Key Words
post-burn toe contracture, post-burn foot contracture, post-burn ankle contracture, rocker-bottom deformity, post-burn foot reconstruction, post-burn ankle reconstruction
Synopsis
Foot burns consist of a small percentage of the total body surface area calculated for burns, but injury to this region of anatomical importance can often result in debilitating consequences. The complexity of these burns requires specialized treatment by a multidisciplinary group, consisting of foot and ankle professionals, burn reconstructive surgeons, and rehabilitative experts. The goal of reconstruction should be to achieve smooth and painless ambulation by preserving limb length, function, and mobility. The most commonly encountered issue with foot and ankle burns involves contracture deformity, which often requires surgical release of scars, scarred tendons, and tight joint capsules, correction of bony deformities, and coverage of soft tissue defects. In the immediate post-operative setting, splinting plays an essential role in proper healing and in minimizing recontracture. When the wounds are ready, physical rehabilitation should begin promptly, because therapy is of the utmost importance in regaining optimal functional recovery of the foot and ankle.
Clinical Problem
Presentation and Etiology
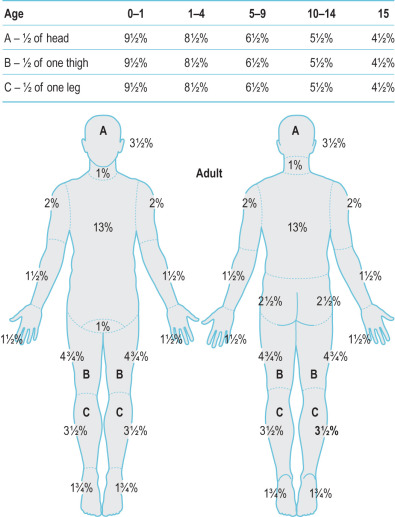
According to the Lund and Browder method of calculating the percentage of total body surface area (TBSA) burned, complete bilateral foot burns contribute a maximum of 7% TBSA ( Fig. 4.10.1 ). Though a small percentage, given the complex nature of foot burns and their potentially devastating functional consequences, all partial- and full-thickness burns involving the feet meet criteria for transfer to a specialized burn center. Foot burns can be sustained from multiple etiologies, such as scald burns, flame burns, contact burns, chemical injuries, electrical injuries, and frostbite injuries. Mechanisms of injury include accidental trauma, assault, rituals, and abuse and/or neglect (especially in the pediatric and elderly populations). One of the more common scenarios involves contact burns in patients with diabetes. Due to peripheral neuropathy, the patient’s feet are often insensate, leading to increased risk for injury. One study demonstrated a 68% incidence rate of pedal burns in patients with diabetes, versus 14% in patients without diabetes, deeming those with diabetes as an at-risk population for suffering from foot burns. In the developing world, open cooking fires are a common cause of foot burns, particularly in children.
Associated Conditions
The principal reconstructive goal of foot burn reconstruction should be to achieve smooth and painless ambulation by restoring anatomical limb length, function, and range of motion. Various conditions may be associated with pedal burns. One must consider growth disturbances in children, because they are at high risk for secondary bone-joint changes (i.e., ankle equinus, varus, and valgus deformities), abnormal gait patterns, chronic ulceration, infection, untreated bony and/or nerve abnormalities, and toe syndactyly. As evidenced by the potential intricacies that need to be addressed in foot burns, a multidisciplinary team of foot and ankle professionals, burn reconstructive surgeons, and rehabilitative experts is essential to providing optimal care and management to those suffering from foot burns.
Pre-Operative Management
Physical Examination, Key Anatomy, and Pre-Operative Studies Needed
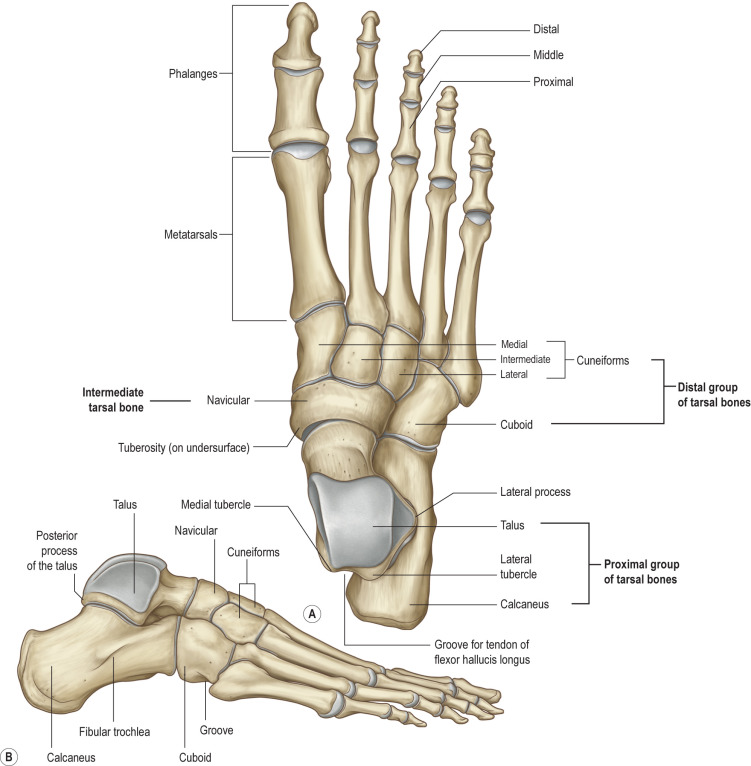
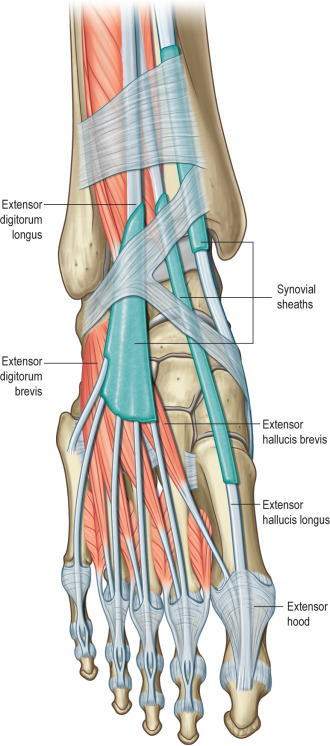
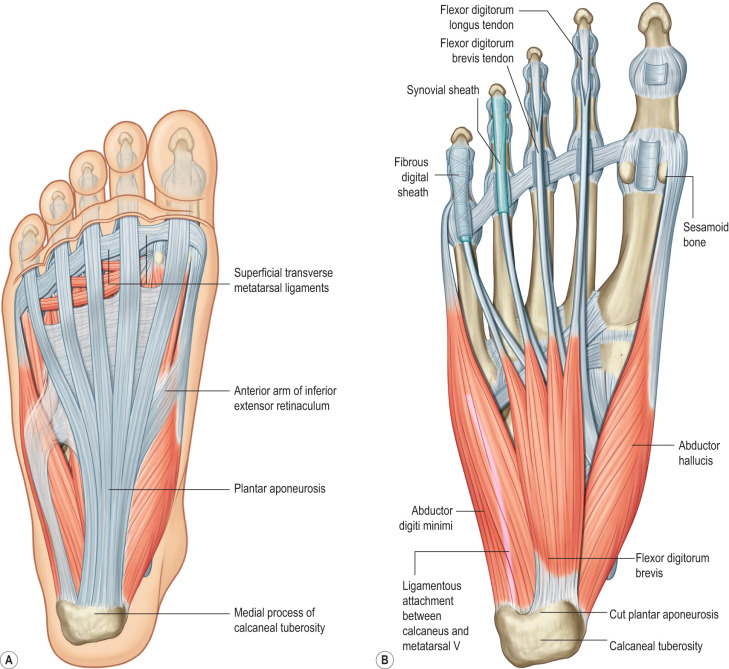
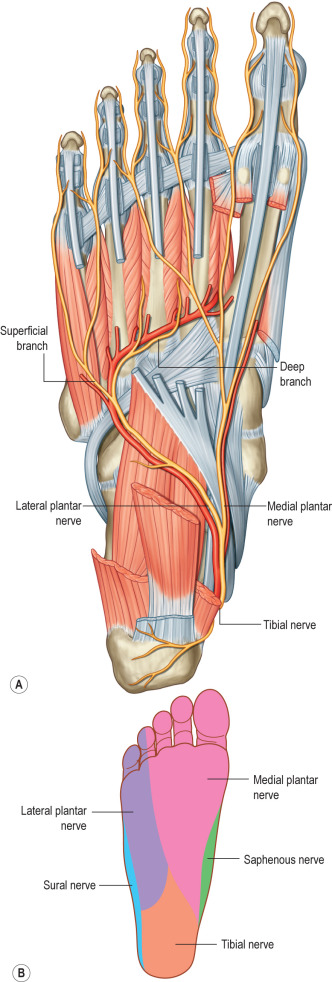
A comprehensive pre-operative assessment of the patient is key to successful reconstructive planning. A thorough patient history and physical examination should be performed. When the history is obtained, the patient’s mechanism of injury and any existing comorbid conditions, such as neuropathy, peripheral vascular disease, collagen vascular disease, and/or venous stasis, should be documented. As well, knowledge of vital foot and ankle anatomy is essential to understanding the patient’s pathological process. An overview of pertinent regional anatomy is depicted in Figs. 4.10.2 through 4.10.5 . Upon performing the physical examination, one should assess acute foot burns for depth, area, and location of burn. For purposes of reconstructive planning, the foot and ankle should be considered in three anatomical subunits: (1) dorsal (foot and toes), (2) plantar (foot-arch, toes, and heel), and (3) ankle (anterior, posterior, medial, and lateral). The importance of these anatomical subunits will be further addressed in the Surgery section of this chapter. In assessing burn contracture deformities of the foot and ankle, one should examine the extent of the scarring and soft tissue contracture, active and passive range of motion, limb length, ambulation, and the presence of any chronic wounds. Radiographic studies may also be obtained to evaluate for any underlying bony abnormalities or evidence of heterotopic ossification.
Optimal Timing of Surgery
Given the potentially debilitating consequences of delayed treatment, foot burns should be managed in a timely, expeditious manner. As with most acute burns, early excision and grafting of foot burns have shown beneficial effects, such as decreased pain, shorter hospitalizations, faster healing times, and improved functional recovery. For the purposes of our chapter, we will focus on the reconstruction of burn contracture deformities; acute burn management will be addressed in Chapter 4.1 . In many instances, scar revisions are delayed until scar maturation. However, in foot and ankle burn reconstruction, these operations are frequently performed at an earlier time, to address the following debilitating complications: contractures limiting function, growth disturbances, and unstable soft tissue.
Supplies Needed
Proper operating room equipment is essential to ensuring a smooth intra-operative course. In acute burn management, tools for tangential excision (Weck knife, Watson knife, VersaJet ® , etc.) and skin grafting (Dermatome, mesher, etc.) should be available. Given the intricate contours of foot and ankle anatomy, debridement via VersaJet ® , a hydrosurgical device, may allow for improved ease and accuracy of debridement over irregular surfaces, while preserving healthy tissue and vital structures. However, this may not be available throughout the world. In the post-acute burn phase, operative management most commonly focuses on releasing contracture deformities. As such, the surgeon should ensure availability of Kirschner wires for temporary joint fixation, in addition to equipment suitable for skin graft and/or flap coverage of acquired soft tissue defects resulting from contracture release. For all operative cases, usage of a tourniquet should be considered to minimize amount of blood loss and to optimize intraoperative visualization.
Anesthesia Concerns
Operations of the foot and ankle can be performed with either general or regional anesthesia. The risks and benefits of both should be discussed in detail with the anesthesiologist, taking into consideration the patient’s medical comorbidities, case complexity, and patient’s preference. Additionally, post-operative pain control should be taken into account at this time, because regional nerve block catheters could be of significant benefit in optimizing post-operative physical rehabilitation.
Surgery
For acute burn management of the foot and ankle, operations include escharotomies, tangential excisions, and skin grafts, which are discussed in Chapter 4.1 . Here we will focus on the details of releasing scar and joint contractures as well as on the options for reconstruction of resultant soft tissue deficits.
General Principles
Local Tissue Rearrangement
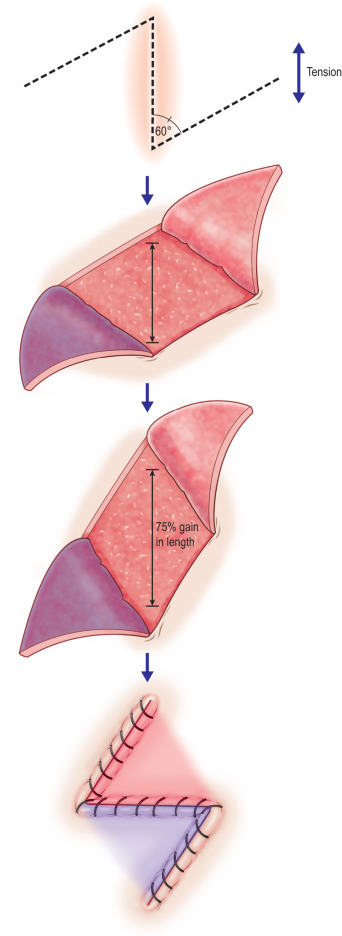
Release of scar contracture with local tissue rearrangement is a pillar of operative management. This technique utilizes local tissue to lengthen and disrupt symptomatic scars. One highly utilized technique is the versatile Z-plasty technique, which uses equilateral triangles of 60-degree angles to lengthen and disrupt the scar ( Fig. 4.10.6 ). Variations of this technique may be used by customizing the angles and the number of interposed flaps to the contour of the scar. Furthermore, the depth at which the flap is taken can be varied, depending on importance of the structures requiring soft tissue coverage. For example, fasciocutaneous Z-plasty flaps may offer more robust coverage over the ankle and its surrounding critical structures.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








