Femoroacetabular impingement (FAI) is the result of abnormal contact between the proximal femur and the acetabular rim.
 Abnormalities can be identified on either the femoral or acetabular side but are more commonly seen on both sides.
Abnormalities can be identified on either the femoral or acetabular side but are more commonly seen on both sides.
 This abnormal contact can lead to acetabular chondral lesions and or labral lesions, leading to hip pain and the development of diffuse osteoarthritis of the affected hip if left untreated.1,7,9
This abnormal contact can lead to acetabular chondral lesions and or labral lesions, leading to hip pain and the development of diffuse osteoarthritis of the affected hip if left untreated.1,7,9
ANATOMY
 The proximal femur and acetabulum normally articulate without abutment through a physiologic range of motion (ROM).
The proximal femur and acetabulum normally articulate without abutment through a physiologic range of motion (ROM).
 Required ROM, however, is variable depending on the activities performed, with less range required for sedentary individuals and extreme range required for activities such as dance, ballet, and hockey goalies.
Required ROM, however, is variable depending on the activities performed, with less range required for sedentary individuals and extreme range required for activities such as dance, ballet, and hockey goalies.
 The acetabulum normally is anteverted 12 to 16.5 degrees.
The acetabulum normally is anteverted 12 to 16.5 degrees.
 The acetabulum normally covers the femoral head to a depth that avoids impingement (ie, overcoverage) and instability (ie, dysplasia or undercoverage) with a horizontal, thin sourcil (ie, the weight-bearing zone).
The acetabulum normally covers the femoral head to a depth that avoids impingement (ie, overcoverage) and instability (ie, dysplasia or undercoverage) with a horizontal, thin sourcil (ie, the weight-bearing zone).
 The proximal femur normally has a spherical head–neck contour and appropriate offset that allows for impingement-free ROM.
The proximal femur normally has a spherical head–neck contour and appropriate offset that allows for impingement-free ROM.
 The normal femoral neck–shaft angle is 120 to 135 degrees; the femoral neck typically is anteverted 12 to 15 degrees.
The normal femoral neck–shaft angle is 120 to 135 degrees; the femoral neck typically is anteverted 12 to 15 degrees.
 The acetabular labrum functions to create a fluid pressurization seal with the femoral head.8
The acetabular labrum functions to create a fluid pressurization seal with the femoral head.8
 It is important to recognize and respect the location of the retinacular vessels that have been shown to enter the antero- and posterolateral portions of the femoral neck and supply the majority of the femoral head’s blood supply.
It is important to recognize and respect the location of the retinacular vessels that have been shown to enter the antero- and posterolateral portions of the femoral neck and supply the majority of the femoral head’s blood supply.
 The capsule is an important hip stabilizer and should be preserved and repaired to maintain soft tissue stability, particularly in dysplastic variants, generalized hypermobility, and connective tissue disorders.3
The capsule is an important hip stabilizer and should be preserved and repaired to maintain soft tissue stability, particularly in dysplastic variants, generalized hypermobility, and connective tissue disorders.3
PATHOGENESIS
 There are two primary mechanisms of FAI: pincer and cam-type impingement.1,7,9
There are two primary mechanisms of FAI: pincer and cam-type impingement.1,7,9
 Pincer impingement is the result of contact between an abnormal acetabular rim and femoral head–neck junction (FIG 1A).
Pincer impingement is the result of contact between an abnormal acetabular rim and femoral head–neck junction (FIG 1A).
Pincer impingement typically is the result of a globally deep acetabulum (coxa profunda), focal anterior overcoverage (acetabular retroversion), or, less commonly, posterior overcoverage.
It leads to labral bruising and degenerative tearing and eventually may result in ossification of the labrum and contrecoup posterior acetabular chondral injury.
Global overcoverage is more frequent in females, whereas acetabular retroversion is more common in males.
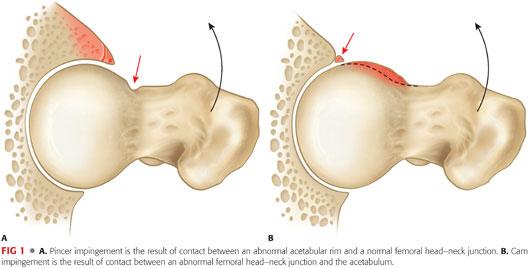
 Cam impingement is the result of contact between an abnormal femoral head–neck junction and the acetabulum (FIG 1B).
Cam impingement is the result of contact between an abnormal femoral head–neck junction and the acetabulum (FIG 1B).
The abnormal femoral head–neck junction is typically secondary to an aspherical anterolateral head–neck junction but also can be secondary to a slipped capital femoral epiphysis, femoral retroversion, coxa vara, malreduced femoral neck fracture, and, less commonly, posterior femoral head–neck abnormalities.
Cam impingement results in a shearing stress to the anterosuperior acetabulum, with predictable chondral delamination and labral detachment or tearing in some cases.
Although cam impingement is reported to predominate in young athletic males and pincer impingement in middle-aged women, most patients with FAI have a combination of both cam and pincer impingement.
 Extra-articular sources of impingement have been recently described.
Extra-articular sources of impingement have been recently described.
Anterior inferior iliac spine (AIIS) impingement is an increasingly recognized type of acetabular-based impingement.
The AIIS serves as the origin of the direct head of the rectus femoris, and impingement can be secondary to prior avulsion injury, pelvic osteotomy, or developmental as seen in the setting of acetabular retroversion.12,18,26
Ischiofemoral impingement is a rare type of proximal femoral-based impingement that occurs between the lesser trochanter and the ischial tuberosity.
The quadratus femoris occupies this space and may be compressed when this space is reduced.
The normal distance between the lesser trochanter and the ischial tuberosity is reported to be 20 mm. This space is reported to be reduced to around 13 mm in patients with ischiofemoral impingement.
In addition, women, as a result of the wider positioning of their ischial tuberosities, appear to be at greater risk.30
NATURAL HISTORY
 The likelihood of an individual with untreated FAI developing hip osteoarthritis is unknown because there have been no longitudinal studies prospectively following these patients before the development of symptoms.
The likelihood of an individual with untreated FAI developing hip osteoarthritis is unknown because there have been no longitudinal studies prospectively following these patients before the development of symptoms.
 Clinical experience with over 600 surgical dislocations of the hip in patients with FAI has revealed a strong association of this disorder with progressive acetabular chondral degeneration, labral tears, and progressive osteoarthritis.1,7,9
Clinical experience with over 600 surgical dislocations of the hip in patients with FAI has revealed a strong association of this disorder with progressive acetabular chondral degeneration, labral tears, and progressive osteoarthritis.1,7,9
 It is now well accepted that many patients with FAI will develop progressive chondral and labral injury, which can ultimately lead to end-stage hip osteoarthritis.
It is now well accepted that many patients with FAI will develop progressive chondral and labral injury, which can ultimately lead to end-stage hip osteoarthritis.
 One population study suggests that there is a 15% to 19% prevalence of deep acetabular socket and 5% to 19% prevalence of pistol grip deformity. This population had a relative risk ratio of developing hip osteoarthritis of 2.2 to 2.4.11
One population study suggests that there is a 15% to 19% prevalence of deep acetabular socket and 5% to 19% prevalence of pistol grip deformity. This population had a relative risk ratio of developing hip osteoarthritis of 2.2 to 2.4.11
 FAI and, in particular, cam-type morphology has been reported in up to 90% of athletic male patients.14,19
FAI and, in particular, cam-type morphology has been reported in up to 90% of athletic male patients.14,19
PATIENT HISTORY AND PHYSICAL FINDINGS
 Patients typically are young to middle aged (second through fourth decade) at presentation with complaints of groin pain exacerbated by physical activity.
Patients typically are young to middle aged (second through fourth decade) at presentation with complaints of groin pain exacerbated by physical activity.
 Prolonged sitting, arising from a chair, putting on shoes and socks, getting in and out of a car, and sitting with their legs crossed often exacerbate the symptoms.
Prolonged sitting, arising from a chair, putting on shoes and socks, getting in and out of a car, and sitting with their legs crossed often exacerbate the symptoms.
 We have found that patients may have a history of siblings, parents, and grandparents with hip pain or osteoarthritis of the hip, and patients may have milder or similar symptoms in the contralateral hip.
We have found that patients may have a history of siblings, parents, and grandparents with hip pain or osteoarthritis of the hip, and patients may have milder or similar symptoms in the contralateral hip.
 Patients often have had pain for months to years with the diagnosis of chronic low back pathology, hip flexor strains, and sports hernias/athletic pubalgia and not infrequently have had other surgeries without relief of their pain.28
Patients often have had pain for months to years with the diagnosis of chronic low back pathology, hip flexor strains, and sports hernias/athletic pubalgia and not infrequently have had other surgeries without relief of their pain.28
 Physical examinations should include the following:
Physical examinations should include the following:
Evaluation of hip ROM: Global ROM restriction indicates advanced osteoarthritis.
Anterior impingement test: Groin pain indicates anterolateral rim pathology.
Posterior impingement test: Groin pain or posterolateral pain indicates posterolateral rim pathology.
Extension/abduction and flexion/abduction indicates lateral-based pathology.
FABER test: FABER means flexion, abduction, and external rotation of the hip. Increased distance from the lateral knee to the examination table can indicate femoroacetabular impingement.
For subspine impingement, there is pain with straight flexion, restricted flexion, and, often, tenderness to palpation of the AIIS that recreates the flexion-based discomfort.
For ischiofemoral impingement, the symptoms can be reproduced by a combination of extension, adduction, and external rotation (ER).
IMAGING AND OTHER DIAGNOSTIC STUDIES
 Plain radiographs including an anteroposterior (AP) pelvis, a frog-leg lateral, 45-degree modified Dunn lateral or a cross-table lateral, and false-profile view are obtained.
Plain radiographs including an anteroposterior (AP) pelvis, a frog-leg lateral, 45-degree modified Dunn lateral or a cross-table lateral, and false-profile view are obtained.
 The AP radiograph should have a coccyx to symphyseal distance of 0 to 2 cm, with the coccyx centered over the symphysis to properly evaluate acetabular version.
The AP radiograph should have a coccyx to symphyseal distance of 0 to 2 cm, with the coccyx centered over the symphysis to properly evaluate acetabular version.
 The following are measured on the AP radiograph (FIG 2A):
The following are measured on the AP radiograph (FIG 2A):
A lateral center edge angle of 25 to 40 degrees distinguishes deep acetabulum from dysplasia.
The presence of a crossover sign represents retroversion and can indicate either local anterior overcoverage or superior posterior undercoverage.
The posterior wall sign indicates posterior undercoverage (retroversion).
Extension of the AIIS below the sourcil and cortical sclerotic change may be indicative of AIIS impingement.
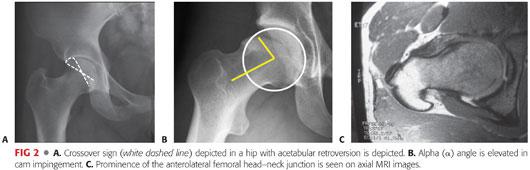
 Decreased femoral head–neck offset and asphericity can be indicative of cam-type morphology.
Decreased femoral head–neck offset and asphericity can be indicative of cam-type morphology.
A decreased femoral neck–shaft angle indicates coxa vara and may contribute to impingement.
 The frog-leg lateral, 45-degree modified Dunn lateral, and or cross-table lateral views with 15 degrees internal rotation (IR) should be evaluated for the following:
The frog-leg lateral, 45-degree modified Dunn lateral, and or cross-table lateral views with 15 degrees internal rotation (IR) should be evaluated for the following:
Alpha angle: normally less than 50 to 55 degrees (anterolateral prominence/aspherical femoral head–neck junction; FIG 2B).25
Femoral head–neck offset and offset ratio: Normal femoral head–neck offset is greater than 8 to 11 mm and the normal femoral head–neck offset ratio is greater than 0.15.
Femoral head–neck cystic changes and sclerosis
 The false profile is used to evaluate the following:
The false profile is used to evaluate the following:
Anterior center edge angle: anterior over- and undercoverage
Excessive anterior and distal extension of the AIIS: Normally, the distal extent of the AIIS is proximal to the acetabular rim.
Anterior and posterior joint space
 A magnetic resonance imaging (MRI) arthrogram is useful to evaluate for the following:
A magnetic resonance imaging (MRI) arthrogram is useful to evaluate for the following:
Labral and chondral pathology, acetabular version, and deformity of the femoral head–neck junction, which is best seen on the axial cuts and, in particular, with radial imaging (FIG 2C).
Femoral neck version: Retroversion/torsion may contribute to impingement, whereas excessive anteversion/torsion can contribute to instability; measurements require additional cuts through the distal femoral condyles.
Synovial herniation pits/impingement cysts at the femoral head–neck junction are also indicative of FAI.
An anesthetic agent can be included with the gadolinium to verify the hip joint as the source of pain, which is indicated by temporary pain relief with provocative maneuvers in the first couple of hours after the injection. Occasionally, the high volume of such an injection can lead to capsular distention with increased pain. Alternatively, a lower volume (<5 mL) of anesthetic-only injections can be used for diagnostic purposes.
The normal distance between the lesser trochanter and the ischial tuberosity is said to be 20 mm. This space is said to be reduced to around 13 mm in patients with ischiofemoral impingement.13
 Three-dimensional computed tomography (CT) scanning can be invaluable and obtained in all or select cases:
Three-dimensional computed tomography (CT) scanning can be invaluable and obtained in all or select cases:
The area of impingement can be more accurately mapped.
This may be done routinely in cases of subtle FAI or suspected unusual locations of FAI (eg, posterior femoral head/neck prominences) or for revision cases in order to better assess prior bone resection.
CT scan can also be used to evaluate femoral version/torsion (additional cuts through the distal femoral condyles required) and acetabular version.5
DIFFERENTIAL DIAGNOSIS
 Sports hernia/athletic pubalgia/core muscle injury
Sports hernia/athletic pubalgia/core muscle injury
 Lumbar spine pathology
Lumbar spine pathology
 Gynecologic or urologic pathology
Gynecologic or urologic pathology
 Intra-abdominal pathology
Intra-abdominal pathology
 Hip flexor pathology or iliopsoas snapping
Hip flexor pathology or iliopsoas snapping
 Iliotibial band pathology or snapping
Iliotibial band pathology or snapping
 Other extra-articular myotendinous pathology
Other extra-articular myotendinous pathology
 Abductor/gluteus medius/minimus pathology
Abductor/gluteus medius/minimus pathology
 Pelvic stress fracture
Pelvic stress fracture
 Apophysitis or apophyseal injury in the developing skeleton
Apophysitis or apophyseal injury in the developing skeleton
 Intra-articular pathology not related to FAI
Intra-articular pathology not related to FAI
 Extra-articular hip impingement
Extra-articular hip impingement
 Neurogenic disorders
Neurogenic disorders
NONOPERATIVE MANAGEMENT
 Nonoperative management of FAI consists of activity modification; avoiding painful activities such as deep hip flexion, aggressive hip flexion–based weight training, and other athletic activities that aggravate symptoms; and anti-inflammatories/analgesics and intra-articular injection in select cases.
Nonoperative management of FAI consists of activity modification; avoiding painful activities such as deep hip flexion, aggressive hip flexion–based weight training, and other athletic activities that aggravate symptoms; and anti-inflammatories/analgesics and intra-articular injection in select cases.
 Intra-articular pathology often progresses without symptoms early in the disease, and there is concern that without surgical treatment, significant labrochondral injury and arthritis might eventually develop, particularly in large cam-type deformities.
Intra-articular pathology often progresses without symptoms early in the disease, and there is concern that without surgical treatment, significant labrochondral injury and arthritis might eventually develop, particularly in large cam-type deformities.
 Nonoperative management may be best employed in the already degenerative hip with joint space narrowing prior to total hip arthroplasty or milder deformities in patients willing to modify activities and consists of activity modification, core trunk strengthening exercises, and occasional intra-articular corticosteroid or hyaluronic acid injections.
Nonoperative management may be best employed in the already degenerative hip with joint space narrowing prior to total hip arthroplasty or milder deformities in patients willing to modify activities and consists of activity modification, core trunk strengthening exercises, and occasional intra-articular corticosteroid or hyaluronic acid injections.
SURGICAL MANAGEMENT
 Physical examination and imaging studies consistent with FAI
Physical examination and imaging studies consistent with FAI
 Pain despite activity modification
Pain despite activity modification
 Pain in patients who are unable or unwilling to modify activity
Pain in patients who are unable or unwilling to modify activity
 Minimal to no degenerative changes
Minimal to no degenerative changes
 Arthroscopic versus open procedure for FAI (Table 1)
Arthroscopic versus open procedure for FAI (Table 1)

 There are no strict indications for open versus arthroscopic management of traditional FAI, and decisions are typically made on the ability of the surgeon to correct the deformities with a given approach.
There are no strict indications for open versus arthroscopic management of traditional FAI, and decisions are typically made on the ability of the surgeon to correct the deformities with a given approach.
 Posteriorly based femoral deformities, extra-articular trochanteric–pelvic impingement, and cases of mixed FAI/dysplastic anatomy with a predominance of instability findings are better served with open corrective procedures.
Posteriorly based femoral deformities, extra-articular trochanteric–pelvic impingement, and cases of mixed FAI/dysplastic anatomy with a predominance of instability findings are better served with open corrective procedures.
 Some higher level athletes may benefit from an arthroscopic approach with the possibility of an earlier return to sports compared to open corrective procedures.29
Some higher level athletes may benefit from an arthroscopic approach with the possibility of an earlier return to sports compared to open corrective procedures.29
Preoperative Planning
 Initially, a fluoroscopic evaluation is done and the pelvis is leveled in order to recreate an image of the acetabulum that recreates a well-centered preoperative AP pelvis radiograph with respect to the relationship between the anterior and posterior acetabular walls. Next, a systematic evaluation of the femoral head–neck junction is performed with six specific views. Three views are taken in extension (ER, neutral, IR) in order to evaluate the lateral and medial head–neck junction and three views in 30 to 40 degrees of hip flexion (neutral, 30 degrees ER, 50 degrees ER) in order to evaluate the anterior and posterior femoral head–neck junction.
Initially, a fluoroscopic evaluation is done and the pelvis is leveled in order to recreate an image of the acetabulum that recreates a well-centered preoperative AP pelvis radiograph with respect to the relationship between the anterior and posterior acetabular walls. Next, a systematic evaluation of the femoral head–neck junction is performed with six specific views. Three views are taken in extension (ER, neutral, IR) in order to evaluate the lateral and medial head–neck junction and three views in 30 to 40 degrees of hip flexion (neutral, 30 degrees ER, 50 degrees ER) in order to evaluate the anterior and posterior femoral head–neck junction.
 Dynamic fluoroscopic evaluation by abduction of the hip in flexion, ER, and extension with IR and ER and abduction occasionally reveals impingement of the acetabulum on the proximal femur and results in a vacuum effect in the joint as the proximal femur is levered out of the acetabulum.
Dynamic fluoroscopic evaluation by abduction of the hip in flexion, ER, and extension with IR and ER and abduction occasionally reveals impingement of the acetabulum on the proximal femur and results in a vacuum effect in the joint as the proximal femur is levered out of the acetabulum.
Positioning
 Arthroscopic management of FAI begins with standard hip positioning in either the supine or lateral position.
Arthroscopic management of FAI begins with standard hip positioning in either the supine or lateral position.
 We prefer the supine position with the hip in slight flexion, neutral abduction, and IR (FIG 3).
We prefer the supine position with the hip in slight flexion, neutral abduction, and IR (FIG 3).

Approach
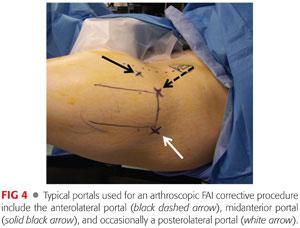
 Most cases can be performed using the standard anterior paratrochanteric and anterior or midanterior portals, with occasional use of the posterior paratrochanteric or accessory distal portal (FIG 4).
Most cases can be performed using the standard anterior paratrochanteric and anterior or midanterior portals, with occasional use of the posterior paratrochanteric or accessory distal portal (FIG 4).
TECHNIQUES
 Diagnostic Arthroscopy
Diagnostic Arthroscopy
Initially, the intra-articular portions of the hip are evaluated, including the acetabular labrum, acetabulum, and femoral head articular cartilage; fovea; ligamentum teres; transverse acetabular ligament; and capsular structures (TECH FIG 1A,B).
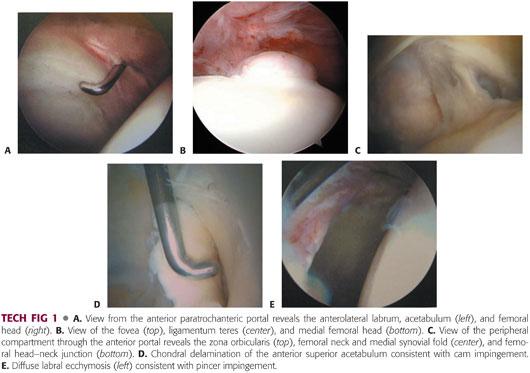
The peripheral compartment is evaluated, including the femoral head–neck junction and femoral neck to the capsular reflection/peripheral capsular attachments, labrum, zona orbicularis, and medial and lateral synovial folds (TECH FIG 1C).
The pathology present helps to define the pathomechanics at work, with chondral delamination in the anterior superior acetabulum often indicating cam-type impingement (TECH FIG 1D) and labral ecchymosis, tearing, and linear posterior acetabular chondral wear indicating pincer-type impingement. Focal labral and capsular bruising/synovitis in the region of the AIIS can be consistent with subspine/AIIS impingement. It is important to recognize that there are often a combination of pathomechanics at work and therefore a number of pathologic findings frequently coexist. In addition, these same findings can be seen in the setting of dysplasia as well (TECH FIG 1E).
 Pincer Impingement
Pincer Impingement
When pincer impingement is present, the labrum is assessed for ecchymosis (TECH FIG 2A), intralabral cyst, degenerative tearing, and ossification; regions of underlying rim prominence/rim fractures are identified.
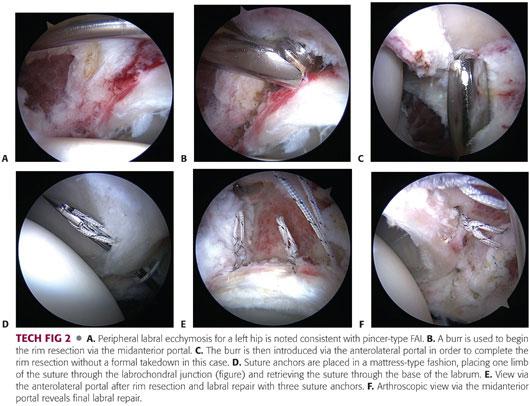
Attempts should be made to preserve the labrum when possible in order to preserve the potential sealing mechanism.
If irreparable tearing of the labrum is present, the labrum is carefully/selectively débrided; however, the periphery of the labrum often remains intact and may be amenable to repair or refixation.
If the labrum is amenable to repair or refixation, the current authors most frequently resect areas of acetabular overcoverage without labral detachment (TECH FIG 2B,C) and reserve labral detachment for cases of more severe focal or global overcoverage.
The capsule is reflected away from the acetabular rim, and the labrum is left attached to the articular margin of the acetabular rim.
Alternatively, the labrum can be carefully detached from the acetabulum using a Beaver blade and shaver, beginning at the periphery and extending to the articular side of the labrum.
Care must be taken to detach as much of the labrum as possible without cutting too deep on the articular side, which could result in inadvertent delamination of the acetabular articular cartilage.
The rim resection usually extends from the anterior portal to the 12 o’clock position for focal anterior overcoverage. Rim resection is quite variable and should be based on preoperative imaging studies and intraoperative findings consistent with pincer-type impingement.
The current authors have become less aggressive with regard to rim resection, particularly in the setting of acetabular retroversion. The current authors try not to resect the rim beyond an lateral center edge angle of 30 to 35 degrees and typically leave 35% to 40% anterior and 40% to 50% posterior femoral head coverage. Again, the amount of resection is quite variable and should be based on preoperative imaging, intraoperative pathologic findings, and dynamic assessment.
If areas of grade 4 chondromalacia remain after acetabular rim trimming, microfracture is performed on the exposed bone.
Suture anchors (usually two to four anchors) are then placed 1 to 2 mm off the articular margin of the acetabulum with care to avoid intra-articular and anterior acetabular wall penetration. Up to five to eight anchors or more can be used for global labral refixation or reconstruction when indicated. The sutures are first passed under the labrum and then retrieved around or through the labrum, securing the labrum to the rim with standard knot-tying techniques (TECH FIG 2D–F).
We generally prefer a mattress base stitch, which might better recreate the labral sealing function. In cases of minimal or poor tissue/hypoplastic labrum, a simple loop stitch can be used in order to avoid further labral compromise.
Care is taken to place the knot on the capsular or medial side of the labrum to avoid damaging the femoral articular cartilage with prominent suture during weight bearing and ROM.
 OS Acetabuli/Subspine and Ischiofemoral Impingement
OS Acetabuli/Subspine and Ischiofemoral Impingement
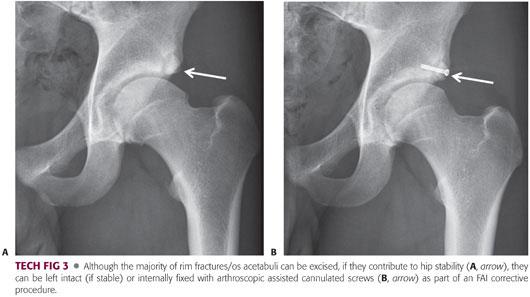
Occasionally, an os acetabuli or rim fracture is responsible for local anterior/posterolateral overcoverage and typically is attached to the acetabulum just peripheral to or behind the labrum.
The os is exposed and excised using a burr beyond the fibrocartilage attachment of the native acetabulum with or without labral débridement or refixation (TECH FIG 3). Most often, the labrum is preserved. If the hip is dysplastic without the fragment, the fragment can be left alone (if stable) or stabilized with arthroscopic assisted cannulated screws after partial excision if necessary.20 If AIIS impingement is present, the resection is carried further proximal at the anterior rim to identify and decompress the prominent AIIS.
It is occasionally helpful to make an additional window through the medial capsule in order to perform a more proximal resection. This allows for greater resection for larger AIIS deformities with the ability to close the capsule at the conclusion of the case when deemed necessary.
In severe cases of ischiofemoral impingement, the lessor trochanter can be burred down either open or arthroscopically to widen the ischiofemoral distance or, alternatively, the hamstrings can be detached from the ischial tuberosity followed by a lateral ischial decompression. The site of decompression depends on the degree and locations of ischiofemoral impingement.
 Cam Impingement
Cam Impingement
Exposure of the femoral head–neck junction can be performed using a generous capsulotomy, capsulectomy, or small capsular window.
We prefer a generous capsulotomy beginning anterior to the anterior portal and extending to the posterolateral portal site (TECH FIG 4A).
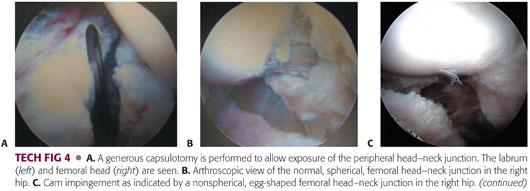
We find that with this technique and careful capsular exposure, the femur can be decompressed from the medial to lateral synovial folds, beyond the synovial folds staying proximal to the vessels, and distally to the level of the trochanter/capsular reflexion. In addition, a portion or all of the capsulotomy can be repaired or plicated at the conclusion of the procedure if deemed necessary.
One alternative approach is to use a “T” capsulotomy to expose the cam, although we find this to be rarely necessary. This should be repaired at the end of the resection as it further compromises the capsule.
At the conclusion of central compartment work, traction is released, and the hip is flexed/extended/abducted/adducted with varying degrees of IR and ER, allowing for visualization of the peripheral head–neck junction and the cam deformity.
The normal head–neck junction is relatively spherical (TECH FIG 4B), whereas in cam impingement, it appears egg-shaped, flat, or with a prominence at the head–neck junction (TECH FIG 4C).
The cam deformity is covered with relatively normal-appearing articular cartilage with varying degrees of eburnation, which can progress to a more degenerative peripheral head–neck junction with clefts and intraosseous cysts in more advanced cases.
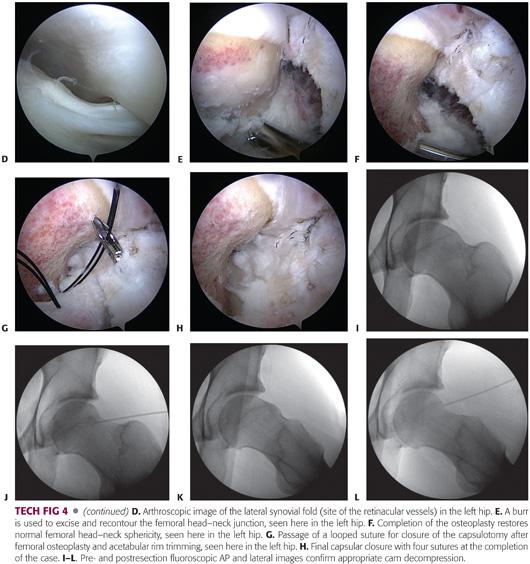
The medial and lateral (TECH FIG 4D) synovial folds should be identified.
Dynamic assessment confirms cam impingement and regions of impingement.
A 5.5-mm burr is used to reshape the anterolateral prominence with the goal of improving sphericity and offset with impingement-free motion (TECH FIG 4E).
Recontouring the femur and attempting to create a convexity into a concavity is ideal in an effort to preserve the labral sealing function through greater ROM than a concave resection (TECH FIG 4F).
A recent cadaveric study recommended resecting no more than 30% of the thickness of the femoral neck in order to minimize the risk for pathologic fractures postoperatively.21
The anterior head–neck junction is best recontoured in various degrees of flexion, and the lateral and medial head–neck junction are best recontoured in hip extension/IR with variable degrees of traction.
Three views in extension and three views in flexion are used to confirm the resection medially/laterally (AP view) and anteriorly (lateral view) (TECH FIG 4I–L).
Care is taken to keep resections proximal to the medial and lateral synovial folds for posterolateral and anteromedial resections in order to avoid damage to the retinacular vessels.
The typical pattern of cam impingement extends down the neck on the anterolateral femoral head–neck junction and closer to the articular cartilage margin of the femoral head, more superiorly in the region of the lateral and medial retinacular vessels.
Final confirmation of adequate resection is then verified arthroscopically with dynamic assessment in flexion/IR (anterior femur), extension/abduction, and flexion abduction (lateral femur).
Capsular closure is then performed with two to six absorbable sutures passed through one side of the capsule with a looped suture passer and grasped through the other side of the capsule (TECH FIG 4F–H).
A combination of absorbable and nonabsorbable sutures are considered for excessive capsular laxity, capsular incompetence in the revision setting, and connective tissue disorders such as Ehlers-Danlos syndrome.
A knot is then tied blindly at the periphery of the capsule using standard arthroscopic knot-tying techniques.
The hip is then infiltrated with an anesthetic, and the portals are closed in the usual fashion.
PEARLS AND PITFALLS | |
Indications |
|
| |
Exposure |
|
| |
| |
Pincer |
|
| |
| |
Cam |
|
| |
| |
Complications |
|
| |
POSTOPERATIVE CARE
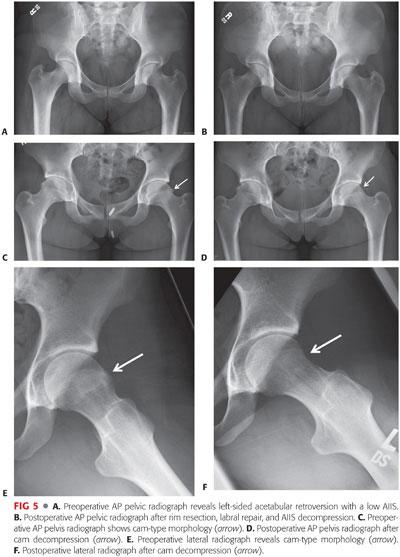
 Pre- and postoperative radiographs confirm adequate osteoplasty and rim trimming (FIG 5).
Pre- and postoperative radiographs confirm adequate osteoplasty and rim trimming (FIG 5).
 Postoperative restrictions are not consistent from one surgeon to the next and are based on the procedures done.
Postoperative restrictions are not consistent from one surgeon to the next and are based on the procedures done.
 We recommend the following restrictions:
We recommend the following restrictions:
Proximal femoral osteoplasty is treated with protected weight bearing with crutches for 2 to 4 weeks depending on the quality of bone and no high-impact or running activities for 2.5 to 3 months.
Acetabular rim trimming with labral débridement requires no specific restrictions.
Acetabular labral repair and refixation is treated with toe-touch weight bearing for 2 weeks and avoidance of the extremes of external rotation for 2 weeks.
Significant capsular repairs should be protected against passive hip extension and extremes of ER for 2 to 4 weeks.
Microfracture procedures are treated with 4 to 8 weeks of toe-touch weight bearing depending on the size of the lesion.
There is no evidence to support or refute the benefit of hip braces, derotational boots, or continuous passive machines (CPMs).
 Passive ROM with circumduction, stationary bicycle, or CPM should be instituted the day of surgery or postoperative day 1.
Passive ROM with circumduction, stationary bicycle, or CPM should be instituted the day of surgery or postoperative day 1.
 The first 2 months focus on restoration of ROM, gait and pelvic alignment, and gentle core strengthening.
The first 2 months focus on restoration of ROM, gait and pelvic alignment, and gentle core strengthening.
 At 2 months, more aggressive core strengthening is instituted, with resumption of full sporting activities at 3 to 6 months based on functional improvement.
At 2 months, more aggressive core strengthening is instituted, with resumption of full sporting activities at 3 to 6 months based on functional improvement.
 Further research is required to develop the optimal rehabilitation programs after the various procedures that have been discussed.
Further research is required to develop the optimal rehabilitation programs after the various procedures that have been discussed.
OUTCOMES
 Early and midterm results and systematic reviews for FAI indicate that pain and function are improved for the majority of patients and directly correlates with the degree of osteoarthritic changes found at the time of surgery.1,2,4,6,7,22–24,27
Early and midterm results and systematic reviews for FAI indicate that pain and function are improved for the majority of patients and directly correlates with the degree of osteoarthritic changes found at the time of surgery.1,2,4,6,7,22–24,27
Studies looking at open and arthroscopic approaches found improvement in pain in 68% to 96% of patients regardless of approach.2,4,6,22,24
In a review of 45 professional and Olympic level athletes with FAI treated arthroscopically, all had symptomatic improvement and returned to play.29
In another series of 320 patients with FAI treated arthroscopically, 90% had elimination of the impingement sign and were reportedly satisfied with their results.10
 Some evidence indicates that repair or refixation of the labrum results in improved outcomes when compared to labral débridement or excision in a consecutive series.7,17
Some evidence indicates that repair or refixation of the labrum results in improved outcomes when compared to labral débridement or excision in a consecutive series.7,17
Larson and Giveans16 prospectively followed 100 patients with FAI treated arthroscopically for a mean of 3.5 years, with statistically significant better outcomes (Harris hip score, SF-12, and visual analogue pain scoring) with labral preservation versus excision with 92% good to excellent results versus 68%, respectively.
Krych et al,15 in a randomized study, found better outcomes with labral repair for Activities of Daily Living and Sports subscale of the Hip Outcome Score than labral débridement in females at 32-month follow-up.
 No well-designed, long-term, or randomized studies have been done to evaluate outcomes after management of FAI to determine whether the natural history with regard to the development of osteoarthritis is altered. Longer term follow-up and studies after open versus arthroscopic treatment should better define the optimal indications and procedures for patients with FAI.
No well-designed, long-term, or randomized studies have been done to evaluate outcomes after management of FAI to determine whether the natural history with regard to the development of osteoarthritis is altered. Longer term follow-up and studies after open versus arthroscopic treatment should better define the optimal indications and procedures for patients with FAI.
COMPLICATIONS
 Lateral femoral cutaneous nerve neurapraxia (common and typically resolves)
Lateral femoral cutaneous nerve neurapraxia (common and typically resolves)
 Heterotopic bone or myositis ossificans formation
Heterotopic bone or myositis ossificans formation
Three weeks of nonsteroidal anti-inflammatory drugs recommended
 Iatrogenic acetabular and femoral chondral damage
Iatrogenic acetabular and femoral chondral damage
Careful surgical technique required to minimize
 Rarely postoperative femoral neck fracture
Rarely postoperative femoral neck fracture
Osteopenic bone/overresections/early aggressive weight bearing
 Potential for sciatic or pudendal nerve neurapraxia
Potential for sciatic or pudendal nerve neurapraxia
Minimize traction amount and time
 Potential for avascular necrosis
Potential for avascular necrosis
Not reported after femoral resections
 Uncommon: deep venous thrombosis/pulmonary embolism
Uncommon: deep venous thrombosis/pulmonary embolism
Typically have risk factors
 Uncommon: fluid extravasation
Uncommon: fluid extravasation
Recommend avoiding prolonged high-pressure fluid systems
REFERENCES
1. Beck M, Leunig M, Parvizi J, et al. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res 2004;418:67–73.
2. Bedi A, Chen N, Robertson W, et al. The management of labral tears and femoroacetabular impingement of the hip in the young, active patient. Arthroscopy 2008;24(10):1135–1145.
3. Bedi A, Galano G, Walsh, C, et al. Capsular management during hip arthroscopy: from femoroacetabular impingement to instability. Arthroscopy 2011;27(12):1720–1731.
4. Botser IB, Smith TW Jr, Nasser R, et al. Open surgical dislocation versus arthroscopy for femoroacetabular impingement: a comparison of clinical outcomes. Arthroscopy 2011;27(2):270–278.
5. Buller LT, Rosneck J, Monaco FM, et al. Relationship between proximal femoral and acetabular alignment in normal hip joints using 3-dimensional computed tomography. Am J Sports Med 2012;40(2):367–375.
6. Clohisy JC, St John LC, Schutz AL. Surgical treatment of femoroacetabular impingement: a systematic review of the literature. Clin Orthop Relat Res 2010;468(2): 555–564.
7. Espinosa N, Rothenfluh DA, Beck M, et al. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am 2006;88(5): 925–935.
8. Ferguson SJ, Bryant JT, Ganz R, et al. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech 2003;36(2):171–178.
9. Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003;(417):112–120.
10. Glick JM, Sampson TG, Gordon RB, et al. Hip arthroscopy by the lateral approach. Arthroscopy 1987;3(1):4–12.
11. Gosvig KK, Jacobsen S, Sonne-Holm S, et al. Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis: a population-based survey. J Bone Joint Surg Am 2010;92(5):1162–1169.
12. Hapa O, Bedi A, Gursan O, et al. Anatomic footprint of the direct head of the rectus femoris origin: cadaveric study and clinical series of hips after arthroscopic anterior inferior iliac spine/subspine decompression. Arthroscopy 2013;29(12):1932–1940.
13. Johnson KA. Impingement of the lesser trochanter on the ischial ramus after total hip arthroplasty. Report of three cases. J Bone Joint Surg Am 1977;59(2):268–269.
14. Kapron AL, Anderson AE, Aoki SK, et al. Radiographic prevalence of femoroacetabular impingement in collegiate football players: AAOS Exhibit Selection. J Bone Joint Surg Am 2011;93(19):e111(1–10).
15. Krych AJ, Thompson M, Knutson Z, et al. Arthroscopic labral repair versus selective labral debridement in female patients with femoroacetabular impingement: a prospective randomized study. Arthroscopy 2013;29(1):46–53.
16. Larson CM, Giveans MR. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy 2009;25(4):369–376.
17. Larson CM, Giveans MR, Stone RM. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: mean 3.5-year follow-up. Am J Sports Med 2012;40(5):1015–1021.
18. Larson CM, Kelly BT, Stone RM. Making a case for anterior inferior iliac spine/subspine hip impingement: three representative case reports and proposed concept. Arthroscopy 2011;27(12):1732–1737.
19. Larson CM, Sikka RS, Sardelli MC, et al. Increasing alpha angle is predictive of athletic related “hip” and “groin” pain in collegiate NFL prospect. Arthroscopy 2013;29(3):405–410.
20. Larson CM, Stone RM. The rarely encountered rim fracture that contributes to both femoroacetabular impingement and hip stability: a report of two cases of arthroscopic partial excision and internal fixation. Arthroscopy 2011;27(7):1018–1022.
21. Mardones RM, Gonzalez C, Chen Q, et al. Surgical treatment of femoroacetabular impingement: evaluation of the effect of the size of the resection. Surgical technique. J Bone Joint Surg Am 2006;88(suppl 1)(pt 1):84–91.
22. Matsuda DK, Carlisle JC, Arthurs SC, et al. Comparative systematic review of the open dislocation, mini-open, and arthroscopic surgeries for femoroacetabular impingement. Arthroscopy 2011;27(2):252–269.
23. Murphy S, Tannast M, Kim YJ, et al. Debridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res 2004;(429):178–181.
24. Ng VY, Arora N, Best TM, et al. Efficacy of surgery for femoroacetabular impingement: a systematic review. Am J Sports Med 2010;38(11):2337–2345.
25. Notzli HP, Wyss TF, Stoecklin CH, et al. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br 2002;84(4):556–560.
26. Pan H, Kawanabe K, Akiyama H, et al. Operative treatment of hip impingement caused by hypertrophy of the anterior inferior iliac spine. J Bone Joint Surg Br 2008;90(5):677–679.
27. Peters CL, Erickson JA. Treatment of femoro-acetabular impingement with surgical dislocation and debridement in young adults. J Bone Joint Surg Am 2006;88(8):1735–1741.
28. Philippon MJ, Maxwell RB, Johnston TL, et al. Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc 2007;15(8):1041–1047.
29. Philippon MJ, Schenker ML. Arthroscopy for the treatment of femoroacetabular impingement in the athlete. Clin Sports Med 2006;25(2):299–308, ix.
30. Torriani M, Souto SC, Thomas BJ, et al. Ischiofemoral impingement syndrome: an entity with hip pain and abnormalities of the quadratus femoris muscle. AJR Am J Roentgenol 2009;193(1):186–190.
< div class='tao-gold-member'>
















