Flexor Tendon Repair
Bradon J. Wilhelmi
INTRODUCTION
Flexor tendon injuries have long been considered one of the most challenging problems for hand surgeons. Poor results following flexor tendon repair in the fingers led one expert hand surgeon, Boyes, to state “Here in a small area we have two flexor tendons, one passing through the other in a close fitting sheath and snugly held to the proximal phalanx by a pulley which is unyielding so that either trauma or infection squeezes out the blood supply and the tendon dies of ischemia. Suturing of a divided tendon usually results in some thickening and this enlarged area cannot pass the constricting pulley and motion is prevented.”1 Furthermore, Bunnell coined the term “no man’s land” to emphasize the difficulties associated with injuries in this area of the digital sheath.2 If we exclude flexor tendon injuries within the digital sheath, however, the remaining flexor tendon injuries are not a problem. For injuries in no man’s land, adherence to certain surgical techniques and postoperative therapy programs can optimize results and finger motion. Harold Kleinert revolutionized the primary repair of acute flexor tendon injuries in the digital sheath, after others had treated them for decades in a staged fashion with grafts for years.3
ANATOMY
Accordingly, Verdan classified flexor tendon injuries by the location of transection relative to the extremity and their prognosis4 (Figure 77.1A). For simplicity, injuries are classified based on zones: distal to the flexor superficialis insertion (zone 1), within the digital sheath of the flexor superficialis and profundus (zone 2), palm (zone 3), within carpal tunnel (zone 4), and in the forearm proximal to the carpal tunnel (zone 5). In general, flexor tendons repaired in zones 1, 3, 4, and 5 have a better prognosis than those in zone 2.
The flexor tendons originate in the forearm with muscles arranged in three different layers: superficial, intermediate, and deep. The superficial layer consists of the pronator teres, flexor carpi radialis, palmaris longus, and flexor carpi ulnaris. The pronator teres, palmaris longus, and flexor carpi radialis are innervated by the median nerve, whereas the flexor carpi ulnaris receives stimulus from the ulnar nerve. The intermediate layer includes only the flexor digitorum superficialis, innervated by the median nerve. The deep layer consists of the flexor digitorum profundus, flexor pollicis longus, and pronator quadratus. The median nerve innervates the flexor pollicis longus, pronator quadratus, and index/middle finger flexor digitorum profundus. The small and ring flexor digitorum muscles are innervated by the ulnar nerve.
Within the carpal tunnel, nine tendons pass to their respective digits. The flexor pollicis longus is the most radial structure, inserting onto the thumb distal phalanx. The flexor digitorum profundus tendons are found along the base of the carpal tunnel, aligned in order to insert into the base of the distal phalanx of the index through the small fingers. The flexor superficialis tendons course under the carpal tunnel in a stacked array with the middle and ring tendon volar to the index and small finger tendons, which insert into the middle of the middle phalanx of each respective finger. In the palm, the flexor superficialis tendons are initially volar to the flexor digitorum profundus tendons. The flexor digitorum superficialis tendon decussates at the level of Camper’s chiasm, to allow the flexor digitorum profundus to become more volar in the finger. The flexor digitorum superficialis and flexor digitorum profundus tendons course in the finger in a fibro-osseous canal that is lined by synovium and reinforced by a pulley system.
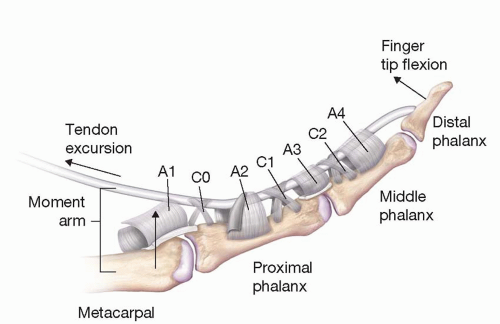
The fibro-osseous canal is comprised of pulleys with variable anatomy depending on their function. There are annular pulleys, labeled A1 to A5, and cruciate pulleys, labeled C0 to C4 (Figure 77.2). The A1, A3, and A5 pulleys prevent bowstringing of the flexor tendon across the metacarpophalangeal joint, proximal interphalangeal (PIP) joint, and distal interphalangeal joint, respectively. The A2 and A4 pulleys prevent bowstringing of the flexor tendon across the proximal phalanx and middle phalanx, respectively. The A2 and A4 pulleys are known as the critical pulleys because they are thicker, longer and in a more critical area than other annular pulleys, allowing them to aid in the prevention of bowstringing. A deficiency of 25% of either of these critical pulleys has the potential to result in the condition of bowstringing. Found between the annular pulleys, the cruciate pulleys (C0 and C3) are of less biomechanical and functional significance.
Digital flexor tendons receive nutrition from both intrinsic and extrinsic sources. The synovial fluid provides extrinsic nutrition with pumping action facilitated by flexion and extension of the fingers. Flexor tendons receive intrinsic nutrition by three sources, including longitudinal vessels entering the palm in the endotendinous channels, vessels that enter at the osseous insertion, and vincula (two short and two long). Most of the internal nutrition is delivered on the dorsal side of the tendon.
Flexor tendon function depends on many factors, including tendon excursion, intact pulley system, joint motion, and the presence of lubricating synovial fluid. Flexor excursion can be limited by adhesions among tendons, bones, and the synovial sheath. If bowstringing is present, greater amplitude of muscle contraction and greater amount of tendon excursion is required to close the fingertip to the palm.
DIAGNOSIS
Clinical exam provides the most accurate means of detecting flexor tendon injuries. When the flexor tendon is transected, the finger will have impaired flexion. Pain may limit the utility of this exercise and other examination maneuvers are required. Flexor tendon lacerations can be identified by observing a loss of normal finger cascade. Injuries to the flexor tendons can also be suggested by loss of tenodesis effect with passive wrist extension and flexion. Another useful technique to evaluate integrity of the flexor tendons can be compressing the distal forearm that normally brings the fingers into the flexed posture.
Diagnostic studies are occasionally helpful. Plain radiographs, magnetic resonance imaging, or ultrasound may help detect the location of the proximal tendon after closed zone 1 injuries (jersey finger injury). Knowing the location of the proximal tendon also assists in management. When the Flexor Digitorum Profundis (FDP) retracts to the palm (Leddy type 1), the tendon must be repaired within 2 weeks. When retracted to the PIP joint, the repair must be performed within 6 weeks (Leddy type 2). When caught at A4 pulley (Leddy type 3), the repair can be performed at any time.5 Fullness and tenderness at these locations, if present, direct management of jersey finger injuries making diagnostic studies unnecessary. The presence of neurovascular injuries should also be assessed for open lacerations at any level.
Partial tendon injuries are suggested in patients with pain on resisted flexion. On exploration, if the injury is more than 60% of the tendon in diameter, it should be repaired. If the injury is less than 60% of tendon diameter, the free edges are debrided to prevent catching on the pulleys.6
TREATMENT
Ideal flexor tendon repairs are strong and smooth. Strength allows for early active motion to prevent adhesion formation. Repairs should be strong enough to resist gap formation, which can be a site for adhesion formation or repair rupture. Repair techniques should also be smooth and not bunched to facilitate gliding of the tendons around adjacent structures such as pulleys or other tendons. Repairing flexor tendons within 24 to 72 hours minimizes adhesions, tendon retraction, and repair tension, along with gapping at the repair site and joint stiffness. Full exposure of the proximal and distal tendons usually requires extending the laceration in a zigzag (Bruner) or mid-longitudinal fashion (Figure 77.1B). The distal end of the tendon will be found more distally when the injury occurred with the finger in flexion. If the finger was extended at the time of injury, the proximal and distal tendon ends are found at the laceration level. Excessive manipulation of the flexor tendons should be avoided to minimize adhesion formation. Flexor tendons should be grasped in the core of the severed end to avoid epitenon injury that could be nidus for adhesion formation. In general, the technique of flexor tendon repair is dictated by the zone of flexor injury.
Repair Techniques
Several techniques of flexor tendon repair have been described over the years. Tendon repair strength has been shown to be proportional to the number of strands of suture placed across the repair site. There are multiple different types of suture material that can be used for flexor repairs, including Ticron, nylon, Ethilon, Mersilene, Prolene, and stainless steel wire. The ideal suture material is nonreactive, of small caliber, is strong, and with excellent knot-holding characteristics. The suture techniques have different grasping qualities depending on the cruciate, mattress, and cross-stitch configuration. Knots tied within the repair site may consume space and delay healing, whereas knots placed outside the repair may increase friction and adhesion formation. Suture placement may be better on the volar surface to avoid hindering blood delivery to the tendon, which is along the dorsal surface. Use of an epitendinous suture in addition to the core suture adds 20% to the strength of the repair.
Recently, the modified Becker technique (MGH, Massachusetts General Hospital) has gained popularity for its strength, resistance to gap formation, and endurance with active range of motion therapy.6,7,8,9,10,11,12 The MGH technique is like the Becker repair as it involves placement of four strands through the core in a criss-cross configuration13 (Figures 77.3A-B). However, the MGH is different in that the core sutures are 3-0 instead of 6-0 and includes augmentation with an epitenon suture and avoids the step-cut bevel.
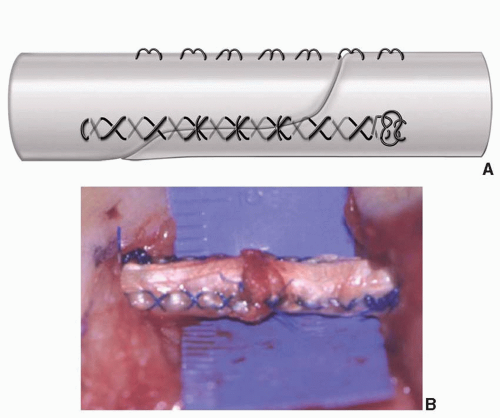 FIGURE 77.3. The MGH flexor tendon repair technique. (A) This technique is like the Becker repair as it involves placement of four strands through the core in a criss-cross configuration. (B). However, the modified Becker technique (MGH) is different in that the core sutures are 3-0 instead of 6-0, and it includes augmentation with an epitenon suture, avoiding the step-cut bevel. © Bradon J. Wilhelmi, MD.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|