Reconstruction of severe facial deformities poses a unique surgical challenge: restoring the aesthetic form and function of the face. Facial transplantation has emerged over the last decade as an option for reconstruction of these defects in carefully selected patients. As the world experience with facial transplantation grows, debate remains regarding whether such a highly technical, resource-intensive procedure is warranted, all to improve quality of life but not necessarily prolong it. This article reviews the current state of facial transplantation with focus on the current controversies and challenges, with particular attention to issues of technique, immunology, and ethics.
Key points
- •
Computed tomography angiography is helpful preoperatively for assessment of recipient vessel targets to plan for typically 2 arterial and 2 venous anastomoses to support the transplant.
- •
Skin is highly antigenic; acute rejection of facial transplants is common, if not universal, but chronic rejection is rare.
- •
Typical 3 drug immunosuppression exposes patients to risks of infection and development of malignancies, both of which can be deadly.
- •
Careful patient selection, thoughtful informed consent, and consideration of the psychosocial impact of facial transplant are necessary to keep the procedure ethically sound.
Introduction
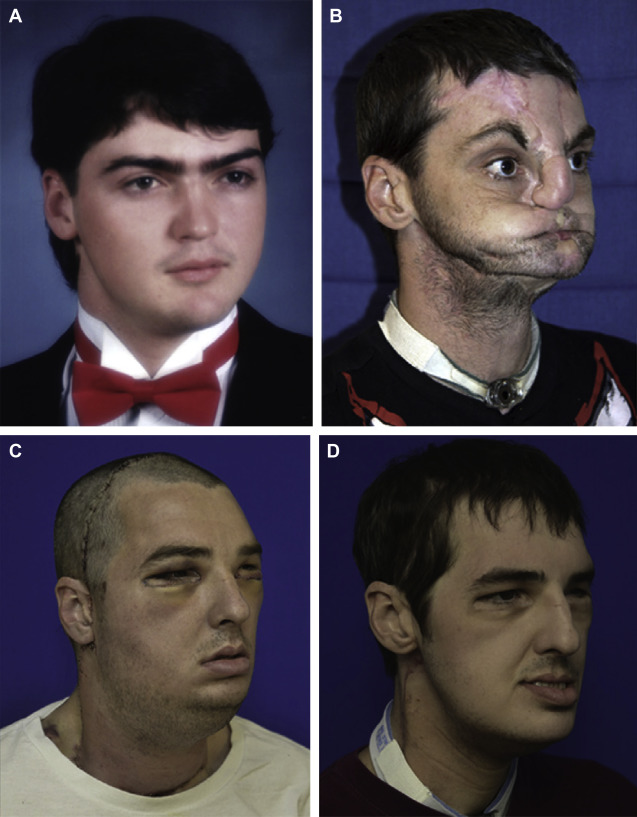
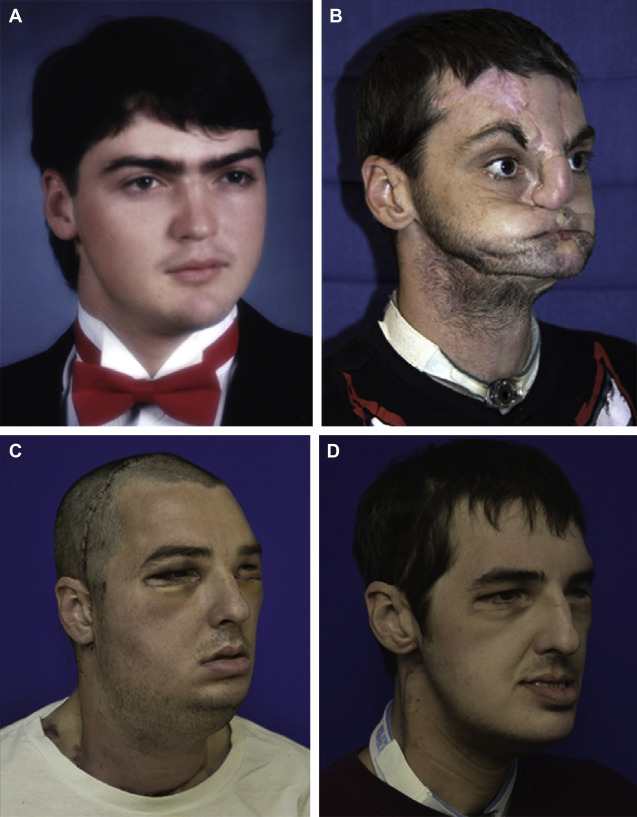
Conventional approaches to facial reconstruction are largely dictated by the extent of the defect. Although smaller defects may be amenable to local flaps, more extensive defects often require free tissue transfer or large split-thickness skin grafts. These techniques may suffice to provide coverage and occasionally restore function. However, in terms of both cosmesis and functionality, traditional reconstruction options fall short for patients with the most severe whole face deformities, often resulting in a patchwork appearance that reflects the sometimes dozens of surgeries these patients endure in pursuit of the elusive goal of achieving an acceptable appearance and quality of life ( Fig. 1 ).
Over the last 10 years, facial transplantation, a form of composite tissue allotransplantation (CTA), has emerged as a viable option for reconstruction of the most severe facial deformities in carefully selected patients. There have been 31 cases of facial transplantation reported in the world literature since the first case in 2005, with good results overall ( Table 1 ). However, facial transplantation was controversial at its inception; despite growing experience with this procedure, significant controversies persist.
| Number | Month/Year | City & Team Leader | R Sex, Age (y) | D Age (y) | Indication | Type | SD (h) |
|---|---|---|---|---|---|---|---|
| 1 | 11/2005 | Devauchelle, Amiens, France | F, 38 | 46 | Animal attack | Partial myocutaneous | 15 |
| 2 | 04/2006 | Guo, Xian, China | M, 30 a | 25 | Animal attack | Partial osteomyocutaneous | 13 |
| 3 | 01/2007 | Lantieri, Paris, France | M, 29 | 65 | NF 1 | Partial myocutaneous | 11 |
| 4 | 12/2008 | Siemionow, Cleveland, United States | F, 45 | 44 | Gunshot injury | Partial osteomyocutaneous | 22 |
| 5 | 03/2009 | Lantieri, Paris, France | M, 27 | 43 | Gunshot injury | Partial osteomyocutaneous | 19 |
| 6 | 04/2009 | Lantieri, Paris, France | M, 37 a | 59 | Burns | Partial myocutaneous | 13 |
| 7 | 04/2009 | Pomahac, Boston, United States | M, 59 | 60 | Burns | Partial osteomyocutaneous | 17 |
| 8 | 08/2009 | Lantieri, Paris, France | M, 33 | 55 | Gunshot injury | Partial osteomyocutaneous | 16 |
| 9 | 08/2009 | Cavadas, Valencia, Spain | M, 42 a | 35 | Radiotherapy | Partial osteomyocutaneous | 15 |
| 10 | 11/2009 | Devauchelle, Amiens, France | M, 27 | — | Burns | Partial osteomyocutaneous | 19 |
| 11 | 01/2010 | Gomez-Cia, Seville, Spain | M, 35 | 30 | NF 1 | Partial myocutaneous | 22 |
| 12 | 04/2010 | Barret, Barcelona, Spain | M, 31 | 41 | Gunshot injury | Full osteomyocutaneous | — |
| 13 | 07/2010 | Lantieri, Paris, France | M, 37 | — | NF 1 | Full myocutaneous | 14 |
| 14 | 03/2011 | Pomahac, Boston, United States | M, 25 | 48 | Burns | Full myocutaneous | 17 |
| 15 | 04/2011 | Lantieri, Paris, France | M, 45 | — | Gunshot injury | Partial osteomyocutaneous | — |
| 16 | 04/2011 | Lantieri, Paris, France | M, 41 | — | Gunshot injury | Partial osteomyocutaneous | — |
| 17 | 04/2011 | Pomahac Boston, United States | M, 30 | 31 | Burns | Full myocutaneous | 14 |
| 18 | 05/2011 | Pomahac, Boston, United States | F, 57 | 42 | Animal attack | Full osteomyocutaneous | 19 |
| 19 | 01/2012 | Özkan, Antalya, Turkey | M, 19 | 39 | Burns | Full osteomyocutaneous | 9 |
| 20 | 01/2012 | Blondeel, Gent, Belgium | N/A | N/A | N/A | Partial osteomyocutaneous | 20 |
| 21 | 02/2012 | Nazir, Ankara, Turkey | M, 25 | 40 | Burns | Full face transplant | — |
| 22 | 03/2012 | Özmen, Ankara, Turkey | F, 20 | 28 | Burns | Partial face transplant | — |
| 23 | 03/2012 | Rodriguez, Baltimore, United States | M, 37 | 21 | Gunshot injury | Full osteomyocutaneous | 36 |
| 24 | 05/2012 | Özkan, Antalya, Turkey | M, 27 | 19 | Burns | Full face transplant | — |
| 25 | 01/2013 | Pomahac, Boston, United States | F, 44 | — | Burns | Full myocutaneous | 15 |
| 26 | 05/2013 | Özkan, Antalya, Turkey | M 27 | 19 | Gunshot injury | Partial osteomyocutaneous | — |
| 27 | 07/2013 | Maciejewski, Warsaw, Poland | M, 33 | 42 | Crush trauma | Partial osteomyocutaneous | 27 |
| 28 | 07/2013 | Özkan, Antalya, Turkey | M, 27 | — | Ballistic trauma | Full osteomyocutaneous | — |
| 29 | 08/2013 | Özkan, Antalya, Turkey | M, 54 a | — | Ballistic trauma | Partial osteomyocutaneous | — |
| 30 | 12/2013 | Özkan, Antalya, Turkey | M, 22 | — | Ballistic trauma | Partial osteomyocutaneous | — |
| 31 | 12/2013 | Maciejewski, Warsaw, Poland | F, 26 | — | Neurofibromatosis | Full myocutaneous | — |
In this article, the authors focus on the current controversies, challenges, and questions that confront facial transplantation while highlighting the lessons learned and challenges overcome through experience thus far. The discussion focuses on 3 main topics: technical issues, issues of facial transplantation immunology, and ethical concerns.
Introduction
Conventional approaches to facial reconstruction are largely dictated by the extent of the defect. Although smaller defects may be amenable to local flaps, more extensive defects often require free tissue transfer or large split-thickness skin grafts. These techniques may suffice to provide coverage and occasionally restore function. However, in terms of both cosmesis and functionality, traditional reconstruction options fall short for patients with the most severe whole face deformities, often resulting in a patchwork appearance that reflects the sometimes dozens of surgeries these patients endure in pursuit of the elusive goal of achieving an acceptable appearance and quality of life ( Fig. 1 ).
Over the last 10 years, facial transplantation, a form of composite tissue allotransplantation (CTA), has emerged as a viable option for reconstruction of the most severe facial deformities in carefully selected patients. There have been 31 cases of facial transplantation reported in the world literature since the first case in 2005, with good results overall ( Table 1 ). However, facial transplantation was controversial at its inception; despite growing experience with this procedure, significant controversies persist.
| Number | Month/Year | City & Team Leader | R Sex, Age (y) | D Age (y) | Indication | Type | SD (h) |
|---|---|---|---|---|---|---|---|
| 1 | 11/2005 | Devauchelle, Amiens, France | F, 38 | 46 | Animal attack | Partial myocutaneous | 15 |
| 2 | 04/2006 | Guo, Xian, China | M, 30 a | 25 | Animal attack | Partial osteomyocutaneous | 13 |
| 3 | 01/2007 | Lantieri, Paris, France | M, 29 | 65 | NF 1 | Partial myocutaneous | 11 |
| 4 | 12/2008 | Siemionow, Cleveland, United States | F, 45 | 44 | Gunshot injury | Partial osteomyocutaneous | 22 |
| 5 | 03/2009 | Lantieri, Paris, France | M, 27 | 43 | Gunshot injury | Partial osteomyocutaneous | 19 |
| 6 | 04/2009 | Lantieri, Paris, France | M, 37 a | 59 | Burns | Partial myocutaneous | 13 |
| 7 | 04/2009 | Pomahac, Boston, United States | M, 59 | 60 | Burns | Partial osteomyocutaneous | 17 |
| 8 | 08/2009 | Lantieri, Paris, France | M, 33 | 55 | Gunshot injury | Partial osteomyocutaneous | 16 |
| 9 | 08/2009 | Cavadas, Valencia, Spain | M, 42 a | 35 | Radiotherapy | Partial osteomyocutaneous | 15 |
| 10 | 11/2009 | Devauchelle, Amiens, France | M, 27 | — | Burns | Partial osteomyocutaneous | 19 |
| 11 | 01/2010 | Gomez-Cia, Seville, Spain | M, 35 | 30 | NF 1 | Partial myocutaneous | 22 |
| 12 | 04/2010 | Barret, Barcelona, Spain | M, 31 | 41 | Gunshot injury | Full osteomyocutaneous | — |
| 13 | 07/2010 | Lantieri, Paris, France | M, 37 | — | NF 1 | Full myocutaneous | 14 |
| 14 | 03/2011 | Pomahac, Boston, United States | M, 25 | 48 | Burns | Full myocutaneous | 17 |
| 15 | 04/2011 | Lantieri, Paris, France | M, 45 | — | Gunshot injury | Partial osteomyocutaneous | — |
| 16 | 04/2011 | Lantieri, Paris, France | M, 41 | — | Gunshot injury | Partial osteomyocutaneous | — |
| 17 | 04/2011 | Pomahac Boston, United States | M, 30 | 31 | Burns | Full myocutaneous | 14 |
| 18 | 05/2011 | Pomahac, Boston, United States | F, 57 | 42 | Animal attack | Full osteomyocutaneous | 19 |
| 19 | 01/2012 | Özkan, Antalya, Turkey | M, 19 | 39 | Burns | Full osteomyocutaneous | 9 |
| 20 | 01/2012 | Blondeel, Gent, Belgium | N/A | N/A | N/A | Partial osteomyocutaneous | 20 |
| 21 | 02/2012 | Nazir, Ankara, Turkey | M, 25 | 40 | Burns | Full face transplant | — |
| 22 | 03/2012 | Özmen, Ankara, Turkey | F, 20 | 28 | Burns | Partial face transplant | — |
| 23 | 03/2012 | Rodriguez, Baltimore, United States | M, 37 | 21 | Gunshot injury | Full osteomyocutaneous | 36 |
| 24 | 05/2012 | Özkan, Antalya, Turkey | M, 27 | 19 | Burns | Full face transplant | — |
| 25 | 01/2013 | Pomahac, Boston, United States | F, 44 | — | Burns | Full myocutaneous | 15 |
| 26 | 05/2013 | Özkan, Antalya, Turkey | M 27 | 19 | Gunshot injury | Partial osteomyocutaneous | — |
| 27 | 07/2013 | Maciejewski, Warsaw, Poland | M, 33 | 42 | Crush trauma | Partial osteomyocutaneous | 27 |
| 28 | 07/2013 | Özkan, Antalya, Turkey | M, 27 | — | Ballistic trauma | Full osteomyocutaneous | — |
| 29 | 08/2013 | Özkan, Antalya, Turkey | M, 54 a | — | Ballistic trauma | Partial osteomyocutaneous | — |
| 30 | 12/2013 | Özkan, Antalya, Turkey | M, 22 | — | Ballistic trauma | Partial osteomyocutaneous | — |
| 31 | 12/2013 | Maciejewski, Warsaw, Poland | F, 26 | — | Neurofibromatosis | Full myocutaneous | — |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







