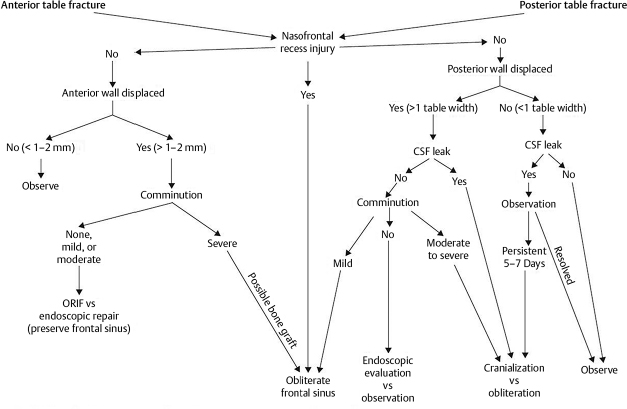
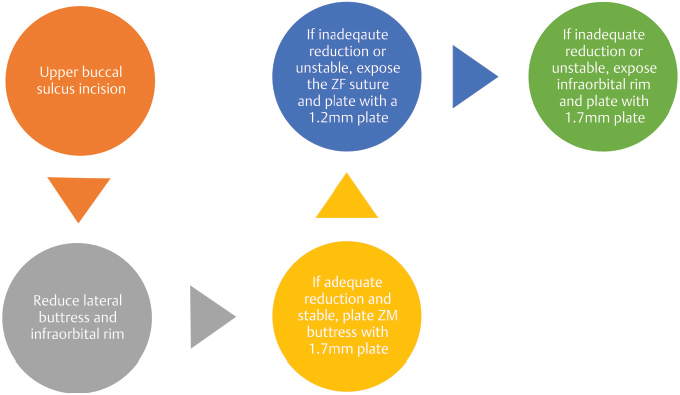
11 Facial Trauma Abstract This chapter will review facial trauma, and specifically facial fractures including mandible fractures, orbital fractures, zygoma fractures, and panfacial fractures. The reader will be able to analyze plain films and CT scans of these fractures and propose surgical plans, as well as describe incisions and explain management of intraoperative and postoperative events and poor outcomes. Keywords: facial trauma, panfacial fractures, zygoma fractures Six Key Points • Bilateral condylar neck fractures have anterior open bites; reapply maxillomandibular fixation if you see anterior open bite after removal. • Always fix stable to unstable (“top to bottom,” “lateral to medial”). • Complex fractures have discrete sequences of fixation. • Enophthalmos can be caused by increased bony orbit or by loss of soft tissue. • Diplopia can be caused by inadequate fixation or by muscle fibrosis. • Restoring buttresses is necessary. Mandible fractures affect the symphysis, parasymphysis, body, angle, ramus, subcondyle, and condyle. Because of the curvature of the mandible, it is common to have fracture in two places; and identification of one fracture should trigger examination for another fracture. Maxillomandibular fixation (MMF) will treat all mandible fractures provided occlusion has been set; open reduction and internal fixation, however, are preferred for those fractures that are amenable to it because of earlier return to function. The surgical sequence of mandible fracture fixation is as follows: arch bar placement, fracture exposure, occlusal and bone reduction, checking condyles are in glenoid fossae, rigid fixation, release intermaxillary fixation (IMF) and check occlusion, closure, and elastic application if needed. The first step of naso-orbitoethmoid (NOE) fracture repair is identifying the type of fracture (type 1, 2, or 3). Associated injuries are assessed. The repair will be determined by the type of fracture; while all require some sort of operative fixation, the reconstruction of the medial canthal ligament (MCL) will depend on whether the MCL remains attached to bone. The repair of NOE fractures consists, in general, of eight discrete steps: surgical exposure, identification of the medial canthal tendon, reduction and reconstruction of the medial orbital rim, reconstruction of the medial orbital wall, transnasal canthopexy, reduction of septal fractures, nasal dorsum reconstruction, and soft-tissue reconstruction.1 The clinical question in frontal sinus fractures is whether the frontonasal ducts are damaged. A frontal sinus fracture is, for that reason, potentially dangerous. If there is no nasofrontal outflow injury, the anterior table can be repaired. If there is nasofrontal outflow injury with obstruction, the sinus must be cranialized or obliterated (Fig. 11.1). On the films, air in the sinus is an indication that the sinus is draining. The anterior wall can be reconstructed with small plates, or with mesh if there is comminution. The sinus is obliterated by burring the bone, and filling it with bone and fibrin glue. If there is a displaced fracture of the posterior wall, there will be air-fluid levels and pneumocephalus, and neurosurgery must be involved. In cases of anterior and posterior wall injuries, as well as floor injuries, the sequence of repair is as follows: remove the posterior wall and dural repair (by neurosurgery), reconstruct the anterior wall, and put bone graft (with or without a flap) to the floor. Zygomaticomaxillary complex (ZMC) fractures are associated with orbital floor injury, and if the zygoma undergoes reduction and an orbital floor fracture becomes manifest, enophthalmos can ensue. Thus, the risk of enophthalmos because of an increased orbital volume is an indication for exploration. One should keep in mind that exposure of the inferior orbit has risk of scleral show.2 The sequence of steps is to reduce the lateral buttress, with the infraorbital rim if needed. If it is stable, no fixation may be necessary. If it is unstable, plate the ZM buttress with a 1.7-mm plate. If the reduction is adequate but continues to be unstable, the zygomaticofrontal (ZF) suture should be plated with a 1.2-mm plate. If after plating of the ZM buttress the reduction is inadequate and unstable, the ZF suture and lateral orbital wall should be exposed and plated. If after exposure and plating of the ZM buttress and the ZF suture there is still inadequate reduction and instability, the infraorbital rim should be exposed, reduced, and plated with a 1.7-mm plate (Fig. 11.2). Orbital fractures are significant because there is a precise balance between the bony orbit and the contents. The antrum and ethmoid are convex, and with fracture the contour becomes concave. Enophthalmos results from mismatch of the bony orbit and the contents—the concave contour causes an increase in the size (and thus, volume) of the bony orbit, and the contents settle into that concavity. Indications for surgical intervention of orbital fractures are the following: trapdoor fracture causing entrapment of muscles and restriction of ocular movement, potential for volume changes, or persistent diplopia. While postoperative enophthalmos should always trigger evaluation to ensure that there has been adequate reduction of the bony orbit, it is important to remember and counsel patients that the trauma itself can cause atrophy of the soft tissues, which can lead to enophthalmos (Table 11.1).
Overview
Mandible Fractures
Naso-orbitoethmoid Fractures
Frontal Sinus Fractures
Zygomaticomaxillary Complex Fractures
Orbital Fractures
Plastic Surgery Key
Fastest Plastic Surgery & Dermatology Insight Engine