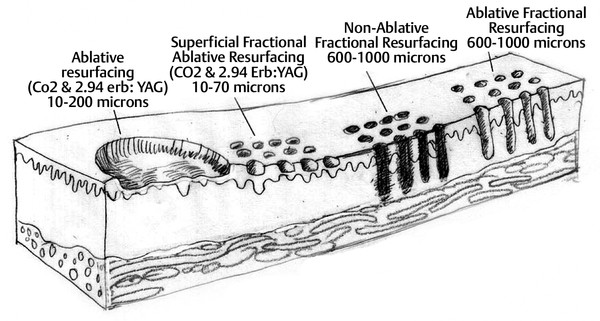
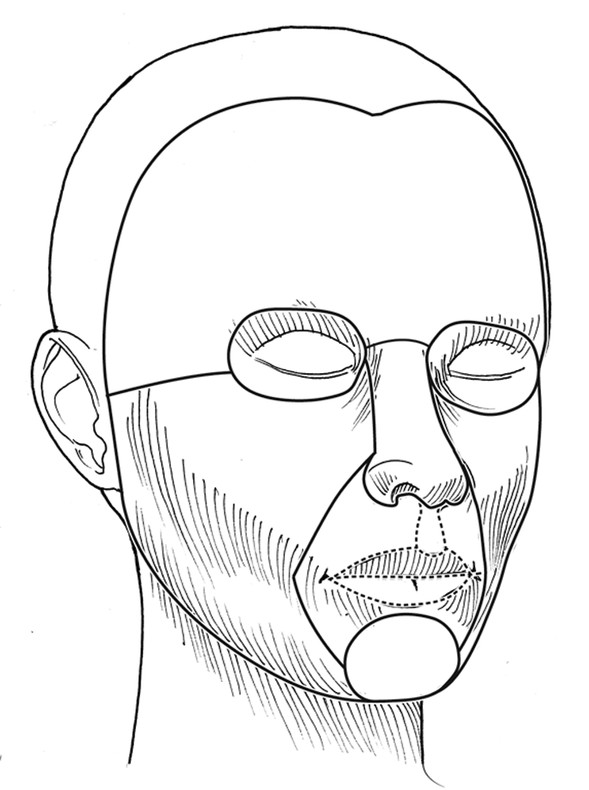
Background Fractional photothermolysis has revolutionized laser skin resurfacing by providing significant improvement in clinical results with a relatively mild posttreatment recovery. There are also lower complication rates and associated morbidity. The concept of fractional photothermolysis was first introduced by Manstein and colleagues in 2004.3 Fractional lasers differ from ablative resurfacing lasers in that ablative lasers create microcolumns with intervening zones of untreated skin. Lasered columns are created in the epidermal and dermal layers to controlled depth, width, and spacing (▶ Fig. 5.1). Fig. 5.1 The evolution of resurfacing lasers leading to fractional ablation is demonstrated in this illustration. With these untreated areas there is additional cooling by heat dissipation through the unlasered area during treatment. Interestingly, bulk dermal heating occurs under the treated and untreated areas. This bulk heating creates a cascade of histochemical effects. This is in contrast to devices that ablate the contiguous skin surface to a given depth. By ablating only columns of tissue, healing is more rapid and the potential for adverse effects such as new dyschromia, infection, scarring, and prolonged erythema is diminished. The adjacent untreated skin also allows for healing by epithelial migration from the adjacent unlasered areas. Thus, there is more rapid healing due to the benefits of the keratinocytes in the surrounding untreated skin.4 Ablative devices include the CO2 (10,600-nm), erbium:yttrium scandium gallium garnet (Er:YSGG) (2,790-nm), and erbium:yttrium aluminum garnet (Er:YAG) (2,940-nm) lasers. The chromophore or target for these lasers is water in the epidermal and dermal skin layers. These high-energy lasers instantly heat the water causing vaporization of the treated tissue with each pulse. This creates wound columns. Depending on the lasers, settings, and techniques during the first 24 hours, there can be minor bleeding, serous drainage, and/or swelling. Time to initial recovery can range from a few days to 7 to 10 days. The duration of erythema postfractional ablative resurfacing varies but typically it lasts from 3 to 7 days. Uncommonly, depending on multiple variables including individual response to the procedure, postresurfacing pinkness can last for weeks. Nonablative fractional lasers include 850- to 1,350-nm infrared, 915-nm, and 1,440-nm neodymium:yttrium aluminum garnet (Nd:YAG). These lasers are coagulative in nature, with no epidermal ablation. Recovery varies depending again on multiple variables and in general is shorter than ablative resurfacing.5 With these nonablative lasers, multiple treatments may be required to achieve the desired results and with present technology they may not be equivalent to the results of fractional ablative resurfacing. Longer wavelength, nonablative fractional lasers can be used to treat some conditions, such as scars, in patients with higher Fitzpatrick skin types (▶ Table 5.1). The anatomical subunits of the face are an important concept in all cosmetic procedures of the face (▶ Fig. 5.2). Knowledge of these helps guide the physician when deciding on a segmental area of resurfacing versus a full-face procedure. If a segmental resurfacing of the face is planned, such as rhytids in the perioral or periorbital regions, care must be taken to resurface the entire subunit for proper blending. Also certain areas of the face can be more prone to scarring such as the malar prominence, and along the jawline. The subunits can be drawn on the face prior to resurfacing to help guide the practitioner. The authors prefer not to resurface individual facial subunits, but to perform a full facial resurfacing encompassing all subunits for balance and blending. Fig. 5.2 Facial aesthetic subunits are shown in this drawing. In general when an area is resurfaced, it has less photodamage and is smoother and tighter. Even with fractional ablative resurfacing, there may be a noticeable difference between the resurfaced area and an adjacent untreated area. Therefore, if segmental resurfacing is planned, we prefer to resurface at least the entire lower or upper two thirds of the face. It is important to evaluate the characteristics of the skin when considering a resurfacing procedure. Fitzpatrick skin typing groups a patient’s skin based on sun reactivity and tanning response. Skin types I through III are usually considered resurfacing candidates because they have less pigmentation and hence less chance of dyschromia. It should be noted in patients with Fitzpatrick III skin type, if there are any olive tones to the skin there may be a greater risk of dyschromia. The authors do not routinely perform ablative fractional resurfacing on patients with Fitzpatrick skin types V and VI. Patients with Fitzpatrick skin type IV can have significant variation in skin tone. The authors only perform fractional ablative resurfacing on these patients if they have lighter skin tones. The Fitzpatrick skin type scale is listed in ▶ Table 5.1. Type I White, always burns, never tans Type II White, usually burns, tans with difficulty Type III White, sometimes burns mildly, achieves average tan Type IV Brown, rarely burns, tans with ease Type V Dark brown, very rarely burns, tans very easily Type VI Black, never burns, tans very easily Another important skin characteristic is skin thickness. As patients get older their skin gets thinner. There is also a difference in skin thickness in different locations. For example, lower eyelid skin is significantly thinner than nasal skin. The density and function of skin appendages are important and vary in different locations. In general skin heals most rapidly and with a lower rate of complications where there is the greatest number of skin appendages and optimal blood supply. Medications such as isotretinoin reduce skin appendages and can cause a healing problem. One of the most important steps in the decision to perform a cosmetic procedure is proper patient selection. Several key points should be addressed in discussions with the patient prior to the procedure: Patient concerns Pertinent medical history (Hx) Physical examination Treatment options Patient expectations Patient procedural experience Complications, as well as after care These obviously apply to every procedure we perform but some specifics to evaluation for laser resurfacing require discussion. The first step in the evaluation is patient concerns. Often it is helpful to have patients stand in front of a mirror with bright lighting, and point out the areas on the skin they would like addressed. This creates a general cosmetic skin “wish list” that really helps the practitioner understand patient desires. These commonly include rhytids, acne scarring, dyschromias, lentigines, rosacea, and actinic changes. During this dialogue, a thorough evaluation of patient skin should be performed. This includes examination of elasticity, pigment, texture, laxity, thickness, scarring, actinic change, and of course neoplastic processes. All cosmetics should have been removed prior to this portion of the evaluation. In addition, a full facial examination should be undertaken with focus on areas of concern for laser resurfacing such as previous surgical and laser procedures, skin cancer resections, radiation therapy, Accutane (isotretinoin) usage in the last year, or Hx of scar or keloid formation. Radiation therapy, isotretinoin use, scleroderma, or Hx of burns can damage the adnexal structures of the skin that are vital to skin healing because re-epithelialization is initiated from within these structures. We recommend a 12-month waiting period after cessation of isotretinoin before resurfacing. Attention should be placed on the periorbital region and Hx of blepharoplasty because even a slight lower ectropion or lid contraction can be greatly worsened by resurfacing. This can be evaluated by having the patient look upward while opening the mouth, which will reveal retraction or loss of lid elasticity. The purpose of the initial patient evaluation is gaining a clear understanding of patient expectations, and managing them accordingly. We feel it is important to explain the expected result and that results vary from patient to patient. Photos of similar patients before and after the procedure help educate patients on expected changes. Showing staged photos of patients on days 1, 2, etc., demonstrating the healing and appearance during the postprocedure period have also proven helpful. All patients are instructed to avoid sun exposure for 4 weeks prior to resurfacing and taught proper sun protection after the procedure. Preconditioning is accomplished with application of retinoic acid 0.025% cream 3 weeks prior to speed re-epithelialization.6 Hydroquinone is used 3 weeks prior to decrease potential for postinflammatory hyperpigmentation, especially in darker skin types. Hydroquinone acts to block tyrosinase that decreases the formation and increases the destruction of melanosomes within the melanocytes.7 Oral antibiotics are prescribed to start 2 days prior and continue 2 days after the procedure to diminish risk of superficial infection from skin bacterial organisms. Acyclovir is also started empirically 2 days prior at 800 mg twice daily and continued for a total of 5 days to help prevent herpes simplex virus (HSV) outbreak. Preoperative photographs are also obtained consisting of a front view and right and left three-quarter lateral views. Patients are asked to cleanse their faces before coming in for the procedure and advised not to apply any makeup, moisturizer, or other topical skin products after cleansing. Because some patients will still apply moisturizer to their faces, we always ask when they arrive. Further skin cleansing can be performed prior to the procedure with mild soap or glycolic wash. The type of anesthesia required for ablative fractional resurfacing can vary depending on the specific laser and the surgeon’s preference. The authors use a topical anesthesia regimen of 6% lidocaine and 6% tetracaine prior to the procedure. This is applied to the face and cervical region for 15 to 30 minutes. No occlusion of the topical anesthesia is used. This regimen provides a good level of anesthesia and patients are comfortable. It is then thoroughly removed. Because the lasers’ chromophore is water, the face should be completely dry prior to starting the procedure. During the procedure a chiller is used. This provides a comforting jet of cool air over the facial skin during the treatment. This increases patient comfort and helps to cool the surface of the unlasered portions of the skin. We have not found a need for oral sedation for this technique or injection of any local anesthesia; however, there is no contraindication to either if needed for patient comfort. If sedation is utilized, patients should be carefully monitored. Immediately prior to commencing the procedure, standard laser safety precautions are undertaken. These include but are not limited to: blocking out light from any windows, immediate availability of water, ease of access to a fire extinguisher, and eye protection. There should be eye protection for patient and staff. Staff eye protection should be designed for the type of laser that is being used. Patient eyes should be covered with metal eye shields. These can be external or corneal types of shields. Plastic eye shields are not used because there is a risk of melting if struck by the laser. A multitude of lasers exist for fractional resurfacing today. As of this writing, there is no split-face study that clearly demonstrates the superiority of any one fractional resurfacing laser. The first author frequently uses a Cortex fractional CO2 laser (Ellman International, Hicksville, New York). Some patients have extensive superficial actinic changes of their facial skin. These patients may derive greater benefit from combined laser treatment with a fractional CO2 laser and superficial erbium laser treatment. Two separate laser devices can be used or both lasers may be available in the same laser device such as in the Cortex laser. There are multiple fractional CO2 lasers that are available. The settings used vary depending on numerous factors. First are physician laser experience and preference. Second are patient and physician goals for this treatment. Third are the time of recovery and the recovery experience that the patient is willing to undergo. Fourth are any potential risk factors for healing problems both systemic and local. Fifth are patient age and skin thickness. Although the authors rarely do this for fractional resurfacing, if there is any question about the effects of a planned laser treatment, test spots can be performed and complete treatment deferred until the results of the test spots are evaluated. Another consideration is that if, at any time during the course of a laser procedure, either patient experience or effects of the laser vary from what was anticipated prior to the treatment, the procedure should be interrupted and an evaluation should be performed as to whether to continue. The following settings are those used by the second author when treating patients with the Sandstone Matrix laser (Ellman). This laser has the capability of controlling many aspects of the laser process such as density, which is directly proportional to the percentage of skin surface area that is treated. The settings or techniques may be laser-specific and may not apply to any other device. Before using a laser, check with the manufacturer for recommended settings and techniques. Pulse duration represents the pulse width or tissue ablation time. Laser power represented in watts (W) correlates directly with the laser fluence. All resurfacing is done in continuous wave mode for fractional ablation. The pattern is generated in the handpiece and can be used in differing sizes and shapes depending on the operator’s preference and the area being treated. The laser is positioned at the patient’s side with the laser arm manipulated by the physician. The second author frequently uses a power of 21 to 23 W, density of ~ 30%, and duration of up to 2 ms. These settings are not universally used by all treating physicians on all patients. The second author treats each subunit with a uniformly, nonoverlapping, square-beam pattern beginning at the forehead. Care is taken to feather into the hairline for completeness. The first author does not treat by subunits. Rather he prefers to treat at least the lower two thirds of the face and, depending on the clinical findings, treat or omit treatment to the forehead region. An important consideration for any fractional laser is the dermal thermal effects. Excessive dermal heating can develop related to fluence, dermal density, and/or pulse duration. If the dermis is overheated there is a greater risk for scarring. Most physicians use a smoke evacuator to remove the laser plume. Surgical masks with a 0.1-µm pore size are also frequently used by the physician and any other staff in the procedure room. If resurfacing is performed in the periorbital area, milder settings should be used. The authors do not routinely resurface the skin of the upper eyelid below the upper eyelid fold. This is particularly important because fractional CO2 laser resurfacing can have a significant penetration depth. Fractional CO2 lasers can penetrate deeper than nonfractional resurfacing lasers. The number of passes that are performed and the settings for each pass vary for each patient and among treating physicians. If a second pass is performed, it should be done starting over at the area that was first treated so that the dermis in this area has had time to cool while subsequent areas were treated. Furthermore, the fractional pattern of the second pass should not overlap the first pass to avoid double pulsing any area and thermal stacking. The skin can have a patternlike appearance after fractional resurfacing. As long as excessive settings have not been used and there are no healing or infectious problems during the recovery period, this pattern is not visible after healing is completed. Pinpoint bleeding may also be noted in some areas immediately after the procedure or the evening after the treatment. This can occur when the fractional resurfacing extends into the level of the dermal plexus of vessels. The authors routinely discuss this possibility with their patients so it will not be a cause for concern. Resurfacing will on occasion be extended into the neck and décolleté area. This can be done quite effectively with fractional resurfacing, but adjustment of the laser settings must be done. Patients should understand that as reduced settings are used, there will be a more limited result. Moving to a lower power (16 W), decreasing density to around 21%, and lowering duration to 0.8 ms have been proven safe and effective in this area for the second author. However, it should be remembered that the neck and décolleté area have a lower sebaceous unit (adnexal structure) count in comparison to the face, different blood supply, and a significantly greater tendency for scarring. The lower settings are used to allow for these differences. Only one pass is made in these areas. These areas should be treated carefully because significant scarring has been reported in the cervical region after fractionated resurfacing.8 The authors cannot guarantee the safety of these settings for any particular patient. Physicians must make their own judgments. Two areas on the face that warrant further discussion and caution are the infraorbital and mandibular ridge regions. The skin of the infraorbital region is significantly thinner than the surrounding facial skin. This places it at higher risk for hypertrophic scarring and ectropion formation.9 Care should be taken in this area with lowered passes or energy settings, especially when laxity or previous surgery is noted. Similarly, the skin of the mandibular ridge is prone to hypertrophic scarring; thus fewer passes, reduced energy, and/or lower density may be warranted in this area. After the laser procedure is completed, as a comfort measure, the patient can be handed a chiller on a low setting to cool the treated surface. Aquaphor (Beiersdorf Inc., Wilton, Connecticut) or another petroleum-based ointment is then applied with a tongue depressor to all the treated areas. The first author has patients apply moist gauze compresses to the treated area with a mixture of white vinegar and water (1 tsp of white vinegar to 2 cups of water) at least three times a day and then reapply the Aquaphor. This vinegar and water mixture can be refrigerated to increase patient comfort. The ointment can predispose the patient to milia or acneiform eruptions. Removing the ointment three times a day and applying the moist compresses helps to reduce this. Furthermore, the ointment use is reduced or discontinued when possible on the 4th day after the procedure. If a patient still has significant dry crusts after 3 days, it is continued for an additional 1 or 2 days. In order to decrease the possibility of developing significant dyschromia after the procedure, it is important to avoid sun exposure. The authors start patients on daytime use of a sunscreen such as micronized zinc oxide that blocks ultraviolet A (UVA) and ultraviolet B (UVB), as soon as the Aquaphor use is diminished. In speaking with their patients, the authors emphasize the importance of the sunscreen. Many patients can start using a mineral-base foundation 5 to 7 days after the procedure. Typically, a mineral-base foundation also provides additional sun protection. Patients may experience some pruritus during the 1st or 2nd week after treatment. If a patient scratches a resurfaced area, this can lead to hypertrophic scarring. Scratching can occur even while a patient is sleeping. Therefore it is important to discuss this with the patient after the procedure. The first author’s standard postresurfacing instructions, in addition to advising the patient not to scratch, include taking an antihistamine such as diphenhydramine at bedtime, if there is even minimal pruritus. An antiscratching measure also discussed is the wearing of white cotton gloves while sleeping. The second author advises using a 1%-hydrocortisone cream once or twice daily for extreme itching. The first author does not routinely suggest this. The results obtained from fractional CO2 laser resurfacing can vary from patient to patient and with the problems being treated. Results can be quite dramatic when considering the reduced downtime associated with these lasers (▶ Fig. 5.3, ▶ Fig. 5.4, ▶ Fig. 5.5). After fractional resurfacing collagen stimulation occurs for at least 6 months. This is a gradual effect and is best seen comparing serial photographs. Because this is a gradual, progressive change, it may not be as obvious to patients who are checking their skin daily in the mirror. Therefore, the authors do not typically perform a second treatment until 6 months after the first treatment. This should be discussed in advance with patients so they are prepared for the gradual improvement. Fig. 5.3 Dramatic procedure results. (a) Before periorbital, segmental fractional CO2 laser resurfacing. (b) 1 year after the treatment.
5.3 Anatomy of Facial Resurfacing
5.4 Patient Selection
5.5 Preoperative Preparation
5.6 Procedure Technique
5.7 Postoperative Care
5.8 Expected Results

Fractional Laser Skin Resurfacing
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








