(© 2016 Emergency Response Guidebook; source Transport Canada website; https://www.tc.gc.ca/eng/canutec/guide-menu-227.htm)
When a chemical comes in contact with body tissue and it causes a burn, it will continue burning while it remains in contact with the tissue. It is important for the first responder to consult Material Safety Data Sheets (MSDS) and to utilize on-site specialists when they are available to provide information about the product and how best to protect the first responder from potential exposures and to remove the chemical from the patient’s body tissue. Continuous flushing of the body area with running water is quite often what is prescribed to cool the burning, dilute/neutralize the substance. Acids and bases are common chemical properties. Acids should not be used to neutralize bases and vice versa; water is the best neutralizer.
10.3.1.3 Electrical Burns
Responder safety is the priority. Turning off/eliminating the energy source may be as simple as unplugging an appliance and as complicated as having your local power authority turn off/isolate energy to the area in which you will be performing a rescue or providing initial patient assessment and care.
10.3.2 Initial Patient Assessment
AVPU
A—Alert; acknowledge rescuers presence and engage in interaction
V—Verbal; respond to verbal stimulus
P—Pain; have a response to a painful stimulus
U—Unresponsive
AEIOU TIPS
A—Alcohol
E—Epilepsy
I—Insulin
O—Overdose
U—Uremia
T—Trauma
I—Infection
P—Psychiatric
S—Syncope
10.3.2.1 A-B-C-D-E-H
A: Airway Management with C-Spine Protection
Assess the airway for patency. Consider the mechanism of injury when assessing the airway. Is their soot around the nose? Is there swelling and soft tissue injuries in and around the airway that could result in the airway becoming blocked by edema? Superheated gases associated with fires can severely compromise a patient’s airway. Airway compromise associated with the products of combustion can happen very quickly; constant monitoring of the status of the airway is critical.
Can the airway be opened easily with a head tilt chin lift? Is there possible c-spine injuries that would necessitate a jaw thrust to open and maintain the airway? The responder airway should be prepared to aggressively manage the airway. BLS skills and adjuncts (oropharyngeal OPA and supraglottic airways) may not be enough to secure a patent airway. Advanced airways (endotracheal intubation) that can secure the lower airway may be necessary. If these resources are available in your jurisdiction, they should be activated as soon as possible. Airway compromise in burn victims is a highly probable life-threatening concern.
Application of an oxygen delivery devise such as a non-rebreather mask would be appropriate therapy for all burn patients.
B: Breathing and Ventilation
Is breathing effective and sufficient to support life? Are there structural injuries to the chest limiting the effectiveness of breathing? Ineffective breathing or the absence of breathing is life threatening and needs to be resolved or the patient can die.
The responder’s skill level will dictate how breathing is managed. BLS responders can use an OPA or a superglottic airway with a bag valve mask (BVM) to assist the patient’s breathing while ALS responders will utilize endotracheal tubes with a BVM.
C: Circulation
Burn injuries often result in a rapid reassignment of fluids. These fluids cause swelling at the burn sights and divert the fluids away from the circulatory system. The burn patient’s blood pressure should be monitored. Rapid assessment of the effectiveness can include pulse checks and electronic assessment (Electrocardiogram ECG) needs to be monitored.
Follow local protocols related to fluid replacement.
D: Disability (Brain Function)
This should have been considered during the LOC assessment, but the responder should use this opportunity to reassess and investigate further at this point.
E: Expose
- 1.
Jewelry can store heat energy and should be removed if it is likely to continue to transfer heat to the body.
- 2.
Edema is associated with burns; rings on fingers should be removed from fingers and toes should there be the potential for swelling in these digits.
- 3.
A rapid trauma assessment should be considered to see if there might be other injuries to the body; electrocution injuries can result in fractures and neurological deficits while blunt force trauma associated with falling debris in structure fires are easily missed if the rescuer is focused on the burn injury.
- 4.
Debriding of imbedded melted material should not occur in the field so as to minimize the potential of causing further injury during the removal.
- 5.
Initial assessment of the severity of the burn will also occur at this step.
The mnemonics CLAPS-D and TICS-D would be appropriate to use as part of a rapid trauma/body assessment (neck to knees) where undiscovered injuries could be life threatening if they are not discovered and managed.
C—Contusions
L—Lacerations
A—Abrasions
P—Penetrations
S—Swelling/Symmetry
D—Deformities/Distention
T—Tenderness
I—Instability
C—Crepitus
S—Subcutaneous Emphysema
D—Deformity/Distention
Life-threatening injuries should be treated when found.
H: History
SAMPLE is a mnemonic that will be a helpful tool for gathering and managing information that can be passed onto the next level of care while the mnemonic OPQRST can be useful to gather information about pain.
S: Signs/Symptoms
An assessment of “Signs” requires the responder to use all their senses.
Can you see the patient has partial thickness burns to most of their chest and they are having difficulty moving air? Can you see soot around the patient’s nose and mouth? Can you here “noisy” breathing? Can you smell the unforgettable sent of burning flesh? Can you see tissue involvement beyond the surrounding unbroken skin? Can you see entry and exit wounds associated with electrical burn injuries?
What can the patient tell you about their “symptoms”; pain they are feeling as a result of the incident? The mnemonic OPQRST can be helpful.
O: Onset
What were you doing when you started to feel the burning? When did you get burnt? Was the onset of pain gradual or rapid?
P: Provocation
What where you doing when you got burnt? Is there anything that makes you feel better or worse?
Q: Quality
Describe the pain to me? What does the pain feel like? (Avoid providing a “menu” as the patient is likely to pick from the menu just to shut you up.)
R: Radiation
Point to where it hurts the most and let me know if you feel pain anywhere else.
S: Severity
On a scale from 1 to 10, ten being the worst pain you have ever felt, rate your pain? (Don’t be surprised if you get an answer like “20”.)
T: Time
How long has the pain been going on? Has there been any change in the pain since the onset?
A: Allergies
Do you have any allergies? This may become important if the patient is allergic to antibiotics.
M: Medications
Are you taking any medications? What do you take the medications for? Where are your medications?
If readily available, the responder should gather medications for transport with the patient to a health care facility. The patient’s heath card (medical insurance) would also be good to obtain should it be available.
P: Past Medical History
Are there any medical conditions you have that we should be aware of?
E: Event Leading
You may have already captured this information during the OPQRST component of your interview. If this information has yet to be gathered, this should be a reminder to find out or reconfirm what the patient was doing when they sustained their burns.
10.3.3 Management of the Burn and Burn-Related Problems
While managing the care for any type burn patient, attention needs to be paid to airway, breathing, and circulation. Airways can become narrowed due to edema caused by exposure to superheated gases and chemical exposures. Breathing could be compromised by superheated gases/chemicals damaging the lungs or by a decreased ability to effectively expand the thoracic cavity as a result of burns to the chest. Circulation could be compromised as a result of the adverse affects of a chemical exposure or electrocution.
A careful balance is required between cooling and helping the patient maintain body temperature as a result of a decreased ability to self-regulate temperature. Once the flame is out and active cooling has been provided, open wounds require the placement of dry, sterile, burn sheets so as to decrease potential for infection. Wet dressings can cause issues with the body’s thermo-regulating system and possibly promote infection.
Chemical burns to the eye are common and require copious and continuous flow of water/saline to remove/dilute the chemical and stop the burning process. Avoid flushing chemicals from the affected eye to the non-affected eye. Consider removing contact lenses if possible as chemicals can become trapped under the lens, prolonging the exposure to the chemical.
Similar to synthetic clothing/fabric adhering to body tissue, hot tar creates a similar issue. The same rules apply in these types of burns; cool, cool, cool, do not remove the hardened tar that has adhered to underlying burnt tissue and transport to a burn center.
Cardiac issues; ventricular fibrillation, cardiac arrest
Burns below the surface; muscle, tissue damage, and fractures
Neurological damage; seizures
Entry and exit wounds
Pain management is a challenge. First responders will encounter patients suffering with pain associated with their burns. The active cooling by using volumes of water poured over the burn area may not provide sufficint relief. BLS providers may be allowed to assist the patient to take their own oral pain relief medication (ibuprophin). An ALS provider is likely able to administer IV analgesics like morphine.
10.3.4 Further Patient Management
Ongoing monitoring of LOC and vital signs should occur while the patient is awaiting transport through to transport to a higher level of care.
Ongoing assessment of burn injuries and changes in status should be monitored and documented.
Splinting and bandaging should be considered so as to limit the potential of further injury during transport. In general, dressings and bandages should be applied loosely so as to allow for swelling and to avoid cutting off distal circulation. When practical, pre- and post-packaging assessment of distal circulation, sensation, and mobility should occur so as to limit the likelihood that the treatment does not make the patient’s condition worse.
Loose/partial packaging will provide appropriate protection while allowing for assessment by the higher level of care during any transfer of care.
10.3.5 Transport and Transfer
Burn patients require attention by a higher level of care than is available outside a health care facility. Rapid transport to definitive care is ideal. Access to the closest emergency room may be necessary to provide appropriate care prior to transport to a burn center.
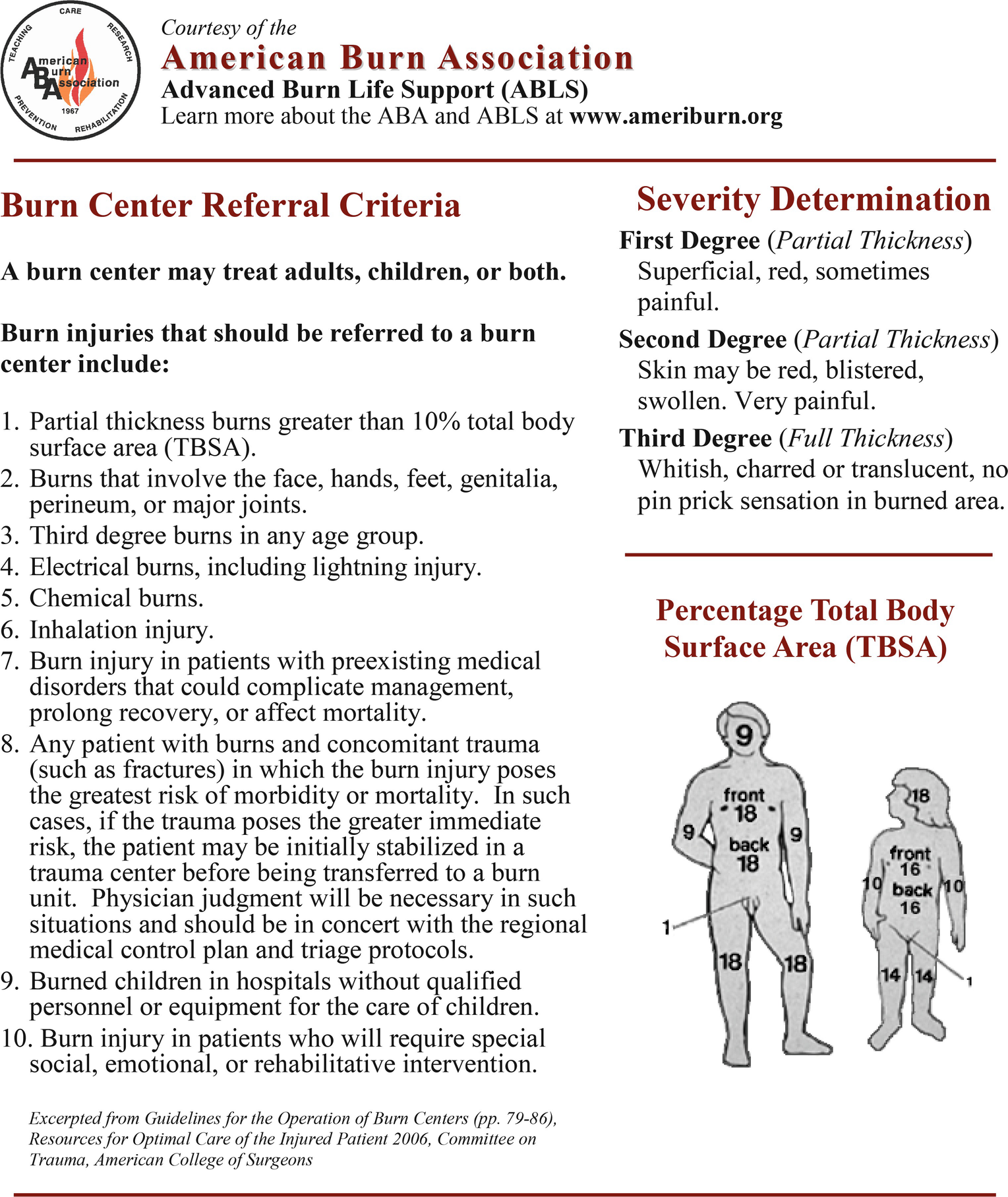
Consider the utilizing the American Burn Association’s Burn Center Referral Criteria’ document:

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








