Fractures and Dislocations: Hand
Robert M. Baltera
Hill Hastings II
Kavi Sachar
Surasak Jitprapaikulsarn
I. Open Fractures/Antibiotics
Open fractures of the distal phalanx in an immunocompetent host with intact circulation can be treated with irrigation and debridement alone. Open fractures of other bones in the hand should be treated with antibiotics in addition to irrigation and debridement. Betadine has been shown to interfere with osteoblastic function in laboratory models. Fractures that are delayed greater than 24 hours in treatment, which are grossly contaminated, or present in a host with multiple systemic diseases (particularly diabetes, peripheral vascular disease, cancer patients undergoing treatment, and various infectious disease states, i.e., AIDS) should be treated with a third-generation cephalosporin. An aminoglycoside should be added for crush injuries, and penicillin should be added for farm injuries and bite wounds.
II. Distal Phalanx Fractures
Distal phalanx fractures can be separated into those involving the distal tuft, the shaft, and the articular surface of the DIP joint.
Tuft fractures can be classified as either simple (single fracture line) or comminuted (multiple fracture planes). Tuft fractures that are nondisplaced, regardless of the amount of comminution, can be treated with splinting alone, as even a fibrous union can give stability for the nail bed. Rarely, these fractures require fixation with small guage Kirschner wires (K-wires) to provide a stable bed for an associated nail bed repair. Tuft fractures that involve an open wound do not require any antibiotics and can be treated with aggressive debridement alone.
Nail bed injuries
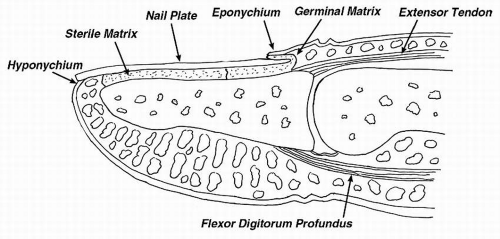
The nail bed is composed of the germinal matrix, the distal extent of which can be identified by the white lunula visible under the proximal aspect of the nail, and the sterile matrix, the red tissue visible under the remaining aspect of the nail. The germinal matrix provides 90% of the nail growth, while the sterile matrix is mainly responsible for adherence of the nail. The proximal nail is covered by the eponychium, the tissue overlying the lunula (Fig. 13.1). The eponychium, or roof of the nail fold, provides the cells that produce the shine of the nail. The hyponychium is the area of keratinized skin at the distal edge of the nail, providing a barrier against infection. The paronychium is the folds of skin overlying the lateral edges of the nail. This is the area most susceptible for infection.
Any displaced tuft fracture or nail avulsion is an indication of a nail bed injury and should be explored surgically with removal of the nail and repair
under loupe magnification with fine resorbable suture. Repair of the nail bed often facilitates reduction of the underlying bony fragments and vice versa. The germinal matrix can be better visualized if necessary by 1-cm incisions starting at the proximal lateral nail fold and angled perpendicular to the nail fold (Fig. 13.2). After repair, the placement of a nonadherent dressing in the nail fold prevents adherence of the germinal matrix to the roof of the nail fold. This
dressing can be left in place, allowing the new nail to force out the gauze over time. If the nail plate is available, it can be placed back into the nail fold after nail bed repair to act as a splint for the underlying fracture as well as a spacer to keep the nail fold open.
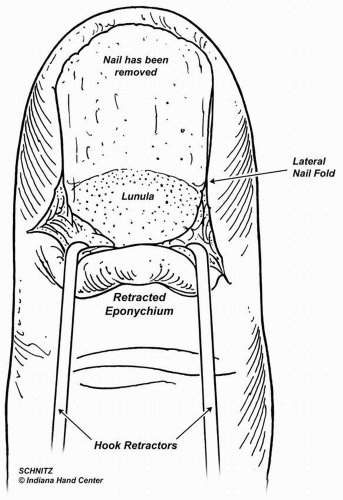
Figure 13.2 Incisions extending proximally from the radial and ulnar corners of the proximal lateral nail fold for exposure of the germinal matrix.
Subungal hematomas, unless accompanied by nail avulsion from the nail fold or displaced fracture, can be treated nonoperatively. Cautery or a large bore needle through the nail plate can be used for symptomatic relief but is not necessary. A subungual hematoma involving greater than 50% of the nail may require nail plate removal and repair of the nail bed injury.
Distal phalanx shaft fractures
Fractures of the shaft are classified by their direction, either longitudinal or transverse, and their nature, either stable or unstable. Unstable fracture, i.e., those in which the displacement or angulation cannot be corrected with closed reduction, should be treated with small gauge K-wires, either two 0.028 in or one 0.035 in, preferably not crossing the DIP joint.
Bony mallet fractures
Fractures of the dorsal base of the proximal aspect of the distal phalanx can occasionally lead to subluxation of the distal phalanx volarly. Closed reduction and percutaneous transarticular K-wire fixation of the subluxated distal phalanx to the middle phalanx is recommended. Anatomic reduction of the displaced fragment is possible with fracture fixation or extension block printing. Open reduction is required infrequently when treated acutely. If there is no subluxation of the distal phalanx, closed splinting is adequate.
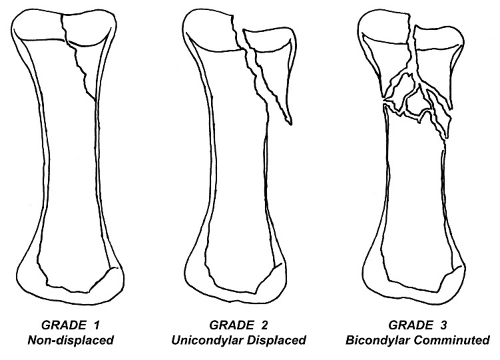
Fractures of the DIP
Fractures of the middle phalanx extending into the DIP joint have been classified by London into three grades. (Fig. 13.3) Grade I is a nondisplaced unicondylar fracture. Grade II is a displaced unicondylar fracture, and Grade III is a bicondylar comminuted fracture. Grade I fractures can be treated in a splint for 3 weeks followed closely with weekly x-rays. The splint is then discontinued and protected motion, i.e., buddy-taped to the adjacent digit, for an additional 2 to 3 weeks. Grade II injuries are by definition displaced and should be reduced and fixed with K-wires or screws. Grade III injuries are comminuted, bicondylar fractures. They are usually the result of direct trauma, and the degree of comminution often makes anatomic reconstruction impossible.
III. Middle Phalanx Shaft Fractures
Fractures of the middle phalanx shaft are classified by their stability and fracture geometry, i.e., transverse or oblique. Nondisplaced fractures and fractures that are stable after reduction can be treated with a short period, i.e., 3 weeks, of immobilization of the proximal interphalangeal (PIP)/DIP joints leaving the MP joint free. They should be followed with weekly radiographs to ensure that alignment is maintained. Protected range of motion is then instituted for an additional 2 weeks by buddy-taping to an adjacent digit. Acceptable parameters for nonoperative treatment include no clinical malrotation of the digit and no angulation greater than 10 degrees in any plane. Rotation is best determined clinically with the digit in full flexion. Digital block should be used for pain control as needed in the office to permit evaluation for rotational malalignment with active flexion.
Oblique fractures tend to be unstable and to shorten, even after a good reduction is obtained. Very little shortening is tolerated at this level because the extensor mechanism cannot adjust, leading to an extensor lag at the DIP joint. Treatment of oblique, comminuted, and open fractures involves internal fixation. While crossed K-wires can often be done without open reduction, it is difficult to mobilize the finger because of tethering of soft tissue until the K-wires are removed, often at 3 weeks after surgery. Lag screws and plate fixation allow earlier range of motion, but the hardware can irritate the tendons, and an additional surgery may be required to remove the hardware and/ or release adhesions. Decreased range of motion, however, is reported in over 50% of all fractures, regardless of fixation techniques. Early motion, then, is essential to a good outcome; and stable fixation is necessary to allow immediate mobilization.
IV. Fracture and Dislocation of the Proximal Interphalangeal Joint
PIP joint stiffness or ankylosis is poorly tolerated and significantly impairs grasp and activities that require fine dexterity. Injuries to the PIP joint are challenging to treat due to technical difficulties in handling small articular fragments, the tendency for stiffness following injury and surgery, and residual controversies regarding optimal treatment.
Anatomy and biomechanics
Bony anatomy
The PIP joint is a hinge joint allowing 100 to 110 degrees of motion in the sagittal plane and minimal motion in the axial and frontal planes.
The head of proximal phalanx is composed of two concentric asymmetric condyles separated by an intercondylar sulcus. The dorsal margin of each condyle is roughly half the width of the volar margin. The ulnar condyle projects further distal than the radial condyle in small finger, is shorter in the index and middle fingers, and both condyles are of nearly equal length in the ring finger. The longer projecting condyles have a greater radius of curvature. In the coronal plane, the articular surfaces tilt away from the second web space. These features provide a rotational component to the motion of each finger, allowing the tips to converge toward each other in flexion.
The base of middle phalanx consists of biconcave articular surfaces separated by a central ridge. The radius of curvature of the surface is slightly greater than that of the reciprocal proximal phalangeal surface imparting a small degree of sloppiness to the hinge.
The volar aspect of the base has two thickened lateral corners and two lateral tubercles to which portions of the collateral ligaments attach.
The palmar base of the middle phalanx is critical for joint stability and provides buttressing support to resist dorsal subluxation.
Soft tissue structures
The Volar plate is a swallow tail-like (tapering in two limbs proximally) strong fibrocartilaginous structure covering the volar aspect of the joint.
Origin—Thin attachment continuous with the periosteum of proximal phalanx, synovial reflection, C1 pulley, and A2 pulley
Insertion—Thicker strong lateral fibers attach to the lateral corner of the base of middle phalanx. Thinner central fibers blend with the volar periosteum
Function
First restraint to hyperextension
Second restraint to lateral stability
Provides mechanical advantage to the flexor tendons by increasing their moment arm
Collateral ligaments
Proper collateral ligament
Origin—The pit on the lateral side of head of proximal phalanx
Insertion—The thickened lateral corner of the base of middle phalanx along its entire volar 40%, volar plate (only most volar fiber)
Function—First restraint to lateral stability
Accessory collateral ligament
Origin—Lateral side of the head of proximal phalanx palmar to the proper collateral ligament origin
Insertion—Lateral edge of volar plate
Function—Very little role in joint stability. Prevents the volar plate from redundancy and allows the base of middle phalanx to move along the corresponding surface as the joint flexes.
The volar plate and the two collateral ligaments form a “box” or “chariot” configuration acting in concert to provide PIP joint stability. Dislocation can occur if this complex fails at least two planes.
Injuries to PIP joint
Dislocation with or without fracture
Dorsal dislocation
Volar dislocation
Lateral dislocation
Isolated fracture
Fracture of head of proximal phalanx (detailed under Proximal Phalangeal Fracture section)
Intra-articular fracture of base of middle phalanx
Dorsal base fracture
Volar base fracture
Avulsion of collateral ligament insertion
Volar lateral plateau compression fracture
Pilon fracture
General treatment principles
The PIP joint has great propensity to develop stiffness following injury, surgery, and prolonged immobilization (especially >3 weeks). Inappropriate or delayed treatment usually results in stiffness, chronic pain, and posttraumatic arthritis.
Re-establishing and maintaining the concentric stable reduction and early mobilization are the crucial factors for the good functional outcomes. If technically feasible, anatomical reduction of articular surface should be obtained.
Dorsal dislocation
Most common joint dislocation of the hand
Mechanism of injury—combination of hyperextension and some degree of axial load
Classification
Type I—Hyperextension injury— Partial or complete avulsion of volar plate (usually from distal insertion)
Type II—Pure dorsal dislocation—Avulsion of volar plate and bilateral splitting of collateral ligaments
Type III—Fracture-dislocation—dislocation with volar base fracture
Kiefhaber modification of Hastings classification
Stable fracture-dislocation
Less than 30% articular base of middle phalanx Congruent through full range of motion
Tenuous
30% to 50% articular base of middle phalanx, reduces with less than 30 degrees flexion
Unstable
Mote than 50% of A-P diameter or less than 50% but requires more than 30 degrees PIP flexion to maintain reduction
Diagnosis
AP and lateral views of the entire finger are obtained. On the perfect lateral x-ray, the two condyles of the proximal phalanx should be superimposed upon each other. In fractures, partially pronated and supinated obliques should also be obtained.
Subtle subluxation can be missed easily. The features on the lateral view that confirm a perfect concentric reduction are
Absence of dorsal “V sign” (divergence of dorsal articular surface)
The center of head of proximal phalanx is aligned with the axis of middle phalanx in all positions
Treatment
Hyperextension injury
Acute injury Extension block splint in slightly flexed position 1 to 2 weeks
Chronic injury—Presenting with PIP hyperextension or swan neck deformity in the absence of chronic mallet finger
Treatment—Volar plate reattachment or flexor digitorum superficialis (FDS) tenodesis
Pure dorsal dislocation
Closed reduction and immobilization in slightly flexed position 1 to 2 weeks
Dorsal Fracture-Dislocation
The important factors for determination of treatment are
Size of volar fragment; Less than 30% of A-P diameter implies stable; more than 50% of A-P diameter implies unstable
Comminution of volar fragment
Degree of PIP flexion required to maintain reduction (>30-45 degrees)
Treatment options
Stable and tenuous stability
Extension block splinting—Motion of PIP and DIP joints can be initiated immediately. The wrist is splinted in 20 to 30 degree extension, the metacarpophalangeal (MCP) joint in slight flexion, and the PIP joint blocked in 10 to 20 degrees greater flexion than the point of demonstrated instability. It is critical to secure the proximal phalanx up to the splint to prevent its sag, which effectively will lead to PIP extension.
Advantage—Easy to do, monitor, and convert to another form of treatment
Complications are mostly salvageable
Disadvantage—Difficult to apply in too short, small, or swollen digits
Complication—resubluxation, late flexion contracture
Unstable
Extension block pinning—Extension block pinning can be use in the short, small, or swollen digit that precludes application of extension block splint
Transarticular pinning
Simple technique—Difficult to determine its efficacy because of a small number of cases reported
Open reduction and internal fixation
Indication—Unstable fracture-dislocation with simple fragments large enough to accommodate implant devices
Surgical approach—Both volar and dorsal approaches have been described
Implant devices—Miniscrew (1.1-1.5mm), K-wire, tension band wire
Nearly full restoration of motion possibile
Complication—Stiffness, flexion contracture, posttraumatic arthritis, and infection
External fixation
A variety of devices in both static and dynamic modes include wire fixator such as Agee force-couple, push traction; pin and rubber band or pin and spring traction systems such as Suzuki traction; the customized external fixator; the commercial external fixator
Principle—Provide distraction force across joint
Reduce fracture fragments via ligamentotaxis
Provide volar-directed force on the middle phalanx in certain systems
Allow immediate PIP motion
Do not reduce depressed articular fragments (especially central fragments)
Indication—Unstable fracture-dislocation with single fragment or comminuted fracture. Can be used as adjunct to internal fixation
Contraindication—Fracture of head of the proximal phalanx
Satisfactory results can be expected in acute injuries with precise application of the fixator, concentric reduction, and early range of motion.
Complication
Loss of reduction upon fixator removal
Pin traction infection
Joint stiffness
Articular incongruity
Volar plate arthroplasty
Principle—Resurface the damaged articular surface of the middle phalanx with vascularized fibrocartilaginous tissue and provide a volar buttress to maintain joint stability. To be successful, the volar plate should be adequately filled with the volar defect to prevent recurrent subluxation
Indications—Acute unstable fracture-dislocation especially with comminuted or impacted volar fragment
Chronic fracture-dislocation of PIP joint
Certain cases of osteoarthritis (OA) with a viable dorsal articular surface
Many series reported satisfactory results from this procedure especially in acute injuries. With greater than 40% articular involvement, results are unpredictable.
Complication
Recurrent subluxation; One of the causes is articular involvement exceeding 40% and residual volar defect inadequately filled by the volar plate. Consider hemihamate resurfacing arthroplasty (HHRA) or filling the residual bony defect with a slip of FDS or bone graft in acute cases, or osteotomy in chronic cases.
Flexion contracture—most common complication
DIP stiffness
Angular deformity
HHRA
Principle—Restore an osteocartilaginous buttress and replacement to the palmar base of middle phalanx with a contour-matched portion of the ipsilateral dorsal hamate
Indications
Acute unstable fracture-dislocation especially with comminuted or impacted volar fragment
Chronic fracture-dislocation of PIP joint
Comminuted lateral plateau fracture of the base of middle phalanx
Salvage after failure of previous surgery
Severe injuries involving >50% of the articular surface, in which volar plate arthroplasty is unfeasible
Contraindication—Fracture of dorsal articular surface.
Reported satisfactory results in a few intermediated-term studies
This is an attractive procedure for the treatment of this difficult fracture-dislocation.
Volar dislocations
These are uncommon injuries but can lead to late deformities because of unrecognized diagnosis. Central slip injury is relatively common in volar dislocation of PIP joint. It can be easily missed and then lead to late boutonniere deformity. In the patient presenting with semiflexion of PIP joint after trauma, the differential diagnosis should be included for central slip rupture and volar plate injury.
Injuries can be classified into
Simple volar dislocation
Pathology—Bilateral disruption of collateral ligaments, volar plate, and occasionally rupture of central slip
Treatment
Closed reduction
Reducible
No extension lag of PIP joint: Short-time immobilization Extension lag of PIP joint (usually unstable): Open repair of central slip
Irreducible: Open reduction
The obstacles to reduction usually are interposed central slip or collateral ligament
Volar fracture-dislocation
The factors that determine the treatment are
The size of dorsal fragment and
Fracture displacement
Volar fracture-dislocation with small dorsal fragment (<20% of articular surface) and less than 2 mm displacement can be treated with PIP joint splinting as in closed boutonniere injury.
Volar fracture-dislocation with large dorsal fragment (>20% of articular surface) or more than 2 mm displacement can be treated with open reduction and screw or wire fixation. Internal fixation may be supplemented by external fixation when fixation is tenuous and instability is substantial.
Volar rotatory dislocation
Pathology
Rupture of volar plate and a collateral ligament
A condyle of head of proximal phalanx is encircled between the central slip and the lateral band
Treatment
Closed reduction
Reducible
No extension lag of PIP joint: Short-term immobilization Extension lag of PIP joint: Splinting as in closed boutonniere injury
Irreducible—Open reduction and central slip repair
Lateral dislocation
Rare injury of PIP joint
The injury involves the rupture of a collateral ligament and volar plate
Treatment
Lateral dislocation usually reduces spontaneously or is easily reduced by closed means. Finger buddy splint with early motion is recommended
Open repair or reconstruction of collateral ligament may be considered in certain high-performance patients such as athletes, manual laborers, or cases with chronic painful PIP instability
Isolated dorsal base fracture
An avulsion involves the insertion of central slip
As in volar dislocation, missed or untreated injuries may be a prelude to boutonniere deformity
Treatment
Small fragment (<20% of articular surface) and less than 2 mm displacement: Splint as in closed boutonniere injury
Large fragment (>20% of articular surface) or more than 2 mm displacement → open reduction and screw or wire fixation
Isolated volar base fracture
An avulsion involves the insertion of volar plate into the base of middle phalanx
Usually less than 10% of articular surface
Treatment
Finger buddy splint with early motion is enough
If the PIP joint represents the tendency to hyperextend, extension block splint in neutral is recommended (as the treatment of hyperextension injury)
Avulsion of collateral ligament insertion
Treatment—Nonoperative treatment with finger buddy splint for less than 3 weeks is preferred for nondisplaced fracture
For the prevention of late lateral stability in significantly displaced fracture, ORIF with miniscrews, K-wires, or tension band wire should be considered.
Volar lateral plateau compression fracture
Result of an eccentric axial load that causes articular depression and metaphyseal impaction—The A-P and lateral x-ray may miss the articular depression. An oblique view can usually show this depression.
Treatment—Nonoperative treatment may result in angular deformity and residual pain
Recommended treatment is ORIF with K-wires or screws and bone grafting
Comminuted intra-articular fracture (pilon fracture)
From axial loading injury, depressed and comminuted central articular surface and complete seperation of volar and dorsal articular surfaces from diaphysis. Treatment
The goal of treatment is to reassociate the overall architecture of the base of middle phalanx, realign the axis of middle phalanx on proximal phalanx both sagittal and coronal planes, and allow early motion. Anatomical reduction is usually infeasible and less important.
The patient should be informed about inevitable stiffness and posttraumatic arthritis.
Nonoperative treatment usually results in suboptimal outcome.
Operative treatments include
V. Fracture of Proximal Phalanx
Fractures of the proximal phalanx are common; however, inappropriate treatment may result in extensor tendon adhesions, joint stiffness, malunion, and decreased function.
Normal anatomy
The proximal phalanx has a straight to slightly convex dorsal cortex that is thicker than the concave volar cortex. Longitudinal crests on the medial and lateral margins of the volar surface correspond to A2 pulley insertion on each side.
The proximal phalanx is totally surrounded by mobile tendons except over a small volar lateral area. The close relationship of the extensor mechanism provides support for fractures but is also prone to extensor adhesions by its coverage.
Pathoanatomy and pathophysiology
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree