Fig. 37.1
Infiltrating the donor site with Klein solution
The amount of solution injected is double the volume of the preestimated fat tissue requirement. The whole procedure of fat harvesting and “lipofilling” is performed according to Coleman’s technique [15]. After the injection of the diluted solution, a two-hole, 3-mm-diameter Coleman cannula with a blunt tip attached to a 10-ml Luer-Lok syringe is inserted through the small incision. A combination of slight negative pressure and the curetting action of the cannula through the tissues allows fat harvesting [2] (Fig. 37.2). The method of liposuction with different machine models or a manual syringe and different sizes and numbers of cannula holes has been not proven to affect fat cell survival. However, the “nontraumatic” blunt cannula technique is preferred rather than a sharp cannula technique [16–19]. Other harvesting techniques such as water-assisted liposuction or the Body-Jet system [20], Cytori Therapeutics’s Celution system [21], and Adivive’s Lipokit system are also available. There is a debate between open-system and closed-system techniques but there is no definite conclusion regarding the difference in fat cell survival and clinical results in each group. At the end of the lipoaspiration procedure, the access site of the cannula is sutured with fine absorbable material and a pressure dressing is applied.


Fig. 37.2
Harvesting the fat tissue with a Coleman cannula
There are different methods to process and purify the fat before grafting. The choice depends on several factors, such as the surgeon’s preference, costs, higher concentration of adipose-derived stem cells, volume requirement, and injection. Different techniques can be used:
1.
No preparation. This no-touch technique allows surgeons to inject the lipoaspirated fat into the recipient site without any preparation [22]. The advantages are that the specimen remains in a closed system and that it allows a shorter operating time compared with other techniques. However, it is suitable only when performing lipoinjection with small volume requirements, e.g., a few cubic centimeters to make a reconstructed nipple projection or a small linear scar correction. The disadvantage is the increase risk of calcification and cyst formation, because the oil is not eliminated.
2.
Mechanical preparation (centrifugation, decantation, or washing technique). The purpose of this technique is to remove cell debris, serum, tumescence solution, and the oily component from the adipocytes and the derivative cells. Centrifugation is the technique currently used by the authors [11, 12]. In our setting, the fat is centrifuged at 3,000 rpm for 3 min until the oily part and fluid are separated from adipose tissue (Fig. 37.3). The speed and duration of the centrifugation have no effect on adipocyte survival, but greater force seems to be better in removing oil and cell debris than lower centrifugal forces as was demonstrated by some authors [23]. Other authors prefer lower speeds and a shorter duration to avoid adipocyte damage [24] (Figs. 37.4 and 37.5). After the top (oily) layer and the bottom (fluid) layer have been removed, the middle (cellular) layer, which contains the adipocytes, endothelial cells, and mesenchymal stem cells, is immediately transferred to a 1-ml Luer-Lok syringe and prepared for injection [11, 12, 25].

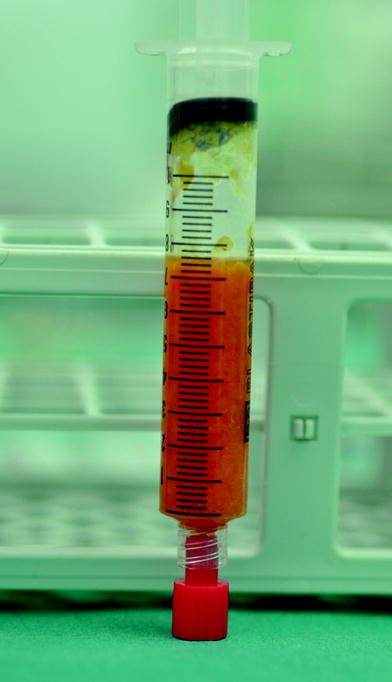


Fig. 37.3
Medical device for fat centrifugation
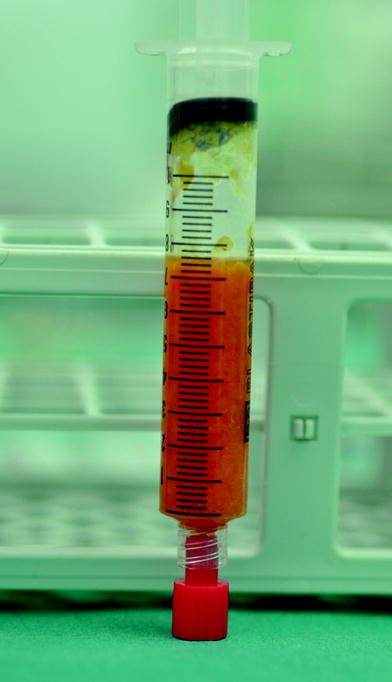
Fig. 37.4
Specimen before centrifugation

Fig. 37.5
Specimen after centrifugation
3.
Other methods of preparation (enzymatic and biological preparation). Some scientists try to enhance fat graft survival with fibroblast growth factor β [26]. Some surgeons divide the lipoaspirate specimen in half and prepare each half separately before putting them together and performing lipoinjection. An example of this technique is called cell-assisted lipotransfer. This process increases the number of adipose-derived stromal cells before fat injection [27, 28]. Cytori Therapeutics’s Celution system also prepares the fat by separation of two equal parts of a lipoaspirate specimen before mixing them together [21].
37.4.2 Recipient Site
The recipient site is prepared by preoperative marking and estimating the area which is required for lipoinjection. A suitable local anesthetic agent is injected around the defect prior to the injection of purified fat if the procedure is done with the patient under local anesthesia. Prepared cellular component is then injected into the defect area through a blunt Coleman cannula. Retrograde injection with a thin-layer, multiple-tunnel and fan or cylindrical shape technique is performed (Fig. 37.6). We avoid placing the fat as an excessive deposit, which may result in liponecrosis and graft loss. We judge the amount of fat needed to be grafted in each individual case on the bass of the tissue quality and the shape and size of the defect. If the anatomical site allows, we try to avoid intraparenchymal injection. In the case of tight fibrosis from a surgical scar or irradiated tissue, a sharp needle is inserted to break up the fibrotic scar and create a space for lipoinjection (Fig. 37.7). In general, we overcorrect the volume deficit by approximately 30–40 % depending on the reconstructive indication and recipient site tissue quality. After finishing the injection, we suture the entrance site of the injection cannula in a conventional fashion.



Fig. 37.6
Fat injection in the recipient site

Fig. 37.7
A sharp needle is used to release fibrotic scars
Some authors have proposed the use of an external suction machine on the donor site to produce subcutaneous tissue expansion and allow a larger volume of fat to be harvested and injected. This machine (Brava system) is not comfortable for patients and needs to be used during the night 1 month before and after the procedure [29].
37.5 Indications
37.5.1 Breast Conservative Surgery Defect Correction
A patient with breast conservative treatment usually receives conventional radiotherapy and this therefore leads to difficulty in selecting a reconstructive procedure. However, lipofilling offers a simple and reliable method which does not increase the complication rates in the breast conservative treatment patient.
Immediate reconstruction after breast conservative treatment. Lipofilling can be used for reshaping of the breast immediately after conservative surgery as a sole procedure or in combination with other oncoplastic procedures. A good indication would be in the case of a small breast and an upper quadrant tumor. A quadrantectomy can be performed and the defect can be closed with glandular sutures. The defect created by these sutures can be repaired by fat grafting in the subcutaneous space. Circumcavity injection is recommended and intracavity injection should be avoided.
Delayed reconstruction after breast conservative treatment. This is one of the major indications for lipofilling performed by the authors. It is possible to correct the defects and also increase the skin quality after radiotherapy damage. Depending on the dimensions of the defect, the correction can be done in one or more sessions. The procedure can be performed with the patient under local anesthesia in the case of a monolateral procedure and with the patient under general anesthesia in cases that need a contralateral procedure, such as a reduction mammaplasty (Figs. 37.8 and 37.9).

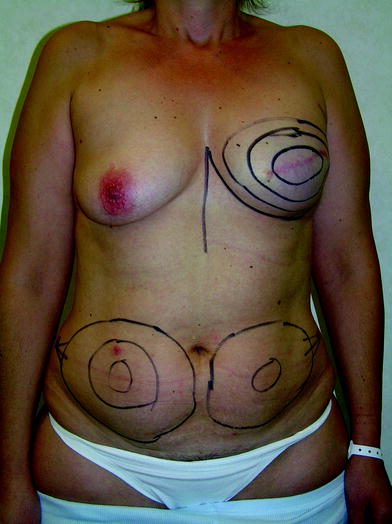
Fig. 37.8
Patient with huge asymmetry after right breast conservative surgery and radiotherapy

Fig. 37.9
Postoperative view after 250 cm3 of fat grafting in the right side and left reduction mammaplasty
37.5.2 Defects After Mastectomy and Breast Reconstruction
Lipofilling is a main technique in breast reconstruction after mastectomy and is indicated in the following situations:
Immediate breast reconstruction, Lipofilling in immediate reconstruction is very difficult owing to the lack of a surgical plane for fat implantation. In special cases with a small breast and huge flank lipodystrophy, an implant can be positioned at the same time as the mastectomy. After complete expansion, the reconstructive steps start with deflation of the expander and fat grafting to twice the volume deflated. After two or three fat grafting sessions, the expander can be removed and the nipple and areola can be reconstructed to achieve the final result without an implant (Figs. 37.10, 37.11, and 37.12),
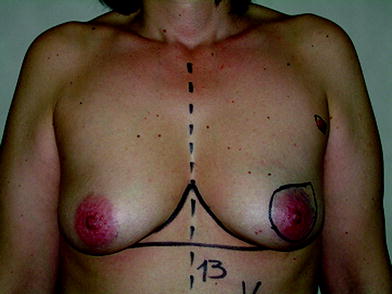
Fig. 37.10
Preoperative view before mastectomy and immediate breast reconstruction with a tissue expander