Facial Veins
 INTRODUCTION
INTRODUCTION
Many patients who present for treatment of leg veins are also concerned about appearance of vascular lesions on the face. We estimate that approximately 50 percent of patients seen for evaluation of leg veins have some form of vascular cosmetic blemish on the face. These blemishes commonly include telangiectasias that are both individual and relatively isolated or large groups of matted telangiectasias on the cheeks. Cherry hemangiomas are also seen, which are small, round, red to purple, dome-shaped vascular ectasias scattered anywhere on the face or body. In addition, some patients develop enlargement of venulectases that appear as purplish vessels on the cheeks, periorbital region, vermillion, and nasal alae. A standard terminology has been proposed that divides vascular lesions into hemangiomas, malformations, and ectasias.1–4
The first group, childhood hemangiomas, consists of proliferative lesions with endothelial hyperplasia. The second group, vascular malformations, results from anomalies of embryologic development, and in some of them, the abnormalities of the involved vessels are more functional than anatomic. The largest category is the ectasias; it is the most common type of lesion on the face for which adults request treatment (Table 17-1). Ectasias have normal endothelial turnover but have enlarged vascular spaces. Spider angioma, capillary aneurysm-venous lake, and telangiectases are examples not of vascular proliferation but dilatations of preexisting vessels. Our goal in treatment is to obliterate these vascular spaces or at least reduce their size so that they are no longer clinically apparent. For patients with rosacea, treatment can improve facial erythema and flushing as well.5
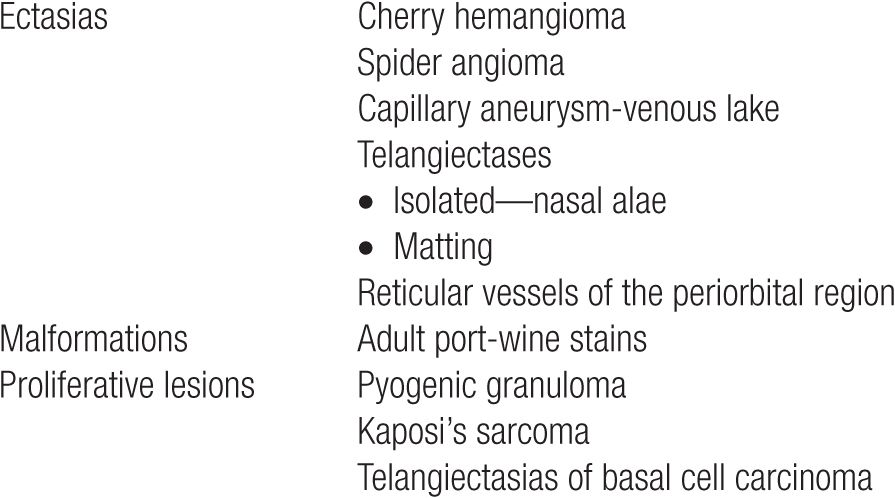
TABLE 17-1
Cosmetic or Medical Vascular Facial Lesions
Special Consent for the Face
Although the face typically heals well, patients should receive instruction as to the risks of purpura, edema, potential pigmentation changes, and scarring before such vessels are treated. Special care should be taken to ensure that the patient’s expectations are appropriate and informed consent documented in the medical record. Patients should fully understand that facial vessels will need to be treated a series of times. They should understand that these veins may recur and that they will periodically need treatments to maintain their results. Angiogenic factors may play an important role particularly in patients who have a genetic predisposition to facial vessels. The patient needs to understand that further sun exposure or flushing episodes may lead to recurrence. Patients should sign a specific consent form or a note written in the chart acknowledging this discussion before beginning treatment of any form. Appendix 17-A shows a sample consent form.
Considerations: Face Versus Legs
Fortunately, the treatment of facial telangiectasias is much more predictable than the legs. The skin heals quickly and is much less likely to scar with a similar depth of injury than on other body locations. Treatment results are often seen much more quickly as healing is much faster on the well-oxygenated skin of the face. Facial vessels also have the advantage of a more uniform depth than the legs. The vascular walls themselves are much thinner and uniform, and hydrostatic pressure typically plays no major role. Arterial pressure is occasionally a factor as seen in spider angiomata, with a small central pulsating arteriole that can be seen when a glass slide is gently pressed on the lesion surface. This is important when deciding on a method of treatment, as sclerotherapy into a bright red arteriole-fed vessel on the cheek incurs more risks of necrosis than the use of laser or light to shut down the branches and shrink the arteriole component. Any kind of residual indentation or imperfection following facial treatment is much less acceptable to patients when it is on their face rather than their legs.
Whereas the causes of telangiectasias on the legs are predominantly hydrostatic pressure, facial vessels appear to result from damage to the collagen of the vessel wall by sunlight. Sun exposure damages and weakens collagen specially with cumulative exposures, resulting in ectasia. A subset of the ultraviolet photodamage components is believed to cause a relatively high incidence of rosacea on the face. Rosacea symptoms typically include frequent flushing associated with facial erythema, telangiectasias, papules, and pustules. As more individuals exercise more frequently and vigorously, the incidence of facial flushing has been increasing. Vasodilators such as sildenafil used for erectile dysfunction may or may not play a role in increasing incidence. Whether diet may play a role with hormones used to increase food production for fowl and livestock is completely unknown. Repeated prolonged facial flushing leads to telangiectasias. Genetic factors also play a large role as the rosy cheek appearance passes from one generation to the next with individuals susceptible to rosacea. Aging of the skin (accelerated by sun exposure) causes more telangiectasias with collagen breakdown.6 Repeated trauma to the face will also induce localized erythema and ultimately vascular dilatation.
 METHODS OF TREATMENT
METHODS OF TREATMENT
Methods of treatment for facial telangiectasias include intense pulsed light (IPL), a variety of lasers, sclerotherapy, ambulatory phlebectomy, and historically, electrocautery (Table 17-2). Although all these methods of destruction carry risks of epidermal injury, electrosurgical units intentionally damage the epidermis as thermal, electrical, or radiofrequency (RF) energy is applied through it to reach underlying vessels. This is why we no longer recommend the use of thermal or RF electrocautery for the destruction of vessels when the avoidance of scarring is important. The immediate response to cautery typically appears as if successful elimination has occurred, but recurrence is common. Although nonspecific tissue destruction methods may work on occasion, the treatments of choice for the vast majority of facial vessels utilize selective photothermolysis of hemoglobin within the unwanted vessel. These devices include IPL and laser because of their selectivity toward the treatment of vessels with little disruption of the surrounding skin.
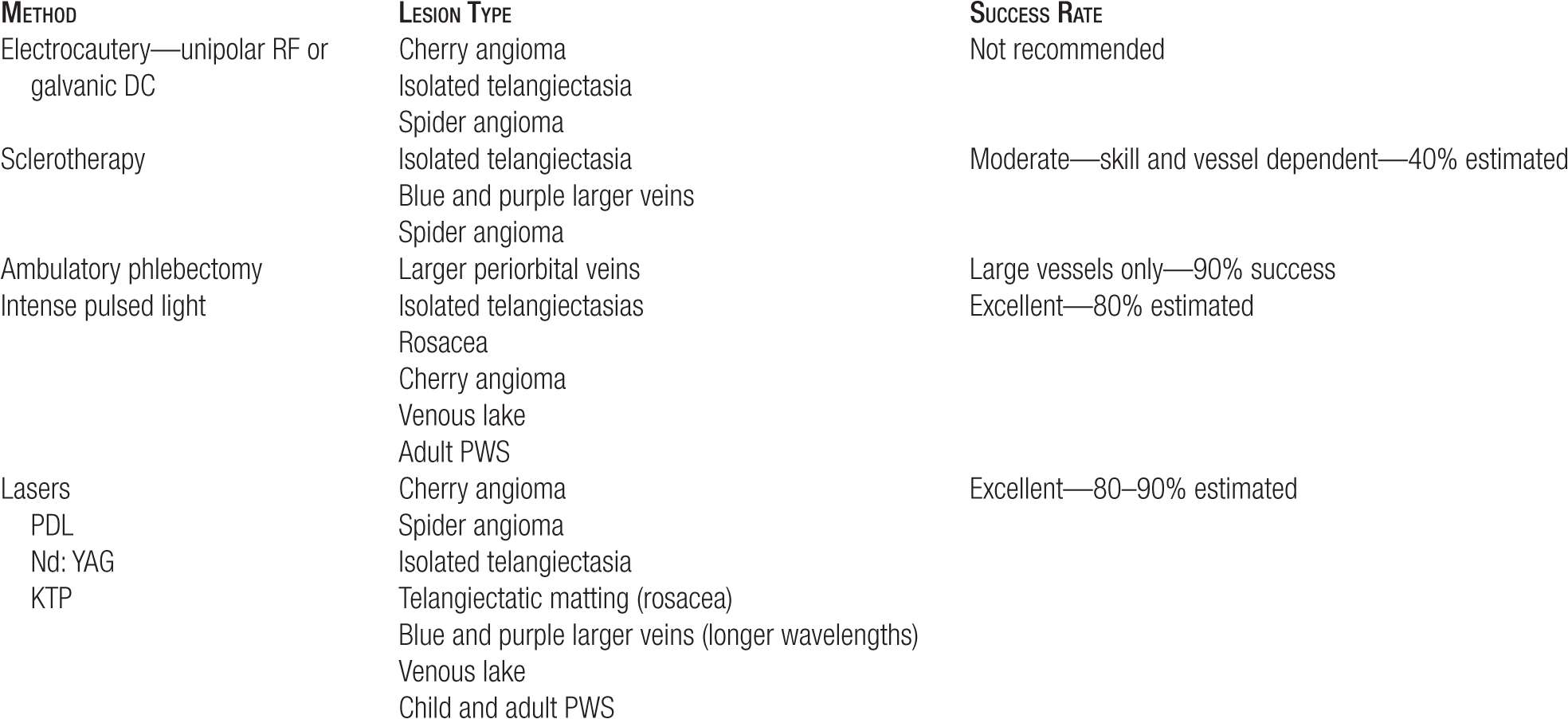
TABLE 17-2
Methods of Treatment for Facial Telangiectasias
Intense Pulsed Light
Intense pulsed light (IPL) consists of a noncoherent flashlamp that delivers controlled amounts of yellow, red, and infrared wavelengths to the skin. The advantages of this device are the large spot size and the ability to control pulse duration and pulse interval times. Some selection of wavelengths is possible by use of lower end cutoff filters. Multiple filters may be employed to gain more selectivity such as the design of the MaxG™ (Palomar Medical Technologies, Inc. 15 Network Drive Burlington, MA) head to the Palomar Starlux 500™ (Palomar Medical Technologies, Inc. 15 Network Drive Burlington, MA), which they have termed as OPL or optimized pulsed light. These devices satisfy the criteria for selective photothermolysis, permitting blood vessels to be selectively heated over the surrounding tissue. Pulses are typically separated to allow thermal relaxation time, in particular cooling of the epidermis in between pulses. Modern IPL units include contact cooling and sapphire crystals (more thermal conductivity) to protect the skin even further.
We have found IPL useful for grouped telangiectasias and telangiectatic mats on the face. It allows rapid treatment of an entire cheek (Figure 17-1). Typical parameters employed are modified according to vessel size and are summarized in Table 17-3. The large spot size footprint allows large areas to be treated rapidly. Purpura is uncommon; when bruising does occur, it fades very quickly in two to three days, rather than weeks as with the original 500-μs short pulsed dye laser (PDL). Efficacy in the treatment of facial telangiectasia, specially rosacea, with IPL is essentially equivalent to treatment with the longer pulsed duration PDL.7 The IPL devices that we recommend for this purpose include three components. Contact cooling is critical to minimize risks for skin burning, with temperatures best at 3°C–15°C. This is best achieved by the use of a water-cooled sapphire crystal. Secondly, the pulse duration must be sufficiently short for small, bright red telangiectasias, and thirdly, the fluence must be sufficiently high at these shorter pulse durations. Pulse durations need to be 10 ms or less, with fluence of 14–40 J/cm2 for a particular device. We utilize the Palomar Starlux LugG or MaxG handpiece at 10–20 ms and 30-40 J/cm2 and the Lumenis One device (LUMENIS, LTD. 13 hayetzira street yokneam, ISRAEL) at 3 ms, double pulse, with 10-20 ms off time between pulses at total fluence of 14–20 J/cm2. Extended pulse durations may be used for larger nasal telangiectasias with pulse durations of 40–50 ms.
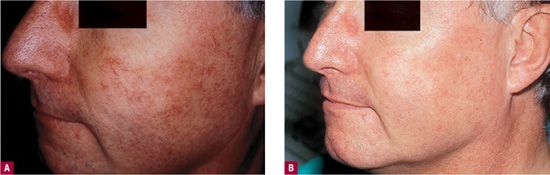
![]() FIGURE 17-1 Telangiectatic matting responds well to IPL. The frequency of rosacea episodes is typically diminished. A. Cheek of rosacea patient with widespread telangiectasia before IPL. B. After IPL.
FIGURE 17-1 Telangiectatic matting responds well to IPL. The frequency of rosacea episodes is typically diminished. A. Cheek of rosacea patient with widespread telangiectasia before IPL. B. After IPL.
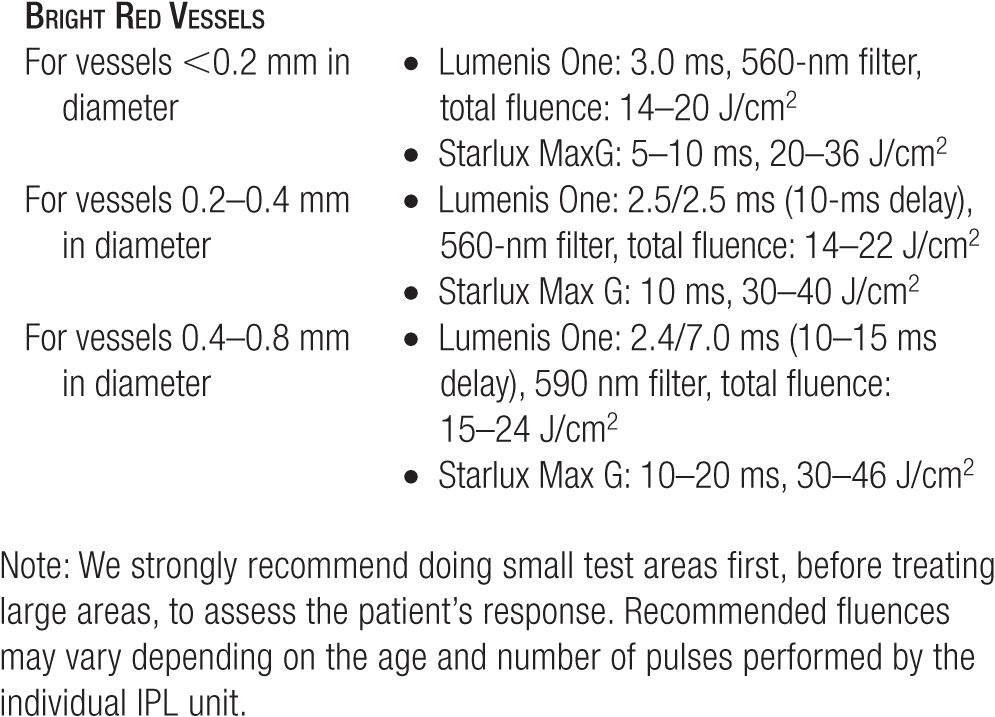
TABLE 17-3
Parameters for Facial Vessels for IPL: Do Not Treat Tanned Patients!
Lasers
The operation and principles of lasers are discussed in detail in Chapter 20. The success of green and yellow lasers for facial blood vessels is irrefutable. However, the side effects, speed of application, pulse durations, cost, and dependability vary widely depending on the machine. There are two primary differences in lasers for the face. One group has a relatively small spot size and requires tracing out each individual vessel. The others have a large spot and are used to treat whole cosmetic units of the face. Pulse duration is typically in the millisecond range, although those in the microsecond range (pulsed dye) tend to have higher risks of purpura. Purpura may not be tolerated by some cosmetic patients, but when it occurs, there is usually a higher clearance rate of the facial telangiectasia.8
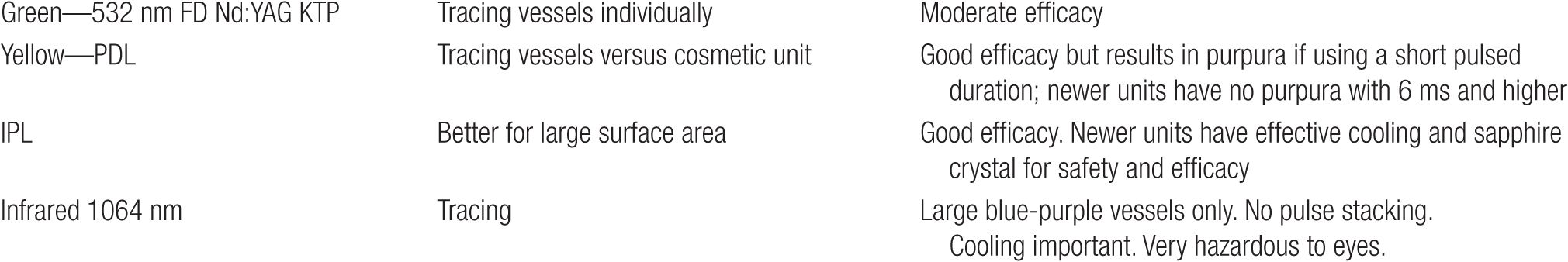
Newer generation PDLs have longer pulsed durations that can effectively treat vessels at nonpurpuric settings. Pulse stacking of nonpurpuric PDL settings increases the efficacy of vessel treatment.9 Green and yellow light lasers are used for smaller superficial blood vessels while the longer wavelengths, like 1064 nm, may be employed for larger purple vessels on the face. Table 17-4 lists the lasers commonly used on the face.
TABLE 17-4
Lasers Commonly Used on the Face
Some recent advances include PDLs with longer pulse durations coupled with special spot sizes such as the 10 × 3 mm elliptical spot size. Coupled with dynamic spray cooling, just before the laser pulse and extended pulse duration to 10–20 ms, facial vessels can be treated more effectively with less down time. Immediate contraction and photodarkening is the primary objective for best results.
In addition, the use of small spot at 532 nm to trace the vessels is an accepted method for resistant telangiectasias, especially on the nasal alae. The goal is to observe complete contraction that can often be observed with 532 nm, 2-mm spot, 12 J/cm2 with at least 1-s spacing between the pulses. Although neodymium: yttrium aluminium garnet (ND:YAG) 1064-nm laser is sometimes utilized for nasal vessels, caution should be exercised with 1064 nm, as excessive heat buildup may occur with pulse stacking leaving pockmarks on the nasal alae. At least 2 s should elapse between each 1064-nm laser pulse and skin cooling needs to be effective to reduce the risk of overheating and subsequent collagen overcontraction.
Sclerotherapy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


