Fractures and Dislocations: Elbow
Michael Darowish
Jesse B. Jupiter
Graham J.W. King
Kevin J. Malone
Jeffrey N. Lawton
The stability of the elbow joint is a result of primarily the bony anatomy. There are two articulations at the elbow and as a result, there are two arcs of motion.
The ulnohumeral joint resembles a hinge joint and permits flexion and extension at the elbow.
The radiohumeral and proximal radioulnar joints allow for axial rotation that results in pronation and supination of the forearm.
I. Functional Anatomy (Fig. 16.1)
Osseous components
The ulnohumeral is one of the most confined and inherently stable joints in the body.
The trochlea is surrounded 180 degrees by the trochlear notch.
The distal humerus tilts 30 degrees anteriorly and the trochlear notch tilts posteriorly in the sagittal plane. This relationship has implications for stability and motion:
The coronoid process resists posterior translation of the forearm in both flexion and extension.
Elbow flexion is enhanced.
The relatively large width of the trochlea and the olecranon enhance varus and valgus stability.
The radial head articulates with the proximal ulna forming the proximal radial ulnar joint (PRUJ).
The radial head resists both posterior translation of the forearm and resists valgus stress.
Capsuloligamentous components
The medial collateral ligament (MCL) and the lateral collateral ligament (LCL) are the main capsuloligamentous stabilizers of the elbow.
The MCL complex has three discrete components.
The posterior bundle originates from the inferior aspect of the medial humeral epicondyle and courses distally to the medial joint line along the sigmoid notch of the ulna (essentially a thickening of the joint capsule).
The anterior bundle is the most distinct and structurally important component. It also originates from the inferior aspect of the medial humeral epicondyle. It courses distally and anteriorly to insert on the medial aspect of the coronoid on the sublime tubercle. This bundle is tight in extension and is an important stabilizing structure of the medial elbow against the type of valgus stress that is created in an overhead throwing motion or a fall onto an extended elbow.
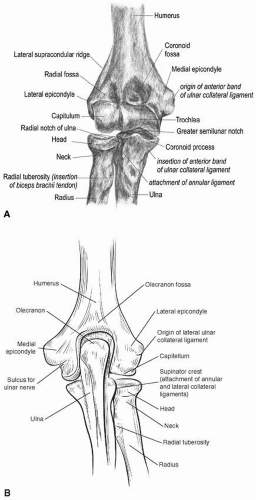
Figure 16.1 A and B Morphlogy of the elbow. Anterior and posterior view of osseous anatomy of the elbow. (Courtesy of Leversedge FJ, Goldfarb CA, Boyer MI, and Lin M.)
The transverse component is the least important part of the MCL complex. It is a capsular thickening that runs from the medial border of the coronoid to the medial aspect of the olecranon.
The LCL complex is made up of the radial collateral ligament, the annular ligament, and the lateral ulnar collateral ligament. The LCL arises from the lateral humeral condyle at a point through which the axis of rotation passes. Because of this, it maintains a uniform tension throughout the arc of motion. It bifurcates as it extends distally.
The anterior portion is called the radial collateral ligament, and it blends with the annular ligament around the radial head.
The posterior portion is called the lateral ulnar collateral ligament and inserts onto the lateral portion of the ulna at the supinator crest. This ligament is the primary lateral stabilizer of the elbow and its compromise will result in the posterior sagging of the radial head and lateral aspect of the sigmoid notch of the ulna with respect to the capitellum and trochlea of the humerus. This condition is called posterolateral rotatory instability.
The anterior capsule and the collateral ligament complexes act as important secondary dynamic stabilizers, and contribute to resisting valgus stress.
Musculotendinous components
The biceps, brachialis, and tricep muscles help maintain the trochlea in the trochlear notch.
Together the muscles provide dynamic stability to the elbow.
Nerve relationships
The ulnar nerve runs posterior to the medial epicondyle and lies medial and deep to the olecranon process. It may be at risk by anterior and ulnar penetration of the cortex by Kirschner wires (K-wires) in a tension band technique.
The radial nerve runs along the lateral aspect, anterior to the lateral epicondyle and crosses anterior to the radiocapitellar joint.
The median nerve runs medial to the brachial artery, which lies medial to the biceps tendon. The mnemonic MAT can be used to remember this orientation from medial to lateral.
Elbow Fractures and Dislocations: Simple Elbow Dislocations
I. Anatomy
(See section on elbow anatomy at the beginning of this chapter.)
II. Definition
A “simple” elbow dislocation involves dislocation of the ulnohumeral joint without associated fractures to the radial head, olecranon, or coronoid. When these other injuries are present, the injury is termed “complex” and the treatment protocol differs. While “simple” dislocations are primarily soft tissue injuries with disruption of the secondary stabilizers, postreduction radiographs reveal periarticular fractures in up to 60% of cases and operative exploration reveals osteochondral injuries in nearly 100% of acute elbow dislocations. Without the injuries seen in the complex patterns, the primary joint stabilizers remain intact and allow for nonoperative management.
III. Incidence
Acute elbow dislocations account for 10% to 25% of all injuries to the elbow. The mechanism of injury is typically a fall onto an outstretched hand with the elbow extended and the arm abducted away from the body. The proposed sequence of events based on laboratory studies is that a combination of valgus, supination, and axial forces applied to the elbow results in a sequential failure of the soft tissues, progressing from the LCL to the anterior and posterior capsules, and finally the MCL This sequence of events has not been universally supported by clinical studies. This is typically an injury of the young adult with the median age for the injury around 30 years.
IV. Evaluation and Initial Treatment
Evaluation should include a complete assessment of the arm with particular attention to the neurovascular status.
Arterial injury or occlusion has been reported.
The motor and sensory examination of the median, ulnar, and radial nerves is determined and documented.
The wrist and shoulder are assessed for deformity or pain, as concomitant upper extremity injuries have been reported to occur in up to 15% of cases.
Radiographs in two planes should be assessed to determine the direction of the dislocation. These injuries are described by the position of the ulna in relation to the distal humerus. Approximately 90% of dislocations occur with posterior or posterolateral displacement of the ulna. The radiographs should be evaluated for associated periarticular fractures.
Attempts at closed reduction typically require adequate muscle relaxation and analgesia. There are many different described maneuvers but they all include correction of medial/lateral displacement and then application of longitudinal traction with the elbow extended followed by elbow flexion. This will allow the coronoid to be brought around the trochlea. Reduction should produce a palpable clunk.
Immediately following reduction, the elbow should be assessed for stability. It will typically demonstrate instability to valgus stress and in full extension. The neurovascular status of the arm following reduction is reassessed. Although the distal pulses may be diminished on initial examination, they often return to normal after reduction. There is a higher incidence of brachial artery lacerations with open dislocations and with complex elbow dislocations. A pulseless arm after reduction is an indication for immediate exploration. Similarly, nerve injuries are rare with simple elbow dislocations. The ulnar nerve is most commonly involved and usually resolves with time. If there is a brachial artery injury, there may be a median nerve injury as well because of their proximity.
Postreduction radiographs should be assessed for concentric reduction of the ulnohumeral, radioulnar, and radiocapitellar joints. Joint space widening may be an indication of entrapped chondral fragments or soft tissue in the joint and is an indication for exploration.
There are few indications for open reduction or immediate exploration. Open dislocations and dislocations with associated brachial artery laceration should be explored. The other indications include a joint that must be maintained beyond 50 to 60 degrees of flexion to remain reduced and a joint with suspected entrapped fragments following reduction. In the setting of persistent instability without evidence of disruption of the bony anatomy, the medial and/or the LCL complexes need to be repaired or reconstructed. Typically, the ligaments are avulsed from their humeral origin.
V. Postreduction Management
If the joint is stable following reduction and radiographs confirm concentric reduction, the elbow is placed into a splint in approximately 90 degree flexion and the forearm in full pronation (to allow healing of the LCL).
The immobilization should be discontinued in approximately 1 week and elbow motion initiated. Immobilization for longer than 3 weeks has been associated with long-term stiffness. Radiographs should be taken at 1 week to confirm maintained reduction. If the joint is still reduced, the patient can begin range of motion exercises with intermittent splinting for protection and comfort. Radiographic follow-up will typically show calcification within the anterior capsule or along the collateral ligaments, but rarely is the cause of limited motion.
VI. Results
Flexion returns first, with maximum improvement usually seen by 12 weeks. Return of extension can continue to show improvement for up to 5 months following injury. Loss of extension is the most common sequela of this injury as patients will typically lose 10 to 15 degrees of extension. As clinical studies have shown the relationship between period of immobilization and final range of motion, many authors are encouraging an earlier motion program. Despite the trend for shorter immobilization, there has not been an increase in the rate of redislocation or early instability.
Long-term follow-up studies conducted at 3 years and 24 years after injury have shown that elbow discomfort is present in up to 50% of the cases. Average flexion contracture was 12 degrees at 24 years. Greater degrees of flexion contractures were associated with longer periods of immobilization. Radiographs showed minimal posttraumatic changes with no loss of joint space.
Coronoid Fractures
I. Anatomy (see additional information at beginning of chapter)
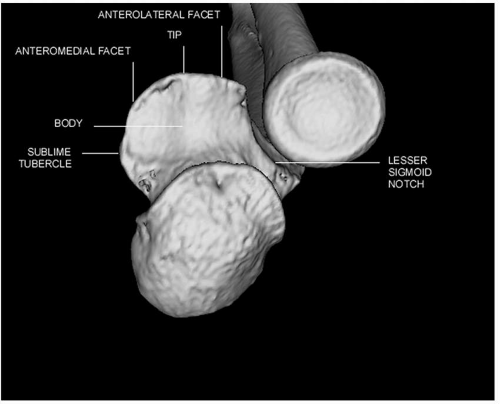
The coronoid is the anterior projection of the greater sigmoid notch of the proximal ulna (Fig. 16.2) It consists of a tip, body, anterolateral, and anteromedial facets. At the base of the anteromedial facet, the sublime tubercle provides the insertion site for the anterior bundle of the MCL. The coronoid is an important stabilizer against posterior, varus, and posteromedial rotatory instability of the elbow. Larger coronoid fractures have a greater influence on elbow stability.
II. Incidence
Coronoid fractures do not occur in isolation; consequently, their incidence is poorly documented. They are usually associated with radial head fractures, elbow dislocations, ligament injuries, or transolecranon fracture-dislocations.
III. Classification
There are two commonly employed classification systems outlining the patterns of coronoid fractures.
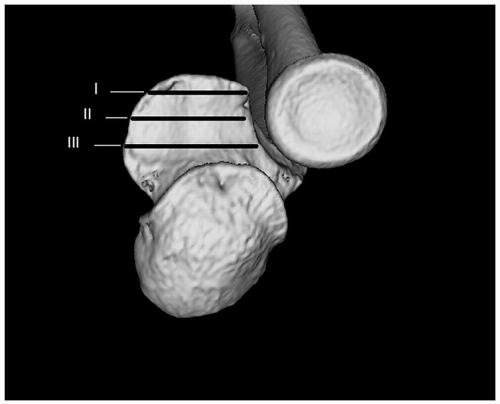
The Regan and Morrey system is based on the height of the coronoid fragment (Fig. 16.3).
Type I: Small “avulsion” of the tip of the coronoid process (typically <10%)
Type II: Includes up to 50% of the coronoid.
Type III: Involves greater than 50% of the coronoid.
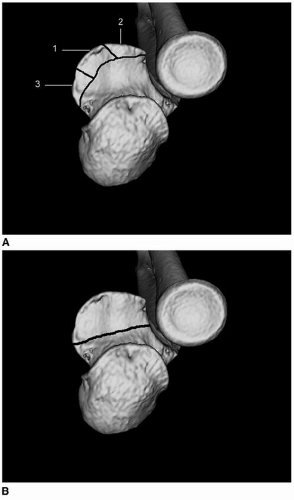
The system of O’Driscoll is based on the location of the fracture (Fig. 16.4).
The coronoid is divided into the tip, the anteromedial facet, and the base.
Coronoid tip fractures are divided into fragments that are less than or greater than 2 mm in size.
Fractures of the anteromedial facet are divided into three subtypes.
Subtype 1 anteromedial facet fractures involve the rim. They begin just medial to the tip of the coronoid and extend toward the sublime tubercle but do not involve it.
Subtype 2 fractures involve the rim of the anteromedial facet and the tip of the coronoid.
Subtype 3 fractures involve the sublime tubercle and also the rim with or without involvement of the tip of the coronoid.
Basal coronoid fractures consist of a fracture through the body of the coronoid and involve at least 50% of the coronoid height.
Subtype 1 involves only the coronoid
Subtype 2 is a coronoid body fracture in association with a fracture through the olecranon.
IV. Clinical Evaluation
A history of fall on outstretched arm is typical; however, some have a higher energy mechanism. Careful examination of both collateral ligaments and the DRUJ is needed to evaluate for associated injuries. Anteroposterior and lateral radiographs of the elbow are essential. Positive fat pad sign for a hemarthrosis may be the only radiographic finding if the coronoid fracture is small or nondisplaced. A double crescent sign is associated with anteromedial coronoid fractures. Supplementary oblique views can more accurately define the anatomy, displacement of the fracture, and any associated injuries. CT imaging is recommended for all coronoid fractures as it is difficult to visualize the pattern and magnitude of injury with standard radiographs. 3D reconstructions can assist with preoperative planning.
V. Management
The treatment of coronoid fractures is dependant on the size and pattern of fracture and the presence and severity of associated osseous and ligament injuries.
Nonoperative
Indicated for small fractures of the tip of the coronoid without associated elbow instability. The arm can be splinted for comfort for 1 week and then active range of motion exercises are initiated using a collar and cuff or splint at 90 degrees for support during the first 3 to 4 weeks. Follow-up should include clinical examination and radiographs to ensure that the range of motion progressively recovers and the elbow remains congruously reduced. If stiffness is a problem, early referral should be considered for physical therapy, with or without splinting.
Open reduction and internal fixation (ORIF).
Larger coronoid fractures should be treated with ORIF. Fixation options include suture fixation, compression screws, and headless compression screws and plates. The fixation technique chosen depends on the size the fragment(s), the pattern of injury, and the presence of comminution and osteopenia. Suture fixation is used for small, comminuted fragments while buttress plate fixation is preferred for anteromedial coronoid fractures.
Surgical approach
The surgical approach depends on the size and location of the fragment and the presence of associated injuries.
If there is a concomitant fracture of the radial head, which is to be replaced, the coronoid can be well visualized and fixed from a lateral surgical approach. Sutures or screws can be placed though the subcutaneous border of the ulna.
If the radial head is intact, fixation of the coronoid is often still possible by subluxing the elbow to obtain an adequate view.
If visualization from a lateral exposure is not adequate or if an anteromedial coronoid fracture is present, a medial approach should be employed.
Smaller coronoid fractures can be approached by splitting the common flexor origin after identifying and protecting the ulnar nerve while larger ones can be approached by working through the floor of the flexor carpi ulnaris (FCU) after transposition of the ulnar nerve, or lifting up the whole flexor pronator group off the medial elbow, as for a submuscular ulnar nerve transposition. Basal fractures with an associated olecranon fracture can often be repaired working through the exposure afforded by the olecranon fracture, with fixation achieved with lag screws placed through the plate.
VI. Rehabilitation
Immobilization of the elbow for 1 week following the initial injury or postoperatively is often helpful to control pain and swelling. Active motion of the elbow should then be initiated within a safe arc of motion. If there are associated injuries such as an elbow dislocation or collateral ligament injury, terminal extension should be avoided until muscle tone improves. Passive stretching should be avoided for 6 weeks due to a risk of heterotopic ossification. Strengthening is initiated after fracture healing is secure, typically 6 to 8 weeks postoperatively. Nighttime static progressive extension splinting can be helpful to regain terminal elbow extension.
VII. Outcome
The limited data available regarding the outcome of coronoid fractures are complicated by the presence and management of associated osseous and ligamentous injuries. Nonoperative treatment of anteromedial coronoid fractures has been documented to
have a high incidence of elbow instability and posttraumatic arthritis while ORIF has a favorable outcome. Similarly, larger coronoid fractures treated nonoperatively are complicated by a high incidence of elbow instability and arthritis. ORIF effectively restores elbow stability and good functional outcome in most patients.
have a high incidence of elbow instability and posttraumatic arthritis while ORIF has a favorable outcome. Similarly, larger coronoid fractures treated nonoperatively are complicated by a high incidence of elbow instability and arthritis. ORIF effectively restores elbow stability and good functional outcome in most patients.
VIII. Complications
Instability and stiffness are the most frequent complications following fractures of the coronoid. Late osteoarthritis is not uncommon, likely due to chondral injuries from the associated elbow dislocation and due to residual instability. Heterotopic ossification seems to be more common with repeated surgical procedures, and with associated dislocations.
Radial Head Fractures
I. Anatomy and Biomechanics (see additional information at the beginning of this chapter)
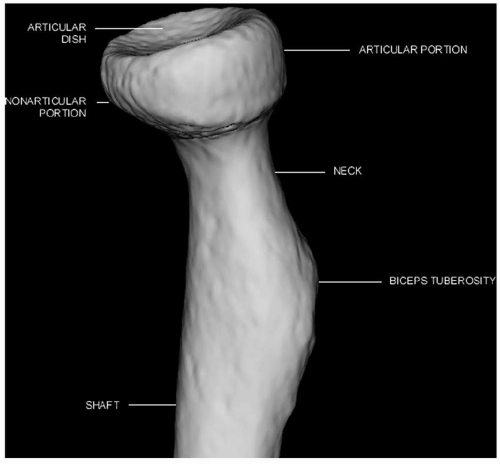
The radial head is elliptical and variably offset from the radial neck, with an articular dish that is circular and shallower than the capitellum, allowing for translation during rotation (Fig. 16.5). The articular portion is flattened with thick cartilage while the nonarticular portion is more rounded with thin or absent cartilage. About two thirds of the circumference of the head articulates with the PRUJ. The blood supply is from
capsular perforators at the head-neck junction, and through the medullary canal. Over half of the load transfer across the elbow is through the radial head, and it contributes substantially to the axial, valgus, and posterolateral rotatory stability of the elbow.
capsular perforators at the head-neck junction, and through the medullary canal. Over half of the load transfer across the elbow is through the radial head, and it contributes substantially to the axial, valgus, and posterolateral rotatory stability of the elbow.
II. Incidence
These are the most common fractures of the elbow. Radial neck fractures are more frequent in children, whereas head fractures are more common in adults. Displaced fractures usually have associated injuries of the collateral ligaments. Fractures of the coronoid, capitellum and olecranon, elbow dislocations, and ruptures of the interosseous membrane are seen concurrently with higher energy injuries.
III. Classification
A modified Mason classification most commonly employed.
Type I: Undisplaced or less than 2 mm displacement.
Type II: Displaced fracture of the head or neck without comminution.
Type III: Displaced and comminuted.
Type IV: Associated elbow dislocation.
IV. Clinical Evaluation
A history of a fall on an outstretched arm is typical; however, some may have a higher energy mechanism. Patients typically present with elbow pain, limited extension and/ or rotation, and tenderness over the radial head. Careful examination of collateral ligaments and DRUJ is needed to evaluate for associated injuries. Anteroposterior and lateral radiographs of the elbow may demonstrate a positive fat pad sign, indicating hemarthrosis (Fig. 16.6). This may be the only radiographic finding in an undisplaced
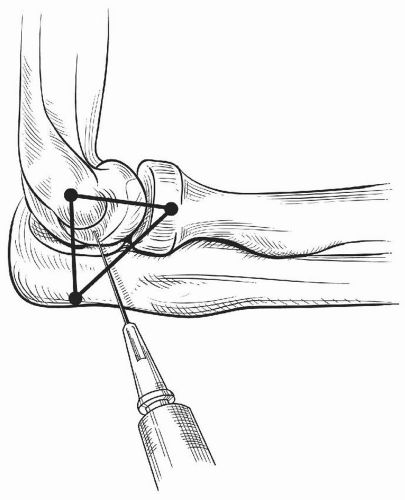
fracture. Supplementary oblique views and CT imaging can more accurately define the anatomy, displacement of the fracture, and any associated injuries. If forearm rotation is restricted, a local anesthetic injection should be performed to rule out a mechanical cause of stiffness that is not evident on radiographs. Under sterile technique, a needle is inserted into the lateral elbow at the centre of a triangle formed by the lateral epicondyle, the tip of the olecranon, and the radial head. After aspirating the hematoma, 10 cc of local anesthesia is injected into the elbow and the motion is re-evaluated (Fig. 16.7).
fracture. Supplementary oblique views and CT imaging can more accurately define the anatomy, displacement of the fracture, and any associated injuries. If forearm rotation is restricted, a local anesthetic injection should be performed to rule out a mechanical cause of stiffness that is not evident on radiographs. Under sterile technique, a needle is inserted into the lateral elbow at the centre of a triangle formed by the lateral epicondyle, the tip of the olecranon, and the radial head. After aspirating the hematoma, 10 cc of local anesthesia is injected into the elbow and the motion is re-evaluated (Fig. 16.7).
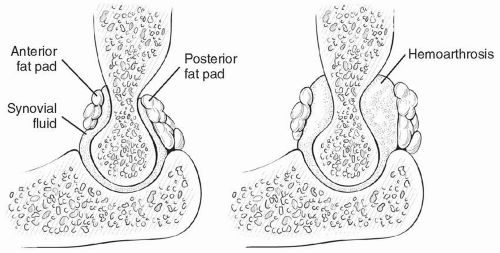 Figure 16.6 Fat pad sign. A hemarthrosis as a consequence of a radial head fracture elevates the anterior and posterior fat pads of the elbow such that they become visible on a lateral radiograph. |
V. Management
A. Nonoperative
Indicated for undisplaced or minimally displaced fractures without a block to forearm rotation. The arm splinted for comfort for a few days, and then active range of motion exercises are initiated using a collar and cuff for support for the first three to 4 weeks. Follow-up should include clinical examination and radiographs to ensure that the range of motion progressively recovers and the fracture does not displace. If stiffness is a
problem, early physical therapy should be considered, with or without splinting (either static progressive or dynamic).
problem, early physical therapy should be considered, with or without splinting (either static progressive or dynamic).
B. Fragment Excision
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree