Bacterial and viral infections are frequently associated with a rash and fever in children. Many of these rashes have known etiologies and characteristic features. Recognizing the pattern of the rash, and identifying key points in the history can help to establish the diagnosis. In Table 27-1, a number of pediatric exanthems are summarized, as well as some other rashes associated with fever. Most exanthems are self-limited and resolve in 7 to 10 days and only symptomatic treatment is needed.
| Disease/Etiology | History | Clinical Findings | Laboratory Studies |
|---|---|---|---|
| Viral | |||
Measles3–8 (rubeola) Paramyxovirus ssDNA | Incubation: 8-14 days Prodrome: fever, cough, coryza, and conjunctivitis Rash lasts 4-7 days | Erythematous macules and papules appear on scalp along hairline and behind ears. Spreads in cephalocaudal distribution (Figure 27-1) and by 5th day, clears in same distribution. Koplik spots (red macules with a white blue center) may be seen on the buccal mucosa. Complications: otitis, pneumonitis, encephalitis, and myocarditis | A fourfold increase in acute and convalescent titers (IgG) confirm diagnosis. IgM assay can be used for rapid diagnosis. PCR and ELISA are also available |
Varicella zoster virus dsDNA | Incubation: 10-21 days Prodrome: Malaise and low grade fever Late fall, winter, and spring | Tear drop vesicles, “dew on a rose petal” (Figure 27-2A and B). Multiple lesional stages present at once. Immunocompromised patients at increased risk of disseminated disease, pneumonia, and secondary infection. Reye syndrome associated with aspirin use. Congenital varicella is associated with hypoplastic limbs | Clinical diagnosis usually sufficient. PCR and DFA are available for rapid diagnosis, viral cultures take several days. Acute and convalescent IgM and IgG antibody titers confirmatory |
Cytomegalovirus (CMV) dsDNA | Postnatal infection in immune competent usually asymptomatic, but mononucleosis-like syndrome may occur | Erythematous macules and papules in diffuse distribution. Skin or mucosal ulcerations are possible. Complications include congenital CMV: “Blueberry muffin” baby resulting in hearing loss, seizures, and intracranial calcifications | Urine virus isolation, serologic evaluation, antigen (blood), and PCR analysis (blood). Skin biopsy may show intracytoplasmic, intranuclear viral inclusions in endothelial cells |
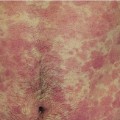
Mononucleosis Human herpesvirus 4 (HHV-4) Epstein–Barr virus dsDNA | Incubation: 30-50 days Prodrome: Fever, pharyngitis, lymphadenopathy, malaise, and anorexia. Rash following use of amoxicillin/ampicillin | Morbilliform rash spreads over entire body (Figure 27-3). Periorbital edema. Petechiae on palate (Figure 27-4). Painful mucosal ulcerations (especially vaginal/perineal) | Leukocytosis with 50% lymphocytosis. Elevated LFTs. Monospot test for IgM heterophile antibodies, usually positive by second week of infection. Not reliable in children <4 years due to low sensitivity |
Rubella7–9 (German measles) Togavirus ssRNA | Incubation: 16-18 days Prodrome: fever, headache, and upper respiratory symptoms | Rose-pink macules in cephalocaudal spread, and clears in 2-3 days in the same manner. May have soft palate petechiae (Forschheimer’s spots), posterior auricular/occipital lymphadenopathy. Self-limited. Complications: teratogenic (congenital rubella syndrome characterized by deafness, cataracts, congenital heart disease, and CNS signs), hepatitis, myocarditis, pericarditis, hemolytic anemia, and thrombocytopenic purpura. Arthritis in adults | IgM antirubella antibody presence, and/or a fourfold increase in IgG antirubella antibody are most diagnostic |
HHV6 dsDNA | Incubation: 5-15 days Prodrome: high fever for 2-3 days, followed by rash on trunk, which then spreads to extremities and face, for 1-2 days. Usually in children <3 years old | Erythematous, blanchable, macules, and papules. Periorbital edema is a common association. Rash appearing after fever defervescence is key finding. Complications: seizures secondary to fever | Serologic confirmation available with ELISA or PCR |
Parvovirus B197,8,10,11 (fifth disease, erythema infectiosum) Parvovirus B19 ssDNA | Incubation: 4-14 days Patients with fifth disease are no longer viremic at presentation. Patients with papular-purpuric gloves and socks syndrome are viremic at presentation Prodrome: headache and fever | Slapped cheeks (red plaques) at 1-4 days (Figure 27-5), then lacy reticular rash in 4-9 days, which can wax and wane for several weeks. Arthritis alone can be seen in adults as presenting sign. Associated “papular-purpuric gloves and socks” syndrome in adolescents. Complications: hydrops fetalis and aplastic crises in sickle cell patients | Clinical diagnosis is usually sufficient. Serologic studies available for detection of anti-B19 IgM and IgG antibodies. PCR studies also available. In a pregnant female who has been exposed to B19, serologic testing for IgM and IgG antibodies should be performed |
Hand, foot, and mouth disease7 Coxsackie A16 (most common serotype) Picornavirus ssRNA | Incubation: 3-6 days Prodrome: fever and malaise | Macules progress to vesicles on red base on the hands and feet (especially on palms and soles) and oral mucosa (Figure 27-6 A and B). Oral lesions are painful and quickly erode | Testing usually not indicated, but PCR is available |
Herpangina7 Coxsackie groups A and B most common, other echoviruses ssRNA | Incubation: 4-14 days Prodrome: fever Most common in children 3-10 years old | Oral erosions and ulceration in posterior pharynx and buccal mucosa. Exanthem usually absent | Testing usually not indicated, but PCR is available |
Gianotti–Crosti syndrome8,12 (acrodermatitis of childhood) Most commonly hepatitis B in developing countries, EBV in USA. Other causes include numerous viruses, bacteria, and vaccinations | Most common in spring/early summer. Most common in 2 year olds with range 6 months to 14 years old. May have associated low grade fever and lymphadenopathy. Hepatosplenomegaly less often | Symmetric papular eruption of face, buttocks, and extremities (Figure 27-7). Papules are pink, to erythematous, “juicy,” and have acral predilection | Evaluate for specific viral etiology, only if indicated |
Unilateral laterothoracic exanthem (periflexural exanthema of childhood) No confirmed etiology, but considered a viral exanthem | Most common in 2 year olds with range 6 months to 10 years. Preceded by URI or GI symptoms. Associated with low grade fever, lymphadenopathy, diarrhea or rhinitis, and pruritus | Rash usually starts in unilateral axilla and spreads in centrifugal fashion to contralateral side as the disease progresses (Figure 27-8). Erythematous papules, plaques with associated scale, with unilateral predominance. May appear urticarial | Laboratory tests not indicated |
Nonspecific viral exanthem7 Nonpolio enteroviruses (most common cause in summer) and respiratory viruses (most common cause in winter) | Prodrome: fever, myalgia, malaise, or gastrointestinal symptoms. Most are self-limited, resolve in 1 week | Blanchable erythematous papules and macules in diffuse distribution involving trunk (Figure 27-9), and extremities, and less often the face | Laboratory tests not required. Enterovirus culture can be obtained from throat or stool |
| Bacterial | |||
Scarlet fever7 Group A beta-hemolytic streptococcus (GABHS): pyrogenic exotoxin—A, B, or C | Incubation: 1-4 days Prodrome: fever, chills, sore throat, and headache. Signs of strep pharyngitis likely. Rash lasts 4-5 days Primarily a disease of children 1-10 years old | Clinical signs of streptococcal pharyngitis likely. Enanthem appears as white coating on the tongue, which sloughs in 4-5 days leaving the classic “strawberry tongue” (Figure 27-10). Fine, erythematous papules and macules (sandpaper-like rash), accentuated in flexures with petechial component (Pastia’s lines). Circumoral pallor characteristic. Rash resolves over 4-5 days and commonly heals with significant desquamation | Gold standard is throat culture with growth of GABHS. The rapid strep test has a high sensitivity and specificity. Antistreptococcal serologic studies are also available and may be useful |
Staphylococcal scalded skin syndrome8 (Ritter’s disease) Staphylococcus aureus, phage group II, exfoliative toxin (ETA, ETB) See Chapter 23 for more detailed information | Fever, malaise, lethargy, irritability, and poor feeding with rapid onset of generalized tender erythema. Cutaneous or systemic staphylococcal infection may be present | Tender erythematous lesions with flexural, perioral accentuation which progresses to large, superficial fragile blisters that rupture easily, leaving behind denuded, desquamating, erythematous, and tender (Figure 27-11). The Nikolsky sign (desquamation induced by slight rubbing of the skin) is positive | Culture of causative lesion (eg pustule, purulent conjunctivitis, surgical wound) if present. Blood cultures positive rarely Skin culture of rash will not yield organisms. The organism is most easily recovered from pyogenic (not exfoliative) foci on the skin, conjunctivae, nares, or nasopharynx See Table 23-5 for differential diagnosis |
Toxic shock syndrome (TSS)13,14 Staphylococcus aureus, TSS toxin-1 or streptococcal (GABHS) | Menstrual and nonmenstrual forms; the latter more common. Caused by toxin-producing strains of S. aureus. Prodrome of malaise, myalgias, chills precedes rash. Fever, lethargy, diarrhea, and altered mental status ultimately develop | Diffuse, scarlatiniform rash that later desquamates, palms, and soles involved. Accentuation in skin folds may be seen, and in rare cases, inguinal folds or perineal area may be only area of involvement. Hypotensive symptoms, shock, hyperemia of the mucous membranes and pharyngitis, “strawberry tongue.” Skin or muscle tenderness may be associated. Edema of hands/feet Streptococcal disease: Usually characterized by a focal tissue or blood infection with GABHS. Necrotizing fasciitis, myonecrosis may be associated. Extremely painful. Shock develops rapidly with renal impairment, DIC, and respiratory distress syndrome | Evidence of multiorgan involvement required. To meet criteria, 3 of 7 organ systems must be involved. Clinical diagnosis usually acceptable, but if positive culture or toxin production can be demonstrated, this is supportive. Biopsy not helpful usually. Leukocytosis, anemia, thrombocytopenia, elevated creatinine and CK, hypocalcemia, abnormal liver function studies, and evidence of disseminated coagulopathy may be present Cultures may be obtained from blood, throat, CSF, and peritoneal fluid. Tissue biopsy for culture if streptococcus is suspected |
Neisseria meningitides Serogroups A, B, and C | Incubation: 2-10 days, average is 4 days Presentation varies from fever to fulminant disease. Upper respiratory prodrome, followed by high fever and headache. Meningitis associated with stiff neck, nausea, vomiting, and coma. Leading cause of bacterial meningitis in children | Petechial rash of skin and mucous membranes. Other morphologies may be seen including macular (Figure 27-12), morbilliform, urticaria, and gray-colored acrocyanosis. Trunk and lower extremities are commonly involved. Palms, soles, and head tend to be spared. Extensive hemorrhagic lesions seen in fulminant disease. Progression to purpura fulminans (purpuric patches with sharply marginated borders, progressing to necrosis and eschar formation) when associated with consumptive coagulopathy. Autoamputation is a potential complication | Culture blood and CSF. Meningococci isolation from nasopharynx is not diagnostic. Petechial lesions may be cultured for organisms. Serology detecting N. meningitidis capsular polysaccharide antigen in CSF, urine, serum, and other bodily fluids is available. PCR available and useful if antibiotics already used |
| Multiple etiologies | |||
Urticaria multiforme16 Multiple etiologies | Upper respiratory infections, viral infections, and fever can occur as prodrome. Abrupt presentation of rash. Fever commonly associated | Abrupt presentation of annular erythematous wheals that may have associated central clearing (Figure 27-13). Generally widespread. Hand/foot edema common. May have associated lip swelling | Skin biopsy may be helpful if other entities are considered including erythema multiforme |
Serum-sickness like reaction (SSLR)16 Cefaclor most common cause. Amoxicillin, griseofulvin also described, among others | Develops 1-3 weeks after initiation of inciting drug with mild fever, rash, and joint pain | Targetoid or annular to polycyclic erythematous plaques. Violaceous center of plaques very characteristic | True vasculitis as seen in serum sickness reaction, type 3 immune mediated reaction is absent in SSLR |
HSV, mycoplasma, medications most common cause | Herpes simplex infection may precede rash | Targetoid erythematous plaques that are persistent and nonmigratory for days. Palm/sole involvement common | HSV titers, cold agglutinins for mycoplasma. Skin biopsy diagnostic |
Henoch–Schonlein purpura8 Etiology unclear, but linked to GABHS, viral infections, drugs, and immunizations | Small vessel vasculitis that occurs in children. Most common 2-11 years old. Antecedent upper respiratory infection suggests hypersensitivity phenomenon | Initial lesions appear urticarial, but quickly progress to purpuric (nonblanchable) papules with primary distribution on lower extremities (Figure 27-14) and buttocks. Scrotal involvement common. Edema of hands, face, feet commonly seen, especially in younger patients. Individual lesions resolve in 4-5 days. Associated with abdominal pain, arthritis, and glomerulonephritis | IgA immune complexes in affected organs. Direct immunofluorescence of skin specimens may document IgA, but absence should not exclude diagnosis. One-third of patients will have elevated serum IgA |
| No confirmed etiology | |||
Kawasaki’s disease8,17 (acute febrile mucocutaneous lymph node syndrome) Unknown etiology, but probably due to infection | Winter or spring most common. Most common in children <5 years old, peak incidence <2 years old | Need 4 of 5 criteria: (1) fever >5 days, (2) palmoplantar urticarial erythema/desquamation, (3) conjunctivitis, (4) strawberry tongue/red fissured, crusted lips, (5) cervical lymphadenopathy. A polymorphous rash on the trunk and extremities usually occurs presenting as a maculopapular, targetoid or scarlet fever-like rash with accentuation in body fold areas. “Atypical” cases more commonly diagnosed Complications: coronary artery aneurysms, myocarditis, and other cardiovascular disease | No reliable diagnostic test. The histopathologic features of a skin biopsy are nonspecific. Clinical diagnosis required |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree