Facial Skeletal Augmentation with Implants
Michael J. Yaremchuk
Chad R. Gordon
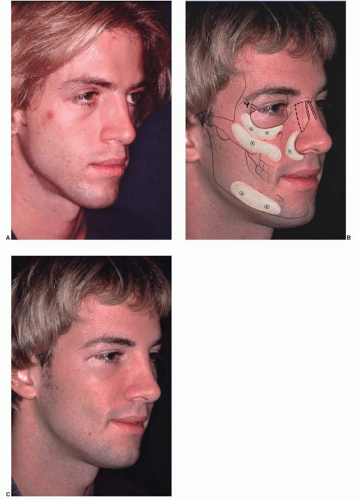
The morphology of the facial skeleton is a fundamental determinant of facial appearance. Facial skeletal augmentation is usually accomplished with alloplastic materials. Implants can be used to restore or create contour during reconstruction of congenital, posttraumatic, or postablative deformities. They are useful adjuncts and, sometimes, alternatives to orthognathic surgery in patients with corrected or normal occlusion, respectively. Most often, facial skeletal augmentation is performed electively to improve facial aesthetics (Figure 50.1).
PREOPERATIVE PLANNING
Physical examination is the most important element in preoperative assessment and planning. Reviewing life-size frontal and lateral photographs with the patient is useful when discussing aesthetic concerns and goals. Although cephalometric radiograph analysis can be helpful in the planning, the size and position of the implants are largely aesthetic judgments. Computerized tomographic (CT) data with subsequent physical model reconstruction can be particularly useful in planning the procedure or designing and fabricating implants specific for an individual patient.
Although often referenced in texts discussing facial skeletal augmentation, neoclassical canons describing ideal facial proportions have a limited role in surgical evaluation and planning because they are arbitrary. When the facial dimensions of normals and those deemed more attractive than normal were compared with artistic ideals, it was found that some theoretic proportions are never found, and others are one of the many variations.1,2 For these reasons, we have found it more useful to use the anthropometric measurements of normals to guide our gestalt for the selection of implants for facial skeletal augmentation.
In planning facial skeletal augmentation, it is important to realize that small increases in skeletal projection have a powerful impact on facial appearance. It is emphasized to the patient during the preoperative consultation that all faces are asymmetric. If unrecognized preoperatively, an asymmetric postoperative result usually may be interpreted by the patient as a technical error by the surgeon.
IMPLANTS
Materials
Virtually all aesthetic facial skeletal augmentation is achieved with alloplastic implants. The use of synthetic materials avoids donor site morbidity and vastly simplifies the procedure in terms of time and complexity. Implant materials used for facial skeletal augmentation are biocompatible, that is, they have an acceptable interaction between the material and the host. Because the host has little or no enzymatic ability to degrade the implant material, the implant tends to maintain its volume and shape. Likewise, the implant has a minimal and predictable effect on the host tissue that surrounds it. This type of relationship is an advantage over the use of autogenous bone which, when revascularized, will be remodeled to varying degrees, thereby changing volume and shape.3
The presently used alloplastic implants used for facial reconstruction do not have a toxic effect on the host.4 The host responds to these materials by forming a fibrous capsule around the implant, thereby isolating the implant. The surface of the implant determines the nature of the capsule. Smooth implants result in the formation of smooth-walled capsules. Porous implants allow varying degrees of soft-tissue ingrowth, which results in a less-dense and less-defined capsule. Clinical experience has shown that porous implants have fewer tendencies to erode underlying bone and fewer tendencies to migrate as a result of overlying soft-tissue mechanical forces. These attributes are presumably due to the fibrous incorporation associated with porous implants as opposed to the fibrous encapsulation typical of smooth implants.
The most commonly used and commercially available materials today for facial skeletal augmentation are solid silicone, polytetrafluoroethylene, and porous polyethylene. The silicone rubber used for facial implants is a vulcanized form of polysiloxane, which is a polymer created from interlocking silicone and oxygen with methyl side groups. Silicone is derived from silicon, a semimetallic element that in nature combines with oxygen to form silicon dioxide, or silicone. Beach sand, crystals, and quartz are silica. The advantages of solid silicone are that it is easily sterilizable by steam or irradiation, it can be carved easily with either a scissor or scalpel, and it can be stabilized with a screw or a suture. There are no known clinical or allergic reactions. Because it is smooth, it can be removed quite easily. The disadvantages of silicone implants include their tendency to cause resorption of the bone underlying it, the potential to migrate if not fixed, and the likelihood for the implant and its fibrous capsule to be visible when placed under a thin soft-tissue cover.
Polytetrafluoroethylene.
Polytetrafluoroethylene has a carbon-ethylene backbone to which are attached four fluorine molecules. It is chemically stable, has a nonadherent surface, and, because it is not cross-linked, is flexible. Extensive experience has been accumulated with polytetrafluoroethylene (Gore-Tex; WL Gore, Flagstaff, AZ) for vascular prostheses, soft-tissue patches, and sutures. A variety of preformed implants are available for both subdermal and subperiosteal placement. Preformed implants are made with a pore size between 10 and 30 µm. The porosity allows for some soft-tissue ingrowth, for less fibrous encapsulation, and for less tendency to migrate as compared with smooth-surfaced implants. It is easily sterilizable, smooth enough to be maneuvered easily through soft tissues, and can be fixed to underlying structures with sutures or screws.
Polyethylene.
Polyethylene is a simple carbon chain of ethylene monomer. The high-density variety—Medpor (Porex, Newnan, GA) and SynPOR (Synthes, West Chester, PA)—is used for facial implants because of its high tensile strength. Although chemically similar to polytetrafluoroethylene, polyethylene has a much firmer consistency that resists material compression yet permits some flexibility. Its intramaterial porosity between 125 and 250 µm allows more extensive fibrous ingrowth as compared with polytetrafluoroethylene. Soft-tissue ingrowth lessens the implant’s tendency to migrate and to erode underlying bone. Its firm consistency allows it to be easily fixed with screws and to be contoured with a scalpel or power equipment without fragmenting. A disadvantage of its greater porosity is that it allows soft tissues to adhere to it, making placement more difficult and requiring a larger
pocket than is required for smoother implants. Soft-tissue ingrowth into the larger pores also makes implant removal more difficult.
pocket than is required for smoother implants. Soft-tissue ingrowth into the larger pores also makes implant removal more difficult.
Requisites of Implant Shape, Positioning, and Immobilization
Shape.
The superficial surface of the implant determines the new skeletal morphology. Its posterior surface should mold to the bone to which it is applied. Gaps between the bone and the implant result in unpredictable increases in augmentation. The implant margins must taper imperceptibly into the native skeleton so that they are neither visible nor palpable.
Positioning.
Although some surgeons prefer to place implants in a soft-tissue pocket (supraperiosteal), clinical experience has led to a strict policy of subperiosteal placement. A subperiosteal pocket involves a dissection that is safe to nerves and is relatively bloodless. It allows optimal visualization of the skeleton and therefore the opportunity for precise augmentation.
The size of the pockets is determined by the type of implant used and its method of immobilization. The long-standing teaching when using smooth silicone implants is to make a pocket just large enough to accommodate the implant so as to guarantee its position. Porous implants require a larger pocket because they adhere to the soft tissue during their placement. When using smooth or porous implants, I dissect widely enough to have a perspective of the skeletal anatomy being augmented, which allows precise and symmetric implant positioning.
Immobilization.
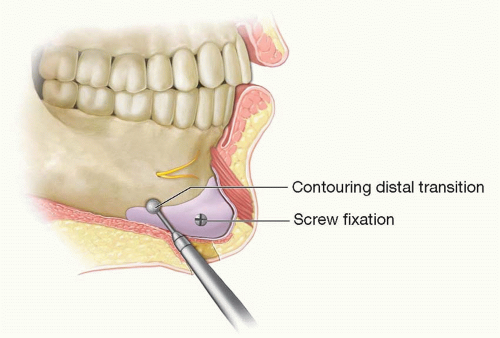
Many surgeons stabilize the position of the implant by suturing it to surrounding soft tissues or by using temporary transcutaneous pullout sutures. Screw fixation of the implant to the skeleton has several benefits. It prevents movement of the implant. Because each facial skeleton has a unique and varying surface topography, portions of an implant may not conform to the bone, leaving gaps between the implant and the skeleton. This results in unpredicted increases in augmentation and distortions of the desired facial shape. Screw fixation assures application of the implant to the bone. Screw fixation also allows for final contouring of the implant in position. This final contouring is particularly important where the edge of the implant interfaces with the skeleton (Figure 50.2). Step-offs between the implant and the skeleton may be palpable and visible.
ANESTHESIA
Facial skeletal augmentation can be performed under local or general anesthesia and is routinely performed on an outpatient basis. I prefer to perform most facial skeletal surgery under general endotracheal anesthesia because most facial implants are placed either in the malar midface or along the mandible, which requires a combination of intraoral incisions. Endotracheal intubation assures protection of the airway and the optimal antiseptic preparation of the oral cavity. Patient positioning and exposure for implant placement are also optimized when the airway is controlled. The surgical site is infiltrated with a solution containing Marcaine for postoperative pain control and epinephrine to minimize bleeding.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree