I. EMERGENCY DEPARTMENT (ED) EVALUATION
A. History
1. Mechanism of injury determines the degree of force
a. Interpersonal violence (usually low energy)
b. Motor vehicle accident (usually higher energy)
2. History, prior facial trauma
3. Time of injury
4. Loss of consciousness?
5. Subjective complaints: Diplopia, blindness, hearing loss, malocclusion, and rhinorrhea
6. Environmental considerations: Chemical exposure?
7. Past medical/surgical history, medications, smoking, and drug abuse
B. Physical exam
1. Trauma patients: ABCs (airway, breathing, circulation) must be first priority
a. *Most facial trauma patients need clinical/radiographic cervical spine (c-spine) evaluation and management
b. *Over 10% of facial trauma patients have associated c-spine injury
2. Control hemorrhage—nasal packing, pressure dressing to lacerations
3. Adequate lighting, irrigation, and suction are required
4. Inspection: Lacerations, abrasions, burns, edema, symmetry, septal hematoma, and dental occlusion
5. Palpation
a. Skull, orbital rims, zygomatic arches, maxilla, and mandible
b. Assess for symmetry, step-offs, crepitus, and pain
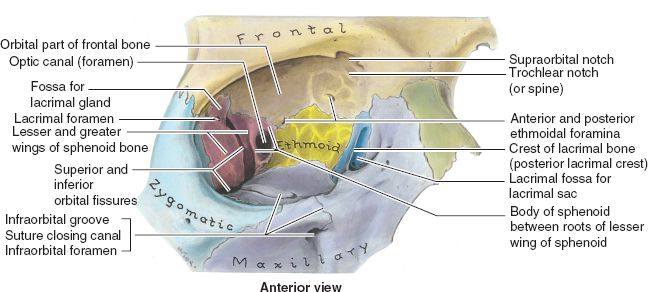
6. Complete cranial nerve exam (prior to administration of local anesthetic) with emphasis on
a. Sensation: Light touch in three divisions of CN V—ophthalmic, maxillary, and mandibular
b. Motor: Test all CN VII branches (temporal, zygomatic, buccal, marginal mandibular, and cervical) and look for asymmetry
7. Eyes
a. Test visual acuity with pocket card
b. Pupillary response to light
c. Swinging flashlight test to rule out afferent papillary defect (optic nerve injury)
d. Diplopia (horizontal versus vertical)
e. Extraocular movements
i. *Perform forced duction to rule out muscle entrapment if intubated/sedated and periorbital fractures present
ii. Grasp the sclera (away from cornea) with fine forceps and move the globe into upward/downward/lateral gaze positions to test for entrapment of extraocular muscles
f. Hyphema or globe injury
g. Enophthalmos
h. Eyelid position
i. Medial canthal tendon stability (versus telecanthus)
______________
*Denotes common in-service examination topics
a. Inspect external ear on all surfaces for lacerations, perichondral hematoma
b. Observe for Battle sign: Bruising of mastoid process indicative of skull base fracture
c. Otoscopy: Hemotympanum, cerebrospinal fluid (CSF) leak, perforation of tympanic membrane
d. *Hematoma on external ear must be evacuated and bolster placed
9. Nose
a. Assess contour of nasal bones
b. *Use nasal speculum for intranasal exam: Assess for lacerations, nasal obstruction, rule out septal hematoma (can lead to septal necrosis if untreated)
10. Midface, cheek
a. *Lacerations should be examined for proximity to Stenson’s (parotid) duct (runs in middle third of a line drawn from oral commissure to tragus)
b. Look for malar flattening and downsloping of palpebral fissure
c. Assess for midface mobility while stabilizing the skull
11. Mandible, oral cavity, occlusion
a. Assess occlusion
i. *Ask patient “Does your bite feel normal?”
ii. Inspect wear facets of teeth—these will intercuspate if occlusion is normal. This is very useful in unresponsive patients.
iii. Anterior or posterior open bite, cross bite
b. Document loose/missing/broken teeth
c. Inspect oral lining for lacerations or ecchymosis
d. Measure incisal opening distance
e. Submucosal hematoma may indicate mandible fracture
f. Palpate temporomandibular joint (TMJ) in external auditory canal with opening and closing of mouth
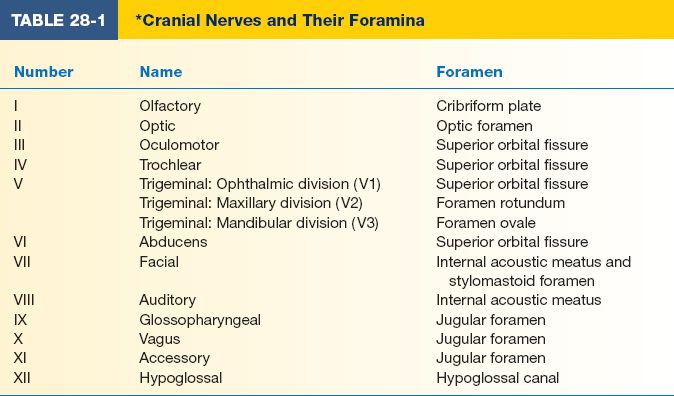
g. Note oral hygiene and any carious teeth that may serve as source of infection (Table 28-1)
C. Diagnostic studies
1. Maxillofacial CT is the gold standard to evaluate for facial fractures
a. Coronal views
i. Accurate assessment of nasal bones
ii. Orbital walls and potential herniation of contents into maxillary sinus
b. Three-dimensional reformats are useful in planning complex panfacial fracture reconstruction
c. Herald findings of fracture
i. Osseous deformity
ii. Sinus opacification
iii. Pneumocephalus or soft tissue air/edema
2. Obtain Panorex in cases of mandible fracture (this requires a patient to sit up in the panoramic radiograph device and therefore cannot be done in unresponsive patients)
3. Consider plain films, three views, to evaluate for missing mandibular segments (e.g., gunshot wounds); also useful when Panorex not available
D. Soft-tissue injuries
1. Facial field blocks are useful for providing anesthesia in awake patients (see Chapter 10—Fig. 10.7)
a. Supraorbital, supratrochlear, and infratrochlear nerves
i. Forehead/anterior scalp/upper eyelid/glabella
ii. Insert needle in midpupillary line at supraorbital rim, advance medially to capture supratrochlear nerve
b. Infraorbital nerve
i. Lateral nose/upper lip/lower eyelid/medial cheek
ii. Insert needle into superior buccal sulcus above the canine tooth root at midpupillary line 6 to 10 mm below the infraorbital rim
c. Mental nerve
i. Lower lip/chin
ii. *Insert needle into inferior buccal sulcus at second premolar
d. Cervical plexus, great auricular, transverse cervical nerves
i. Posterior auricle/mandibular angle/anterior neck
ii. *Both great auricular and transverse cervical nerves emerge at Erb’s point
a) 7 cm inferior to tragus
b) Posterior border of sternocleidomastoid (SCM) muscle
iii. Mark patient’s SCM when flexed, locate midpoint from clavicle to mastoid for injection
e. Auriculotemporal, great auricular, lesser occipital, Arnold’s nerve
i. Ear “ring block”
ii. Begin with needle at junction of lobule and cheek and proceed with four injections circumferentially
iii. Avoid superficial temporal artery
iv. Separate injection in external auditory canal for Arnold’s nerve (auricular branch of the vagus nerve, CN X)
2. Laceration repair
a. The face has a robust vascular supply; avoid excessive debridement
b. Repair in layers under minimal tension
c. Copious irrigation with normal saline, remove foreign bodies
d. Deep dermis: 5-0 interrupted buried absorbable sutures (e.g., vicryl and monocryl)
e. Skin: 5-0 or 6-0 interrupted or running permanent suture (e.g., nylon and prolene)
f. In young children, skin closure may be performed with 6-0 fast absorbing gut to eliminate the need for suture removal
g. Nonabsorbable sutures are removed in 5 to 7 days; delayed removal will result in suture tract epithelialization
h. Avoid undermining and/or local tissue rearrangement
i. Partial avulsions: Tissue present on small pedicles will usually survive
3. Scalp
a. Close with surgical staples or running locking absorbable suture (e.g., chromic gut)
b. Avulsions are indication for microvascular replantation
i. Scalp can tolerate 12 to 18 hours cold ischemia time
ii. Superficial temporal or occipital vessels can serve as recipient vessels during scalp replantation.
a. Direction of hair growth helpful in realigning wound edges
b. Inspect within the wound for occult fracture
c. Avoid cautery: Cicatricial alopecia
d. *Temporal branch of facial nerve: Pitanguy’s line
i. 0.5 cm inferior to tragus to 1.5 cm superior to lateral margin of eyebrow
ii. Deep surface of superficial temporal fascia (i.e., temporal parietal fascia) with superficial temporal artery
e. Advance lateral brow if necessary to close, medial brow position more aesthetically important
5. Eyelids
a. Conjunctiva meets the skin at grey line on lid margin
b. Ptosis on exam may indicate levator injury
c. *Rounding and mobility of medial canthus may indicate nasoorbitoethmoid (NOE) fracture (telecanthus) (normal intercanthal distance 32mm)
d. Epiphora (excessive tearing) indicates possible lacrimal canalicular injury
e. Repair techniques
i. Repair conjunctiva only if large defect present (e.g., 5-0 fast absorbing chromic)
ii. Repair tarsal plate (e.g., 5-0 Vicryl)
iii. Repair lid margin with vertical mattress at gray line using polyfilament (e.g., 6-0 Vicryl)
a) Eversion of closure prevents notching of lid margin
b) Avoids corneal abrasion from monofilament suture
c) May be removed in 5 to 7 days
iv. Keep all suture tails long, tied into an inferior suture knot away from globe
f. Lacrimal system injury
i. Canaliculus courses 2 mm perpendicular to lid margin then heads medially to lacrimal sac and nasolacrimal apparatus
ii. *Drains into nose at inferior meatus
iii. Laceration to medial third of eyelid ⇒ suspect canaliculus injury
a) Exploration: Place lacrimal probe in punctum and pass it into canaliculus, look for probe within the wound
b) Place silastic lacrimal stent; “Crawford tubes” (±suture repair of duct)
c) Stent remains in place for 2 to 3 months
d) *Jones I and II tests may be used clinically
6. Cheek
a. Stenson duct penetrates buccinator to enter oral cavity opposite second molar; travels with buccal branches of facial nerve
i. Probe intraoral papilla with 22G angiocath peripheral venous catheter and inject hydrogen peroxide: If duct is injured, visualize gas bubbles in wound
ii. Repair duct to prevent sialocele, or leave drain
iii. *If sialocele develops, aspirate and apply pressure dressing
b. Nerve injury—can use nerve stimulator up to 48 to 72 hours later
i. Considerable crossover between zygomatic and buccal CN VII branches
ii. Does not require repair if medial to lateral canthus
7. Nose
a. Redundant arterial supply: Lateral nasal, external nasal, septal, and columellar arteries
b. Septum composed of septal cartilage, vomer bone, perpendicular plate of ethmoid, maxillary crest, and premaxilla
c. Septal hematoma
i. Evacuate with needle aspiration or blade to prevent necrosis and septal perforation
ii. Place running quilted 4-0 gut suture
i. Mucosal lining: 4-0 chromic with knots in nasal cavity
ii. Cartilage: 5-0 clear nylon or monocryl
iii. Skin: 6-0 nylon in the skin
e. Avulsion injuries: Consider composite graft (replantation if possible)
i. 50% failure
ii. All grafted material must be within 5 mm of viable tissue
8. Ears
a. Arterial supply: Superficial temporal and postauricular arteries
b. Great auricular, auriculotemporal, Arnold, lesser occipital nerves provide sensation
c. Otohematoma
i. Evacuate with needle or blade to avoid “cauliflower ear”
ii. Compression dressing
a) Xeroform bolster mattressed with 3-0 through and through sutures
b) Remove in 1 week
d. Lacerations
i. May require figure-of-eight sutures in cartilage (clear nylon or absorbable monofilament)
ii. Evert skin margins in key locations (e.g., helix) with mattress sutures
e. Amputation
i. Partial amputation—suture repair
ii. Complete amputation—attempt replantation
iii. Consider leech therapy for venous congestion
iv. Consider dermabrasion of ear part and banking cartilage in dermal pocket
9. Mouth
a. Anatomic landmarks: Philtral columns, philtral dimple, Cupid bow, ver-million border, and white roll
b. Lacerations: Repair mucosa, orbicularis, and skin in layers. Mark white roll with methylene blue or marking pen prior to administration of local anesthetic
II. FRACTURE EVALUATION AND MANAGEMENT
A. Mandible fractures
1. Anatomy (Fig. 28-1)
a. Mental nerve (CN V3)
i. Exits skull base from foramen ovale
ii. Courses 2 mm below foramen
iii. *Exits mental foramen at second premolar
iv. *Nerve is closest to buccal cortex at third molar, farthest from buccal cortex at first molar
b. Muscles of mastication (CN V3) exert deforming forces of mandible
i. *Lateral pterygoid: Protracts (lowers) mandible
ii. Medial pterygoid: Closes mouth
iii. Temporalis: Elevates and retracts mandible
iv. Masseter: Elevates mandible
v. Geniohyoid, genioglossus, mylohyoid, digastric muscles: Depress mandible
2. The mandible is like a pretzel: Difficult to break in only one location; look for second fracture
3. Classification of fracture—location on mandible, simple versus comminuted, open versus closed, and intracapsular/extracapsular
4. Teeth in line of fracture should be retained if roots are not fractured
5. MMF (maxillomandibular fixation; also called intermaxillary fixation, or IMF) may be used as a single modality (controversial) for 4 to 6 weeks
6. Principles of ORIF (open reduction and internal fixation)
a. Indications: Displaced fracture with abnormal occlusion
b. MMF to restore occlusion
Figure 28-1. Mandible anatomy. (Asset provided by Anatomical Chart Co., 2013.)
c. Subperiosteal dissection to expose fracture line
d. Reduction of fracture fragments
e. Rigid fixation using plates/screws, 2.0 mm plating systems
f. Early, active mobility
g. Tension band plate placed along alveolar border
h. Large reconstruction plate along inferior border
7. Fracture subtypes
a. Symphyseal/parasymphyseal fractures. Miniplate fixation with at least two points of fixation
b. Body fractures. Miniplate fixation
c. Angle fractures. Highest complication rate
d. Coronoid fractures-MMF for 2 weeks usually enough
e. Condylar and subcondylar fractures
i. Intracapsular
a) Condylar fractures (head and upper neck)
b) Closed reduction and limited (2 weeks) MMF with early controlled mobilization; rarely ORIF
c) *Open treatment warranted if: (1) Cannot reduce fracture and it precludes ranging the mandible, (2) a foreign body is present within the TMJ, (3) the condyle has displaced into the middle cranial fossa, and (4) bilateral condyle fractures with midface fractures to restore vertical height
ii. Extracapsular
a) Subcondylar fractures
b) IMF × 4 to 6 weeks, weekly observation of occlusion after release
f. Pediatric mandible fractures
i. *Avoid immobilization; early active therapy; growth potential allows improvement of occlusion with time
ii. May require MMF
iii. In the absence of permanent dentition
a) Piriform drop wires
b) Circum-mandibular wires
i. Closed fractures with minimal displacement: No dentures, soft diet
ii. Open fractures or those with displacement: ORIF with load-bearing plate
h. Dislocations
i. Anterior displacement of condyle from glenoid fossa
ii. Closed reduction necessary
a) Conscious sedation
b) Intraoral downward and posterior pressure at ramus
8. Indications for tooth removal
a. Grossly mobile
b. Severe periodontal disease
c. Root fracture
d. Exposed apices
9. Common complications
a. Malocclusion/malunion/nonunion
b. Increased facial width, rotation of mandible
c. TMJ ankylosis: Stiffness, pain, limited range of motion
d. Infection: Often treated with I&D, hardware removal generally not required
B. Zygoma fractures
1. Anatomy
a. Zygoma has a quadrilateral shape: Articulates with maxilla, sphenoid, temporal, and frontal bones; fractures are therefore “tetrapod fractures”
b. Muscle attachments: Masseter, temporalis, zygomaticus major and minor
2. Clinical presentation
a. *Flattening of malar eminence with downslanting palpebral fissure: Lateral canthus attaches to zygoma via Whitnall tubercle
b. Zygomatic arch fractures may limit the motion of coronoid, resulting in trismus
c. Enophthalmos
d. Infraorbital paresthesia
3. ORIF: Required to restore facial width, malar projection, and orbital dystopia
a. Approaches
i. Upper blepharoplasty incision: Access to zygomaticofrontal junction
ii. Coronal incision: To expose entire arch and lateral orbital rim
iii. Gillies approach
a) Temporal incision behind hair line
b) *Dissect deep to temporalis muscle fascia
c) Reduce posteriorly displaced arch fracture with outward force
iv. Transconjunctival incision: Access to zygomaticomaxillary junction (and orbital floor)
v. Intraoral incision: Dingman elevator placed under arch with outward force
b. Fixation: 1.5- or 2.0-mm plating systems
c. Postoperative arch splint: May wrap tongue depressor in silk tape and bend into bridge shape, secure to face with tape as buttress to prevent infracturing during sleep (not needed when plated)
d. Zygomaticosphenoid articulation is the most important to assess reduction
C. Orbital fractures
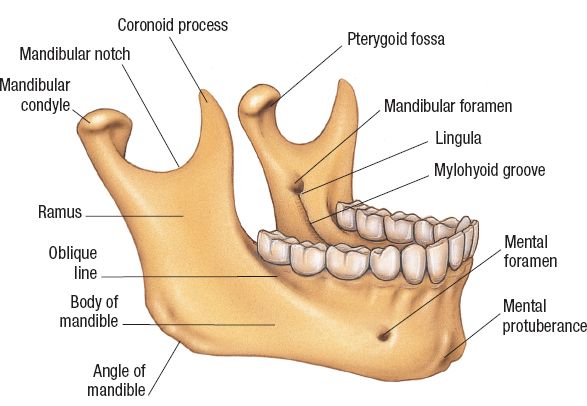
1. Anatomy (Fig. 28-2)
a. Orbit is constructed of seven bones—maxilla, zygoma, sphenoid, frontal, palatine, lacrimal, and ethmoid
b. *Conical/pyramid shape: Optic nerve is ~4 cm posterior to orbital rim
c. Thinnest region is medial wall (lamina papyracea)
2. All orbital fractures require consultation with ophthalmologist to evaluate for ocular trauma
3. Fractures most common in orbital floor and medial wall (lamina papyracea of ethmoid)
Figure 28-2. Skeletal orbital anatomy and the relationship of the superior and inferior orbital fissures and optic foramen. (From Moore KL, Dalley AF II. Clinical Oriented Anatomy. 4th ed. Baltimore, MD: Lippincott Williams & Wilkins; 1999, with permission.)
4. Dystopia occurs if loss of bony support
5. Enophthalmos
a. Fractures of orbit result in increased intraorbital volume and disrupt ligamentous support of globe
b. During healing, periorbital takes on shape with smaller volume
6. Clinical presentation
a. Periorbital edema
b. Periorbital ecchymosis
c. Diplopia
d. Infraorbtial nerve paresthesia
e. Enophthalmos
f. Orbital rim step-off
g. Limited globe excursion from edema or entrapment
7. Indication for ORIF
a. Persistent diplopia (>2 weeks)
b. Fractures that involve >50% orbital floor or >2 cm2
c. Clinically significant enophthalmos
d. *Entrapment of extraocular muscles (requires emergent intervention, i.e., less than 24 hours, to release ischemic muscle). Entrapment is determined by assessing extraocular movements or by forced duction testing (see above, under ED Evaluation and Physical Examination) if unconscious.
8. ORIF
a. Subciliary, transconjunctival, inferior orbital rim incisions
b. *Transconjunctival approach is associated with lowest rate of postoperative ectropion
c. Medpor (porous polyethylene) implant or cranial bone grafts can be used to reconstruct the orbital floor: Secured in place with screws at infraorbital rim
d. Young children may present with a “trapdoor” floor fracture in which there is no defect but the fracture has entrapped the extraocular muscle (usually the inferior rectus muscle). The muscle can be released and the orbital floor usually needs no implant or reconstruction if it feels stable.
9. Associated potential ophthalmic consequences
a. Corneal abrasion
b. Hyphema: Blood in anterior chamber
c. Sympathetic ophthalmia
d. Traumatic optic neuropathy: Traumatic loss of vision
i. Requires surgical decompression, and high-dose steroids
e. *Superior orbital fissure syndrome
i. Effects oculomotor, trochlear, abducens, and trigeminal (lacrimal, frontal, and nasociliary branches) nerves and ophthalmic vein
ii. Signs
a) Ptosis
b) Proptosis
c) Ophthalmoplegia
d) Numbness in VN V1
e) Dilation and fixation of ipsilateral pupil
f. *Orbital apex syndrome: Same as superior orbital fissure syndrome but with loss of vision due to injury to optic nerve
g. Traumatic carotid cavernous sinus fistula
i. Proptosis
ii. Ocular bruit
iii. Ophthalmoplegia of CN III, IV, or VI
iv. Treatment: Surgical ligation of carotid artery or coils to block off fistula
D. Nasal bone fractures
1. Nasal anatomy
a. Upper one-third of the nose: Paired nasal bones
i. Fractures common in thinner lower halves of paired nasal bones
ii. Younger patients experience fracture–dislocations of larger segments
iii. Older patients develop comminuted patterns
b. Lower two-thirds of the nose: Paired upper lateral cartilage, lower lateral cartilage
c. Septum consists of quadrangular cartilage, vomer, perpendicular
2. Treatment goals
a. Restoration of function and appearance
b. Wait 6 months before considering revision rhinoplasty or secondary closed reduction plate of ethmoid bone
c. Acutely before edema begins (uncommon) or after swelling resolves (3 to 5 days)
d. Closed reduction should be accomplished within 2 weeks of injury to avoid osteotomies
3. Principles and technique
a. Look for septal hematoma
b. Do not misdiagnose NOE for simple fx as NOE is hard to fix
c. Usually treat closed except with complex facial fractures, inability to obtain good closed reduction, severe comminution
d. External nose anesthetized by regional block 0.5% lidocaine with 1:200,000 epinephrine
e. Internal nose anesthetized by afrin-soaked pledgets
f. Reduce bridge with elevator and septum and Asch forceps or butter knife
g. Nasal bone must be mobilized before reduction
h. External thermoplast splint and internal nasal splints placed after reduction
4. Complications
a. Subperichondral fibrosis with partial obstruction
b. Synechiae
c. Obstruction of the nasal vestibule from malunited fractures or scar contractures from loss of vestibular lining
d. Osteitis
e. Malunion of nasal fractures with residual deviation
1. Fractures of nasal bones, frontal processes of maxilla, lacrimal bone, and ethmoid bone
2. Markowitz classification: Based on central fragment with medial canthal tendon
a. Type I: Single, noncomminuted, central fragment without medial canthal tendon disruption
b. Type II: Comminuted central fragment without medial canthal disruption
c. Type III: Severely comminuted central fragment with disruption of medial canthal tendon
3. Clinical presentation
a. *Telecanthus (not always seen acutely): Normal intercanthal distance is 30 to 34 mm
b. Foreshortened and depressed nose
c. Lack of nasal support on palpation
d. Subconjunctival hemorrhage
e. CSF rhinorrhea
f. Mobility of the medial canthus on bimanual exam
4. *Commonly includes medial canthal ligament-bearing bone
a. Fracture line through anterior and posterior lacrimal crest
b. Leads to traumatic telecanthus
c. Possible damage to nasolacrimal system, leading to epiphora
5. Septal cartilage fractures: Progressive deviation from warping forces due to perichondrium
6. Treatment
a. Principles
i. Rule out brain injury (frontal lobes, dural tears, and bone fragments in the brain) and coordinate with neurosurgery
ii. Early intervention (very difficult to fix if done as a late reconstruction
iii. Wide exposure; reduce and stabilize anterior orbital rim; restore internal orbital architecture with bone graft; reconstruct glabella, upper nasal region, medial canthi; and release soft tissue
b. Exposure
i. Usually required two to three separate incisions
ii. Nasofrontal area: Through laceration, midline nasal, or coronal incision (best exposure)
iii. Subciliary or transconjunctival: with lateral canthotomy
iv. Upper buccal sulcus: May be required to obtain adequate reduction
c. Technique
i. Subperiosteal dissection to inferior orbital rim and floor
ii. Asch forceps used intranasally to elevate and reduce nasal fragments
iii. Do not detach canthal ligament from bone fragment if avulsed
iv. Preserve medial canthal ligament attachments to the bone
v. Preserve lacrimal sac and nasolacrimal duct attachment to the bone
vi. Isolate segments containing canthal ligament, place in perfect anatomic reduction, and stabilize with rigid fixation
vii. Preserve and attach all bone fragments
viii. Reduction, rigid fixation
a. Plates/screws if canthal-bearing segment is large enough
b. If canthus is avulsed from bone, reposition using transnasal wires
c. *Vector of wire fixation: Posterior and superior
ix. Bone graft often needed for medial orbital wall and floor and for restoration of nasal dorsum height and contour (cantilever cranial bone graft or rib graft)
x. External splinting 2 weeks
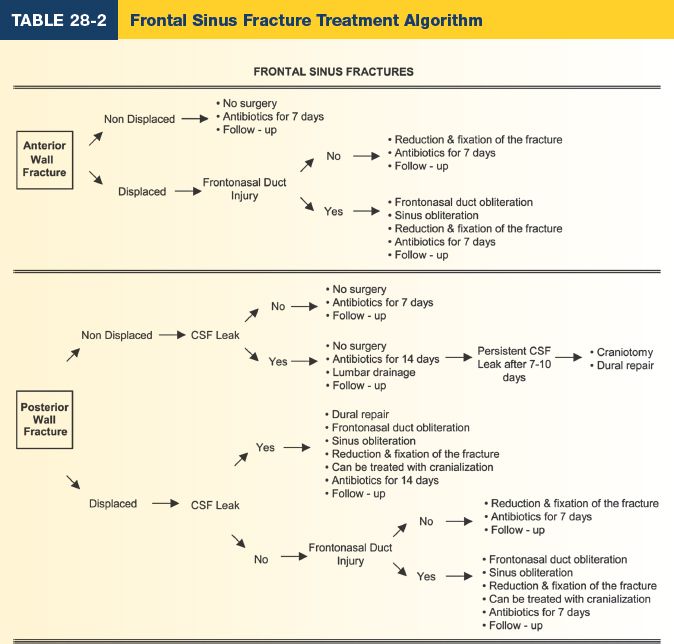
F. Frontal bone/sinus fractures
1. Anatomy
a. Thick anterior table, thin floor (orbital roof), and thinner posterior table
b. Nasofrontal duct is posterior medial in location and runs through anterior ethmoid bone
c. Drains into middle meatus
d. *Not present at birth, begins to develop at 2 years old, and does not reach adult size until 12 years old
2. Fracture classification
a. Anterior table
b. Posterior table
c. Nasofrontal duct involvement
3. *Forces of 800 to 2,200 lb are required for frontal sinus fractures, 2 to 3× greater than any other facial bone
4. Frequently associated with NOE and midface fractures
5. Clinical presentation
a. Palpable deformity to frontal bone
b. CSF rhinorrhea
c. Paresthesia in pattern of supraorbital and supratrochlear nerves
d. Inferior globe displacement of orbital roof
6. Complications
a. Mucocele; pyomucocele
b. Osteomyelitis
c. Infection of orbital contents
d. CSF rhinorrhea
i. Halo test/ring sign: Fluid is placed on gauze and concentric rings of blood and CSF form, indicating CSF leak
ii. Fluid can be sent for beta transferrin level to confirm leak
7. Indications for operative management
a. Displaced anterior table (leads to contour deformity)
b. Nasofrontal duct involvement or obstruction (leads to mucocele)
c. Depressed posterior table
8. Treatment goals
a. Restoration of contour
b. Isolation of cranial cavity from upper airway
c. Construction of safe sinus
9. *Operative management
a. Displaced anterior table
i. ORIF with low-profile miniplates
ii. If comminuted, IO wiring may be needed
iii. Nasofrontal duct obstruction or posterior table displacement with minimal or no CSF leak. Obliteration of sinus with bone, fat grafts, or pericranial flaps after exenteration of sinus mucosa
b. Posterior table fracture with CSF leak: Cranialization
i. Exenterate sinus mucosa
ii. Remove posterior table allowing the brain to fill potential space
c. Nasofrontal duct obstruction can result in mucopyocele. To test for patency: Instill methylene blue into sinus and place cotton tip applicator (i.e., Q-Tip) endonasally for confirmation of flow (Table 28-2)
G. Maxillary fractures
1. Anatomy
a. Four processes: Frontal, zygomatic, palatine, and alveolar
b. Contains maxillary sinus
c. Muscle attachments include facial expression muscles anteriorly and pterygoid muscles posteriorly
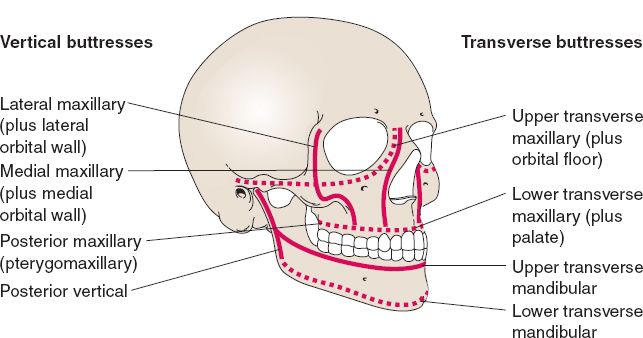
d. Three major buttresses that provide strength (Fig. 28-3)
i. Nasomaxillary
ii. Zygomatic
iii. Pterygomaxillary
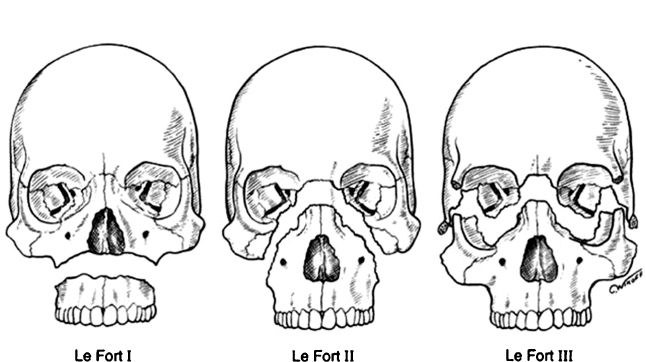
2. *Le Fort classification (Fig. 28-4)
a. Alternating thick buttresses and thinner segments create distinct fracture patterns
b. Usually involve pterygoid plates
c. Le Fort I: Transverse
i. Fracture at the level of tooth apices above the palate and alveolus
ii. Separates tooth-bearing maxilla from midface
iii. Extends from pyriform aperture posteriorly through nasal septum, anterior maxillary wall, lateral nasal wall, and pterygoid plates
d. Le Fort II: Pyramidal
i. Fracture crosses nasal bones along zygomaticomaxillary suture
ii. May involve frontal sinus
iii. Upper jaw and nasal bones mobile as single unit
e. Le Fort III: Craniofacial disjunction
i. May be minimally displaced with subtle occlusion problems
ii. Entire midface is mobile and detached from cranial base
iii. Fracture though pterygoid plates at a high level
iv. Simultaneous mobility of maxilla and nasofrontal and zygomaticofrontal regions
3. Vertical or sagittal fractures
a. Fracture sections maxilla in AP plane
b. Split palate, less common than Le Fort
Figure 28-3. Vertical and transverse buttresses of the facial skeleton. (From Mulholland MW, ed. Greenfield’s Surgery. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2011.)
Figure 28-4. Le Fort fracture patterns. (From Tasman W, Jaeger EA. Duane’s Ophthalmology. 2006 ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
4. Initial management
a. ABCs: Midfacial fractures are associated with high impact injury and concomitant C-spine fracture (10%)
b. IMF reduces fracture and decreases bleeding
5. Treatment
a. Alveolar fractures: Apply arch bars, place segment in occlusion, place IMF wires, 2-0 plates to stabilize fracture
b. Le Fort fractures: Primary bone grafts and rigid fixation
i. IMF 4 to 6 weeks
ii. Ensure proper reduction of nasomaxillary and zygomaxillary buttresses
c. Surgical steps
i. MMF to reestablish proper occlusal relations. This will usually establish the known starting point, mandible to crania base (may be difficult in the presence of split palate, alveolar, or mandible fx).
ii. Expose widely. May require multiple incisions—coronal, upper buccal sulcus, transconj, depending on the location of fractures.
iii. Reduce each segment anatomically starting from mandible → maxilla → zygoma → NOE, etc.
iv. Stabilize with mini-plates. Le Fort II must stabilize nasofrontal jx and infraorbital rims; Le Fort III must stabilize zygomaticofrontal suture.
v. Primary bone grafting utilized in the acute setting. Bridge gaps >0.5 cm of maxillary buttresses, >1.5 cm of antral wall.
vi. Soft tissue suspension of check to infraorbital rim
vii. Immobilization in MMF is not necessary for the healing of Le Fort fx if rigid fixation is utilized in the fx repair
viii. For Le Fort fx without mobility (<10%), place in MMF with elastics. If occlusion is not restored in 3 days do ORIF, otherwise keep in MMF for 6 weeks with soft diet.
ix. If the patient is allowed to return to early fx, soft foods only as true rigid fixation in the midface is not completely attained due to the thin bones and corresponding thin plates and screws
x. If the mandible is fractured at the condyle—cannot rely on mandible to establish proper facial height. ORIF midface first and star with the zygoma then place the patient in MMF and treat the mandible as indicated
xi. If the palate is fractured it may be helpful to first wire the posterior aspect of the palate for stability before MMF or any midfacial plating is undertaken
xii. Most common complication of Le Fort is reduced facial height and projection
f. Common inadequate fixation sequelae: Enophthalmos, malocclusion, increased facial width, soft-tissue descent, facial diastasis, and fat atrophy
g. Complications: Hemorrhage, airway compromise, pneumocephalus, open bite, nonunion, and malunion
H. Temporal bone trauma
1. Clinical signs
a. Facial palsy
b. Bruising over mastoid (Battle)
c. Hemotympanum
I. Palate fractures
1. Indications for surgery
a. Anterior–posterior-oriented fractures with large individual segments and no comminution
b. Palatal splints are used for complex fractures to provide the best vault stabilization
2. Surgical approach
a. Avoid devascularizing the buccal, gingival, or palatal mucosa during fracture exposure
b. Full open reduction must include reduction and stabilization of the palatal vault, dental arch (alveolus and pyriform aperture), and the four anterior vertical buttresses of the maxilla
c. Place the patient in MMF for 2 to 6 weeks
d. Splints only to supplement fixation
QUESTIONS YOU WILL BE ASKED
1. The bones comprising the orbit
Maxilla, zygoma, sphenoid, palatine, ethmoid, lacrimal, and frontal (see Fig. 28-2).
2. Facial nerve branches
(“two zebras bit my cat”) temporal, zygomatic, buccal, marginal mandibular, and cervical.
3. Patterns of Le Fort fractures
See Figure 28-4. Le Fort I is horizontal maxillary fracture. Le Fort II is pyramidal maxillary fracture. Le Fort III is craniofacial disjunction. All involve pterygoid plates.
The zygoma has a quadrilateral shape. It articulates with maxilla, frontal, sphenoid, and temporal bones.
5. The facial buttresses and their importance
See Figure 28-3. Four transverse and four vertical paired structural units of thicker bone lend strength and stability and project the soft-tissue envelope of face.
6. How to diagnose a CSF leak?
Send fluid for β-transferrin.
Recommended Readings
Fraioli RE, Branstetter BF 4th, Deleyiannis FW. Facial fractures: beyond Le Fort. Otolaryngol Clin North Am. 2008;41(1):51-76, vi. PMID: 18261526.
Haug RH, Buchbinder D. Incisions for access to craniomaxillofacial fractures. Atlas Oral Maxillofac Surg Clin North Am. 1993;1(2):1-29. PMID: 8118664.
Sargent LA. Nasoethmoid orbital fractures: diagnosis and treatment. Plast Reconstr Surg. 2007;120(7 Suppl 2):16S-31S. PMID: 18090726.
Sharabi SE, Koshy JC, Thornton JF, Hollier LH Jr. Facial fractures. Plast Reconstr Surg. 2011;127(2):25e-34e. PMID: 21285753.
Yavuzer R, Sari A, Kelly CP, et al. Management of frontal sinus fractures. Plast Reconstr Surg. 2005;115(6):79e-93e; discussion 94e-95e. PMID: 15861045.
< div class='tao-gold-member'>