechanical characteristics.
The dorsal region of the scapholunate interosseous ligament is a true ligament. It is the thickest and strongest region and constrains translation between the scaphoid and the lunate.
The palmar region of the lunotriqeutral ligament shares these characteristics.
The palmar region of the scapholunate interosseous ligament is also a true ligament. It is thin and constrains rotation (flexion-extension, pronationsupination) between the scaphoid and the lunate. The dorsal region of the lunotriquetral interosseous ligament shares these characteristics.
The proximal regions of the scapholunate and lunotriquetral ligaments are composed of fibrocartilage and are believed to function as menisci, absorbing compressive loads along the proximal rims of the articulations.
Extrinsic ligaments
Along the volar side of the wrist from radial to ulnar, the ligamentous elements include radioscaphoid and long and short radiolunate ligaments. These ligaments extend from the radial side of the radius and extend obliquely ulnarward to attach to elements of the proximal and distal carpal row.
The dorsal extrinsic ligament (the counterpart of the palmar ligaments) is the dorsal radiotriquetral (dorsal radiocarpal) ligament, which originates at the junctional raphe between the scaphoid and lunate fossa and extends obliquely across to attach to the lunate and triquetrum. This ligament shares a common attachment on the triquetrum with the dorsal, intrinsic, scaphotriquetral ligament (dorsal intercarpal ligament).
Palmarly and ulnarly there is a relatively superficial ligament, the ulnocapitate, which arises near the fovea and extends obliquely to the side of the capitate. Two ligaments arise from the volar limbus of the triangular fibrocartilage complex (TFCC), the so-called ulno-lunate and ulnotriquetral ligaments.
These ligamentous elements form dorsal and palmar V-shaped ligaments that support the carpus and are directly perpendicular to forces that favor carpal dissociation from the radius. The arrangement of these ligaments puts them in a position to act as a supportive sling for the carpus, and resist translation under load especially with the arm in an extended position and with the forearm in neutral rotation. This is the position in which most power activities are performed. When the supportive sling mechanism is lost, radiocarpal dislocation can occur. The dislocations may be purely ligamentous; however, avulsion fractures that contain ligament origins off the dorsal or volar radial rim of the radius are commonly present.
The wrist and distal radioulnar joint (DRUJ) combine to form essentially a universal joint, normally capable of stable motion with six degrees of freedom in the cardinal planes (flexion, extension, radial deviation, ulnar deviation, pronation, and supination). Combining these motions results in circumduction. Many consider the “dart throw” axis as the most functional motion in the wrist, which combines radial deviation and extension through ulnar deviation and flexion. In general terms, the center of rotation can be thought of as being in the head of the capitate.
Overall, the bones of the distal carpal row are tightly bound to each other, creating essentially a single functional unit.
The bones of the distal row move with the hand through all six degrees of freedom.
The proximal carpal row behaves differently.
First, there is significant motion between adjacent bones as the entire row moves in generally the same direction. This is similar to the behavior of train cars traveling as a group down a railroad track, but exhibiting some independent motion through their couplings.
The proximal carpal row bones move with the distal row bones during flexion and extension of the wrist (adjunct rotation) but continue to experience flexion and extension during radial and ulnar deviation of the wrist, respectively (conjunct motion). This occurs because the scaphoid is shaped and positioned within the wrist such that any extrinsic loading will induce flexion.
The triquetrum, on the opposite side of the proximal row, will experience extension when loaded.
The lunate simply moves with the dominant direction of its neighbors, as long as the intrinsic interosseous ligaments are intact.
Wrist radial deviation is accomplished with flexion of the proximal carpal row as the scaphoid flexes allow wrist to deviate without distraction of the ulnar carpal articulations.
Wrist ulnar deviation comprises primarily of proximal row extension with engagement of the hamate in the triquetrum and extension of the scaphoid as the trapezium and trapezoid move away from the distal radius.
Associated injuries may include fractures of the distal radius and radial head. Scaphoid fractures may also be seen in perilunate injury patterns. When a scaphoid fracture is present in association with lunocapitate and lunatotriquetral instability, the injury is termed trans-scaphoid perilunate instability. Similarly, when a scaphoid fracture is present in association with a capitate fracture and triquetrolunate instability, the injury is termed trans-scaphoid, trans-capitate perilunate instability or scaphocapitate syndrome.
Fracture nonunion and avascular necrosis (AVN) is more common in proximal pole fractures, given the retrograde blood supply to the proximal aspect of the scaphoid.
The scaphoid occupies a position in both the proximal and distal carpal rows. It is almost completely covered in articular cartilage and has no tendinous attachments.
Morphologically it can be divided into proximal and distal thirds (poles), and a central third termed the waist.
The blood supply to the scaphoid can be divided into two main anatomic regions.
The dorsal scaphoid branches of the radial artery enter the bone through the nonarticular dorsal ridge and the distal tubercle, supplying 70% to 80% of the bone, including the proximal pole. As a result, the blood supply to the proximal pole of the scaphoid is retrograde, which is the main reason why the more proximal fractures are susceptible to developing AVN following a fracture.
A second group of vessels arising from the volar scaphoid branches of the radial artery enters via the scaphoid tubercle to supply the distal 20% to 30% of the bone. This flow is typically anterograde, which explains why the more distal fractures have a tendency to heal uneventfully.
Patients typically present with wrist pain that is localizable to the anatomic snuffbox on physical examination. Careful attention should be paid to the radial head in the elbow and the distal radius to rule out any associated injuries.
The radiographic evaluation should include PA, lateral, and ulnar deviation (scaphoid) views of the wrist. For evaluation of the distal pole, a carpal tunnel view or a semisupinated lateral view can be helpful. The sensitivity of fracture detection with the standard radiographic series in the acute setting is moderate, and pronation and supination oblique views may increase this sensitivity.
Patients with a history and clinical examination suggestive of fracture but negative initial radiographs should be treated empirically in a thumb spica splint or cast, followed by repeat radiographs in 7 to 10 days. If repeat films are also negative and the clinical suspicion for a fracture remains, further studies such as computerized tomography (CT) or magnetic resonance imaging (MRI) should be considered.
Assessment of fracture healing can also be problematic. CT scans are a valuable adjunct obtained prior to the discontinuation of immobilization if union is in question.
Classification: Scaphoid fractures can be classified by location and chronicity, as both have significant implications with regard to prognosis. Fracture pattern also has some prognostic significance, as oblique or vertical fractures are known to be more difficult to treat than their horizontal counterparts.
Scaphoid fractures are broadly considered unstable if
Fracture displacement of greater than 1 mm is present
Fracture angulation—scapholunate angle greater than 60 degrees (normally 30 to 60 degrees), or radiolunate or capitolunate angle greater than 15 degrees (normally -25 to +10 and 0 to 15 degrees, respectively) is present and/or
Fracture comminution is present
the intrascaphoid angle is greater than 45 degrees, and
there is an associated intercarpal ligament tear (i.e., trans-scaphoid perilunate fracture dislocation)
Stable distal pole fractures should be immobilized in a short- or long-arm thumb spica cast for about 6 weeks, at which time radiographic union is often observed.
Stable waist fractures can be managed in a long-arm thumb spica cast for 6 weeks followed by short-arm thumb spica casting for another 6 weeks or until radiographic union is achieved. The long-arm cast prevents forearm rotation and felt to decrease healing time.
Stable proximal pole fractures are difficult to treat in a closed manner, and may require as long as 20 weeks to heal without operative intervention.
Stable fractures in which the diagnosis has been delayed but which do not display evidence of nonunion may be treated with a trial of cast immobilization.
Any fractures treated with immobilization should not be considered healed until there is definite evidence of osseous bridging, which is best assessed with CT scan.
Unstable or displaced fractures typically require surgical fixation. Surgical options include closed reduction and percutaneous pinning, closed reduction and percutaneous headless compression screw fixation, and ORIF with a headless compression screw.
Distal pole fractures are best approached volarly, while proximal pole fractures are best approached dorsally. Fractures of the waist of the scaphoid can be approached from either dorsal or volar (or both). Union is most predictably achieved with a single compression screw placed beneath the articular surface.
Arthroscopic assisted or open reduction may be required depending on displacement and comminution. Primary bone grafting should be considered in comminuted fractures. Surgical fixation and bone grafting should be considered for fractures not healed after 3 to 4 months of closed treatment.
Recently, surgical fixation of stable or nondisplaced scaphoid waist fractures has been advocated, although to date the outcomes of nonoperative and operative treatment of nondisplaced scaphoid fractures appear similar, with each method having advantages and disadvantages.
With proper management, nearly 100% of distal pole fractures, 80% to 90% of waist fractures, and 60% to 70% of proximal pole fractures go on to bony union. Delay in diagnosis by more than 1 month is associated with a higher incidence of nonunion.
Patients with fracture nonunion typically present with wrist pain with or without a specific history of trauma.
Radiographically, nonunion is characterized by sclerosis, cyst formation, flexion (humpback) deformity of the scaphoid due to the flexed posture of the distal fragment, and dorsal intercalated segment instability (DISI) deformity of the wrist in the more chronic cases. This change in carpal mechanics as a result of scaphoid nonunion leads to a recognizable pattern of articular degeneration of the wrist joint termed the SNAC (scaphoid nonunion advanced collapse) wrist.
Establishing the presence of proximal pole AVN can be difficult preoperatively. Vascularity of the proximal pole can be assessed preoperatively with gadolinium-enhanced MRI scans or intraoperatively by assessing the presence of punctate bleeding from the proximal pole.
Symptomatic fracture nonunions can be treated with cancellous, corticocancellous, or vascularized bone grafting in conjunction with internal fixation (headless compression screw).
Nondisplaced nonunions can be treated with corticocancellous grafting from a volar approach (Russe technique)
Displaced nonunions with a humpback deformity require the placement of a corticocancellous volar wedge graft from a volar approach to correct the humpback deformity.
For proximal nonunions or those in which the proximal fragment has developed AVN, volar grafting techniques are contraindicated. In the absence of fragmentation and presence of structural integrity of the proximal pole
at the time of surgery, reconstruction in the form of ORIF and bone grafting should be attempted. With the use of ORIF and conventional bone grafts, only about half of scaphoid nonunions with proximal pole AVN will go on to heal. Local vascularized bone grafts can be used for the treatment of scaphoid nonunions complicated by AVN. The distal radius vascularized bone graft based on the 1,2 intercompartmental supraretinacular artery is used commonly. Other grafts that have been described include
A vascular pedicle originating from the second dorsal intermetacarpal vascular bundle, which is directly implanted into the nonunion site.
Vascularized bone grafts from the distal radius based on a pronator quadratus pedicle, among others. While vascularized bone grafting initially generated great interest, results of longer-term follow-up of nonunions treated with this technique remain less than ideal.
Vascularized free graft from the medical femoral condyle
In the presence of fragmentation and absence of structural integrity of the proximal pole at the time of surgery, salvage procedures such as fragment excision with intercarpal arthrodeses, or proximal row carpectomy are typically recommended.
Types of instability
Carpal instability dissociative refers to instability within a carpal row; scapholunate or lunotriquetral ligament tears. This involves an intrinsic ligament injury, and leads to counterrotation between the radial and ulnar components of the carpal row.
Carpal instability nondissociative (CIND) occurs when the bones within each carpal row are normally constrained but support has been lost either between the rows or between a row and its neighboring structure (i.e., midcarpal instability). Extrinsic ligaments are most likely injured in this case.
Carpal instability complex incorporates each of the above elements and denotes marked loss of ligamentous support (i.e., perilunate dislocation).
Carpal instability adaptive describes the unstable carpus occurring as a result of pathology proximal or distal to the carpus itself (i.e., a malunited distal radius fracture).
Degree of instability
Static: When the carpus is malaligned (i.e., scaphoid excessively flexed) on resting radiographs, the ligamentous injury has likely compromised both primary and secondary restraints at a given joint.
Dynamic: When resting radiographs are normal but stress views demonstrate intercarpal widening (i.e., scapholunate diastasis on grip radiograph) a dynamic instability is diagnosed.
Predynamic: In the predynamic state, patients report pain or tenderness that corresponds to an injured ligament but all imaging is normal (i.e., pain over the scapholunate ligament but normal resting and grip radiographs).
Lunate posture
Dorsal intercalated segmental instability (DISI) refers to abnormal lunate extension seen on lateral radiographs. This most commonly is associated with scapholunate ligament tears, which free the lunate from the flexion moment that the scaphoid imparts.
Volar intercalated segmental instability (VISI) describes abnormal flexion of the lunate on lateral radiographs. This most commonly occurs with disruption of the lunotriquetral ligament, which releases the lunate to flex with the scaphoid, and can also occur with generalized ligamentous laxity leading to a CIND pattern.
Ulnar translocation and dorsal translocation of the carpus involve displacement of the carpus as a unit with the lunate moving in the direction specified.
Force transmission
Greater arc injuries involve an arc of injury that is transmitted through, and fractures, the involved carpal bone (i.e., trans-scaphoid perilunate dislocation).
Lesser arc injuries involved purely soft tissue injury and can disrupt multiple ligamentous structures without fracture.
Chronicity
Acute (<1 week)
Subacute (1 to 6 weeks)
Chronic (>6 weeks): Primary ligament healing unlikely
Etiology
Traumatic
Indirect forces applied to the outstretched, extended hand are most commonly responsible for carpal instability.
Mayfield et al. (1980) described the accepted sequence of perilunar instability
Stage 1: Scapholunate ligament tear or scaphoid fracture
Stage 2: Capitolunate dissociation
Stage 3: Lunotriquetral ligament tear or triquetral fracture
Stage 4: Dislocation of the lunate
Nontraumatic (i.e., chronic inflammatory arthritic degeneration as in rheumatoid arthritis)
History: Patients with carpal instability can present with wrist pain, weakness, or loss of motion. Some experience a high energy trauma to the upper extremity while others with subtle instability often recount a lower energy injury that may have involved a seemingly benign fracture (Chauffeur-type, or distal radius styloid fracture).
Physical examination: A detailed wrist examination is performed bilaterally as the asymptomatic wrist offers an excellent control for the comparison of motion, joint laxity, and symptoms produced on provocative testing (up to 20% of asymptomatic wrists demonstrate a clunk on scaphoid shift test).
Inspection for malalignment or signs of acute trauma (swelling and ecchymosis).
Assess forearm, wrist, and digital motion. “Clicks” or crepitus should always be correlated with pain reproduction.
Note degree of ligamentous laxity (i.e., elbow/digit hyperextension).
Grip and pinch strength
Palpate ligaments of wrist
Selective provocative testing
Scaphoid (Watson) shift test (for scapholunate ligament tear)
Place examiner’s thumb on the palmar surface of the patient’s distal pole of the scaphoid
Place the examiner’s index finger over the dorsal surface of the scapholunate joint
Passively move the patient’s wrist from ulnar deviation to radial deviation while applying a dorsally directed force on the distal pole of the scaphoid
A positive response is dorsal pain with detection of dorsal subluxation of the proximal pole of the scaphoid.
Lunotriquetral shuck (Regan and Linscheid): Grasp the pisotriquetral column between the examiner’s thumb and index finger with one hand, and stabilize the lunate with the other hand. Translate the pisotriquetral column anteriorly and posteriorly, estimating the magnitude of translation.
Lunotriquetral shear (Kleinman): Grasp the pisotriquetral column between the examiner’s thumb and index finger with one hand and passively move the wrist through radial/ulnar deviation with the other, looking for assymetrical displacement patterns of the triquetrum.
Lunotriquetral compression (Linscheid): Apply compression (medial to lateral) across the LT joint, assessing for pain.
Lichtman test: To diagnose midcarpal instability, axial compression is applied to the hand and the wrist is brought from radial deviation into ulnar deviation. As this occurs, the proximal row produces a clunk as it rapidly attains the extended posture that it failed to gradually obtain during the motion (“catch up” clunk).
Imaging is helpful, but must be interpreted carefully, knowing that a spectrum of normal conditions exist.
Posteroanterior and lateral radiographs of the wrist are absolutely necessary, and most useful when combined with comparison views of the contralateral wrist.
Both must be taken in a standard position, such that the third metacarpal is collinear with the longitudinal axis of the radius.
Calculation of specific angles on lateral radiographs can be determined by use of the axis of the specific carpal bone as demonstrated in Figure 14.1 and Table 14.1.
On the PA radiograph (in neutral radial-ulnar deviation and with the hand and wrist flat on the x-ray plate), one should look for the disruption of Gilula lines, defined as the normally continuous arches created by connecting the images of the subchondral lines of the proximal surfaces of the proximal carpal row, the distal surfaces of the proximal carpal row, and the proximal surface of the distal carpal row.
Gaps between adjacent bones may be significant if asymmetrical.
Additionally, dynamic changes may be created with motion of the wrist or application of load through grip.
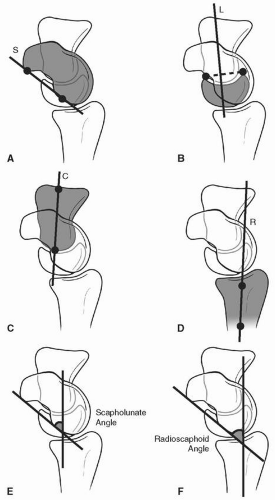
Figure 14.1 Method for determining carpal angles from lateral radiograph: A: The scaphoid is outlined along the volar aspect with a line between the most volar portion of the proximal and distal poles. B: The axis of the lunate is determined by a line perpendicular to the line connecting the dorsal and volar distal aspects. C: The axis of the capitate is determined by a line connecting the center of the proximal and distal articular surfaces. D: The radius is determined by a line perpendicular to its distal third. Commonly used carpal angles: E: Scapholunate F: Radioscaphoid. (Reprinted with permission from Glickel SZ, Barron OA, Catalano LW III. Green’s Operative Hand Surgery, 5th Ed. Philadelphia, PA: Elsevier, Churchill Livingstone; 2005, Fig. 14-12, p. 537.)
TABLE 14-1 Normal measurements for intercarpal angles
Joint Relationship
Normal (degrees)
Standard Deviation (degrees)
Radiolunate
0
±10
Radioscaphoid
47
±32
Scapholunate
47
±32
Other imaging may be of use on a case-specific basis, including arthrography, MRI (with or without a gadolinium arthrogram component), live fluoroscopy, radionuclide scintigraphy, and ultrasound.
Arthroscopy offers a unique opportunity for evaluation of the status of the carpus and, most typically necessitate observation in both the radiocarpal and midcarpal joints. Geissler et al. (1996) have devised a classification scheme (Table 14.2) based upon the midcarpal appearance of the proximal row joint clefts and have correlated these features with grades of ligament disruption. Care must be taken, however, to view these findings in the light of normal laxity.
Computed tomography may identify subtle avulsion fractures.
MRI is of variable sensitivity and specificity for identifying carpal ligamentous injury with usefulness that varies both with the quality of the scanner and interpretive experience of the surgeon and radiologist.
MRI arthrography may increase the test’s accuracy.
TABLE 14-2 Arthroscopic classification for intercarpal (scapholunate and lunatotriquetral) ligament injuries | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Scapholunate dissociation (SLD)
Dissociation of the scaphoid and lunate represents the most common form of carpal instability.
This injury occurs most commonly as the result of axial loading in a wrist positioned in dorsiflexion, ulnar deviation, and intercarpal supination.
Patients often have pain over the scapholunate ligament palpated 1 cm distal to Lister tubercle. The Watson shift test may be positive in acute cases.
Once uncoupled, the scaphoid tends to excessively flex and the lunate extends (DISI) resulting in an increased scapholunate angle and a “cortical ring sign” on a PA radiograph as the distal scaphoid is now being imaged in line with its longitudinal axis. Additionally, radiographs may show a diastasis greater than 3 mm between the scaphoid and lunate, implying dorsal intercarpal ligament separation from the lunate.
Power grip radiographs may identify dynamic instability produced by rupture of the scapholunate interosseous ligament with preservation of secondary stabilizers.
Chronic scapholunate diastatis produces progressive arthritic degeneration termed scapholunate advanced collapse (SLAC).
Stage 1: arthritis at the radial styloid
Stage 2: arthritis of the entire scaphoid fossa of the distal radius
Stage 3: arthritis of the capitolunate articulation
Treatment
Acutely diagnosed tears of the scapholunate interosseous ligament are treated surgically. A dorsal ligament repair through bone tunnels or with suture anchors can be performed and supplemented by K-wire fixation of the scapholunate and scaphocapitate joints. Generally, protective fixation is maintained for 2 to 3 months.
Partial tears not responding to conservative treatment may be debrided arthroscopically.
Chronic injuries are generally less amenable to direct ligament repair and are approached with either a dorsal capsulodesis (especially with dynamic instability, but less reliably in cases of fixed instability), a tenodesis (such as the Brunelli reconstruction using the FCR), bone-ligament-bone reconstruction, or limited carpal arthrodesis (i.e., scaphotrapezial and scaphocapitate).
Once arthritic changes are present at the radial syloid-scaphoid joint, a radial styloidectomy may be considered (Stage 1 SLAC) while more advanced arthritis often necessitates proximal row carpectomy, scaphoid excision and four corner fusion, total wrist fusion, or total wrist arthroplasty.
Specific x-ray findings
It is important to recognize that dynamic SLD may appear normal under standard static x-ray examination.
Motion series or grip views of the wrist may unmask a dynamic subluxation of the scaphoid or a diastasis between the scaphoid and the lunate. Fluoroscopy may also be useful to detect dynamic instability patterns.
TABLE 14-3 Treatment for scapholunate ligament injuries based on arthroscopic grading
Geisler Grade
SLAC
I
II
III
IV
I
II
III
Pins
+ (1)
+ (1)
+ (2)
+ (2)
Direct repair
+ (3)
+ (3)
+ (4)
Reconstruction
+ (2)
+ (3)
+ (4)
Augmentation
+ (5)
+ (5)
+ (5,6)
+ (5,6)
Partial arthrodesis
+
+ (7)
+
+
+
Salvage
+ (7)
+
+
As the severity of the dissociation increases, more static changes can be detected radiographically.
The scaphoid can assume a more flexed (or vertical) posture. This results in an increasingly exaggerated radioscaphoid and scapholunate angle on lateral radiographs.
The scaphoid will appear foreshortened in a PA x-ray, and a “cortical ring sign” may appear where the cortex of the vertical scaphoid appears more radiodense.
In advanced SLD, the lunate may be extended in an otherwise neutrally positioned wrist, and the carpus may have collapsed height due to the capitate migrating proximally and dorsally on the extended lunate.
The lunate may be excessively ulnarly translated, where over 50% of the proximal surface may be located ulnar to the level of the lunate fossa.
Treatment (Table 14.3)
Optional
As part of additional procedure
Only if scapholunate relationship is easily reducible
Accompanied by very limited radial styloidectomy, if painful
Some prefer adding capsulodesis to any approach for SLD
Higher-grade SLD treatment may be augmented with the insertion of a headless screw across the scapholunate joint (Reduction and Association of Sacphoid and Lunate (RASL) procedure) or dorsal ligamentoplasty using a strip of tethered dorsal intercarpal ligament.
If scapholunate relationship is difficult to reduce
Lunotriquetral dissociation
Lunotriquetral ligament injuries occur less commonly than scapholunate ligament injuries and occur as a result of a fall axial loading in a wrist positioned in dorsiflexion, radial deviation, and intercarpal pronation.
Patients may present with pain on the ulnar side of the carpus and demonstrate positive provocative signs as described previously.
Radiographs may be normal or demonstrate a VISI posture of the lunate. More subtle findings may include the disruption of Gilula lines.
Wrist arthroscopy greatly aids in diagnosing lunotriquetral injuries with the midcarpal portals allowing a clear assessment of any dissociation between the bones.
Lunotriquetral ligament injures have been treated in a variety of fashions. The ligament has been repaired, reconstructed, and the lunotriquetral articulation arthrodesed. Shin et al. (2001) reported superior results for ligament repair and reconstruction compared to arthrodesis.
Dynamic instability, which by definition requires provocation to be problematic, most likely occurs with disruption of only the lunatotriquetral ligament. Static instability, which has fixed radiographic features of scaphoid and lunate flexion and/or triquetral dorsiflexion (VISI deformity) implies lunotriquetral ligament disruption and dissociation of the dorsal radiocarpal ligament from the lunate.
Diagnosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





