I. FACIAL NERVE ANATOMY AND FUNCTION
A. The facial nerve, or cranial nerve VII, has separate motor and sensory divisions
1. Motor division
a. Originates from the facial motor nucleus within the pons
b. Dorsal neurons of the facial motor nucleus receive bilateral cortical input, while ventral neurons receive contralateral cortical input only
i. An upper motor neuron lesion manifests as contralateral lower facial paralysis (i.e., the contralateral forehead is spared due to its own ipsilateral cortical input)
ii. A lower motor neuron lesion manifests as ipsilateral total facial paralysis
2. Sensory division
a. Also referred to as the nervus intermedius
b. Originates from the geniculate ganglion at the junction of the labyrinthine and tympanic segments of the facial canal
c. Preganglionic parasympathetic secretomotor fibers originate from the superior salivatory nucleus within the pons
3. Intratemporal course
a. The motor and sensory divisions enter the facial canal at the internal acoustic meatus and join together as a common trunk at the geniculate ganglion prior to exiting the stylomastoid foramen
b. Can be divided into three segments: labyrinthine (proximal), tympanic, and mastoid (distal)
4. Extratemporal course
a. From the stylomastoid foramen to the muscles of facial expression
b. *Three anatomic landmarks are commonly used to identify the main trunk of the facial nerve as it exits the stylomastoid foramen
i. Tragal pointer: The nerve is located 1 cm inferior and 1 cm deep to the tragal cartilage
ii. Tympanomastoid suture: The nerve is located 6 to 8 mm medial to the end of the suture line
iii. Posterior belly of the digastric muscle: The nerve runs at the same depth as this muscle and is found halfway between this muscle and the styloid process
iv. The styloid process itself is not a useful anatomic landmark because it is located deep to the nerve, resulting in a higher incidence of nerve injury during its dissection
v. A small branch off the occipital artery is often encountered just lateral to the nerve; thus, brisk bleeding is usually an indicator that the nerve is nearby
vi. Be careful in children—these anatomic landmarks can be distorted, and the nerve runs more superficial
c. The facial nerve gives off the posterior auricular nerve, stylohyoid branch, and digastric branch prior to entering the parotid gland
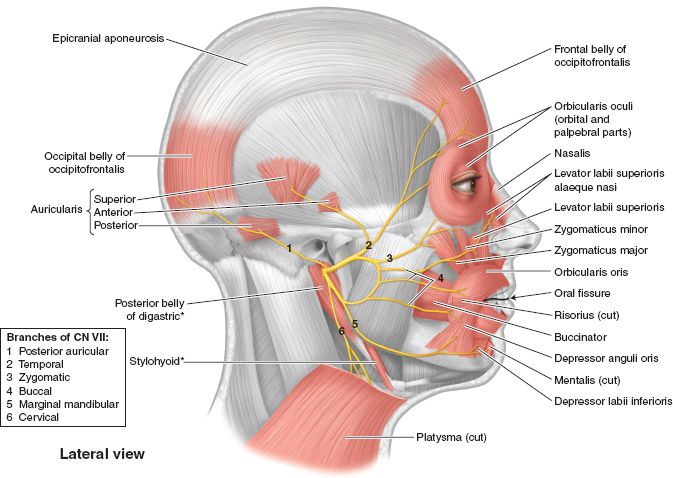
d. Within the parotid gland, it lies between the superficial and deep lobes, and separates into the temporofacial (upper) and cervicofacial (lower) divisions at the pes anserinus (Fig. 24-1)
______________
*Denotes common in-service examination topics
Figure 24-1. Facial nerve anatomy and facial musculature. (From Moore KL, Dalley AF, Agur AM, eds. Clinically Oriented Anatomy. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010.)
i. Temporofacial (upper) division: Terminates as the temporal, zygomatic, and buccal branches
ii. Cervicofacial (lower) division: Terminates as the buccal, marginal mandibular, and cervical branches
e. Temporal branch
i. *Lies just superficial to the superficial layer of the deep temporal fascia (i.e., deep to superficial temporal (tempo-parietal) fascia which is continuous with SMAS).
ii. *Follows the course of a line drawn from 0.5 cm below the tragus to 1.5 cm above the lateral brow
iii. Crosses the zygomatic arch over its middle third
iv. Especially prone to injury due to its location and lack of redundancy (i.e., it does not arborize)
f. Buccal branch
i. Lies deep to the SMAS where it arborizes and forms extensive interconnections
ii. *Most common facial nerve injury during rhytidectomy, but rarely symptomatic due to its redundancy
g. Marginal mandibular branch
i. Lies deep to the platysma muscle
ii. *Before crossing over the facial vessels, it runs along the inferior border of the mandible (80%) or 1 to 2 cm below it (20%)
iii. After crossing the facial vessels, it remains above the inferior border of the mandible
iv. Similar to the temporal branch, it is especially prone to injury due to its lack of redundancy
B. The facial nerve contains five types of nerve fibers
1. General visceral efferents (GVEs)
a. Provide preganglionic parasympathetic secretomotor function as part of the autonomic nervous system
b. Chorda tympani nerve: Sublingual and submandibular glands
c. Greater superficial petrosal nerve: Lacrimal, nasal, and palatine glands
2. Special visceral efferents (SVEs)
a. Voluntary motor control of muscles derived from the second branchial (hyoid) arch
b. Nerve to stapedius: Stapedius muscle
c. Posterior auricular nerve: Intrinsic ear muscles and the posterior auricular muscle (auricular branch), and the occipitalis muscle (occipital branch)
d. Terminal branches: Stylohyoid muscle, posterior belly of the digastric muscle, and the muscles of facial expression
3. General somatic afferents (GSAs)
a. Transmit feelings of pain, light touch, and temperature
b. Posterior auricular nerve: External auditory canal
4. General visceral afferents (GVAs)
a. Transmit feelings of pain from the visceral structures as part of the autonomic nervous system
c. Greater superficial petrosal nerve: Soft palate
5. Special visceral afferents (SVAs)
a. Transmit the special sense of taste, or gustation
b. Chorda tympani nerve: Anterior two-thirds of the tongue
c. Greater superficial petrosal nerve: Soft palate
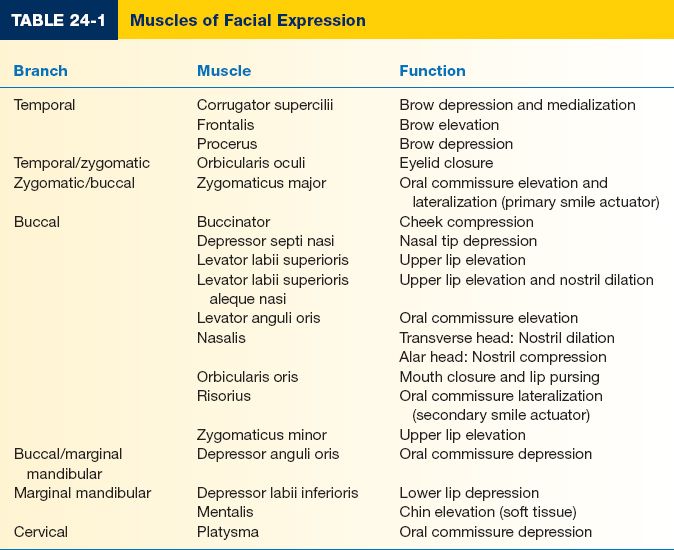
C. Muscles of facial expression (Fig. 24-1 and Table 24-1)
1. Four layers of facial musculature (from superficial to deep)
a. Depressor anguli oris, zygomaticus minor, orbicularis oculi
b. Depressor labii inferioris, risorius, platysma, zygomaticus major, levator labii superioris alaeque nasi
c. Orbicularis oris, levator labii superioris
d. Mentalis, levator anguli oris, buccinator
2. The muscles of facial expression can be viewed as a series of constrictors or expanders of the ocular, nasal, and oral sphincters
3. *All muscles are innervated on their deep surface, except for the buccinator, levator anguli oris, and mentalis (i.e., these muscles are inner-vated on their superficial surface)
4. Muscle movements on examination
a. Raises eyebrows: Frontalis
b. Closes eyelids: Orbicularis oculi
c. Smile: Zygomaticus major and minor
d. Purse lips: Orbicularis oris
II. ETIOLOGY OF FACIAL PARALYSIS
A. Facial paralysis can result from an anatomic lesion anywhere along the length of the facial nerve including proximal to, within, or distal to the temporal bone
1. Proximal to the temporal bone (intracranial): Compressive masses tend to have an insidious onset, while acute vascular obstruction accounts for most cases of sudden-onset facial paralysis
a. Neoplastic: Meningioma, cerebellopontine tumors, and bilateral acoustic neuromas in the setting of neurofibromatosis type 2
b. Traumatic: Penetrating trauma and shear injury
c. Infectious: Encephalitis, meningitis, and intracerebral abscess
d. Vascular: Aneurysm, cerebrovascular accident, vasculitis, and intracerebral hemorrhage
e. Neurodegenerative: Amyotrophic lateral sclerosis and multiple sclerosis
f. Iatrogenic: Tumor extirpation
g. Congenital: Möbius syndrome and Goldenhar syndrome
i. *Bilateral underdevelopment of the facial and abducens nerves, usually accompanied by congenital absence of the facial motor nucleus
ii. *Patients typically present with a motionless face and inability to abduct the eyes
iii. Other anomalies include club foot (most common) and features of Poland’s syndrome
2. Within the temporal bone (intratemporal)
a. Neoplastic: Cholesteatoma
b. Traumatic: Penetrating trauma and temporal bone fracture
i. Classified as either longitudinal (80%) or transverse (20%)
ii. Facial paralysis is more common with the transverse type
iii. Symptoms are usually due to swelling and compression of the nerve within the facial canal
c. Infectious: Acute otitis media/externa, mastoiditis, and Ramsay–Hunt syndrome—“herpes zoster oticus”
i. Characterized by unilateral facial paralysis, otalgia, and a painful vesicular rash in the external auditory canal
ii. Oral corticosteroids and antivirals for 10 days may be helpful, if started within 72 hours of symptom onset
d. Iatrogenic: Tumor extirpation
e. Systemic: Pregnancy, diabetes mellitus, neurosarcoidosis, hyperthyroidism, amyloidosis, and Melkersson–Rosenthal syndrome—“cheilitis granulomatosa”
i. Characterized by recurrent granulomatous inflammation of the lips, facial paralysis, and plicated tongue
ii. Often associated with Crohn disease
f. Toxins: Lead poisoning and carbon monoxide
g. Idiopathic: Bell’s palsy
i. *Most common cause of unilateral facial paralysis in adults
ii. A diagnosis of exclusion thought to involve a viral-induced inflammatory process leading to edema and compression of the nerve within the facial canal
iii. Higher incidence in pregnant and diabetic patients
iv. Rapid onset is characteristic, often described as appearing overnight
v. Most patients (85%) experience spontaneous recovery within 3 weeks, and the remainder of patients within 6 months
vi. *Observation is recommended for 3 weeks prior to performing any imaging or electrodiagnostic studies
vii. Oral corticosteroids and antivirals are recommended within 72 hours of symptom onset
viii. Facial nerve decompression is controversial
3. Distal to the temporal bone (extratemporal)
a. Neoplastic: Parotid tumors
b. Traumatic: Penetrating trauma
i. *The general “rule of thumb” is that facial nerve exploration is not warranted for lacerations medial to a vertical line dropped down from the lateral canthus
ii. *Exploration must be performed within 72 hours of injury (prior to neurotransmitter depletion) so that the distal end can be identified by electrical stimulation
c. Infectious: Parotitis
d. Iatrogenic: Tumor extirpation
e. Obstetrical: Forceps delivery
i. May also be related to pressure from the maternal sacrum
ii. Produces a neuropraxia that is managed nonoperatively
f. Congenital: Congenital unilateral lower lip paralysis (CULLP)
i. Not considered a true congenital facial paralysis
ii. Caused by hypoplasia or absence of the lower lip depressors
iii. Typically presents with deviation of the lower lip toward the unaffected side with emotion (e.g., crying)
B. Bilateral facial paralysis is not as common as unilateral facial paralysis, but frequent causes include Lyme disease (most common), Möbius syndrome, toxins, and any systemic condition including HIV infection.
III. DIAGNOSIS OF FACIAL PARALYSIS
A. Detailed history
1. Facial paralysis is a clinical diagnosis
a. Rate of disease progression: Gradual onset (e.g., neoplastic, neurodegenerative, systemic) versus rapid onset (e.g., traumatic, vascular, infectious, iatrogenic, idiopathic)
b. Duration of symptoms: Health of the affected mimetic musculature as a result of prolonged denervation—key factor in decision between a nerve operation or muscle operation.
c. The temporal relationship between symptom onset and the possible contributing factors (e.g., new medications, exposure to toxins, history of recent surgery or trauma, chronic illnesses, infection) helps narrow down the differential diagnosis list.
2. Use a “top-down” anatomic approach to document all of the patient’s complaints, so that each of them can be individually addressed
a. Eye
i. Does the patient complain of eye discomfort, changes in vision, dryness, or excessive tearing?
ii. Can the patient close his or her eye on the affected side? (caused by paralysis of orbicularis oculi)
iii. Does the patient require the use of artificial tears?
i. Does the patient have any difficulty breathing out of his or her nose? (caused by paralysis of Levator labii superioris aleque nasi and nasalis)
ii. Is it worse during inspiration or expiration?
c. Mouth
i. Does the patient complain of drooling?
ii. Does the patient have any difficulty speaking, especially when articulating bilabial plosives?
iii. Does the patient complain of a crooked smile?
B. Neuromuscular examination
1. Ask for a picture of the patient; routinely, subtle facial asymmetries exist prior to the diagnosis of facial paralysis
2. Classically, unilateral facial paralysis presents with symmetry at rest and asymmetry with spontaneous animation
a. Upper motor neuron lesion: Contralateral lower facial paralysis
b. Lower motor neuron lesion: Ipsilateral total facial paralysis
c. At rest
i. Smooth forehead with absence of wrinkles
ii. Brow ptosis with absence of true eyelid ptosis
iii. Paralytic ectropion with increased scleral show
iv. C-shaped nasal deformity with tip and phitral deviation toward the unaffected side.
v. Effacement and lack of definition of the nasolabial fold
vi. Drooping of the oral commissure
b. With spontaneous animation
i. Inability to elevate the brow (temporal branch)
ii. Lagophthalmos (zygomatic branch)
iii. Lack of nostril dilatation during inspiration (buccal branch)
iii. Inability to smile (zygomatic branch)
iv. Inability to whistle or puff out cheeks (buccal branch)
v. *Inability to expose lower dentition in a full-denture smile (either marginal mandibular or cervical branch—asymmetry on pursing lips is also present in marginal mandibular palsy, but absent in cervical palsy); additionally,the paralyzed side always corresponds to the lower lip that is more elevated (i.e., the lower lip depressors are paralyzed).
c. Other associated physical findings may also be present
i. Xerophthalmia (greater superficial petrosal nerve)
ii. Hyperacusis (nerve to stapedius)
iii. Dysgeusia (chorda tympani nerve)
5. Preoperative evaluation of eyelid and canalicular function (refer to Chapter 17, “Eyelid Reconstruction”)
6. Synkinesis represents “miswiring” of regenerating SVE fibers to different mimetic muscles than which they were intended
a. Produces synchronization of voluntary contraction between disparate muscle groups (e.g., eyelid closure with smile)
b. Crocodile tears refer to hyperlacrimation during chewing or salivation and are caused by “miswiring” of regenerating GVE fibers to the lacrimal gland instead of the salivary glands.
7. The House–Brackmann facial nerve grading system is the most common classification scheme—I (normal) to VI (complete facial paralysis)
a. Evaluates gross appearance and motion at the forehead, eye, and mouth
b. Limitations include its generalized assessment of facial nerve function, inability to detect small changes in facial nerve recovery, and it does not address synkinesis.
C. Electrodiagnostic studies
1. Assist with prognostication and the decision between operative intervention versus continued observation
a. The normal side of the face is required for comparison and interpretation of results (i.e., less useful in bilateral cases)
b. Must allow at least 72 hours after symptom onset for Wallerian degeneration to occur in the distal segment
2. Nerve excitability test (NET)
a. Transcutaneous stimulation over the stylomastoid foramen until contraction of the paralyzed side is visualized at the lowest current
b. Difference greater than 3.5 mA with the normal side is significant
c. Easy to perform, but highly subjective and examiner dependent
3. Maximal stimulation test (MST) is similar to the NET, except maximal current is used for comparison
4. Electroneurography (ENoG)
a. Compares amplitude of CMAPs between sides with greater than 90% axonal degeneration representing a poorer prognosis
b. Most predictive test for facial nerve recovery
5. Electromyography (EMG)
a. Performed 2 to 3 weeks after symptom onset—at rest, with needle insertion, and with voluntary muscle contraction
b. Fibrillation potentials: Muscle denervation
c. Polyphasic potentials: Muscle reinnervation
D. Other imaging modalities
1. An audiogram should be obtained in all patients, and if abnormal, then the next step is magnetic resonance imaging and referral to an otolaryngologist
2. In cases of trauma, computed tomography is helpful in ruling out temporal bone fractures
IV. NONSURGICAL MANAGEMENT OF THE PARALYZED FACE
A. Protection of the cornea
1. If dryness is not prevented, it can lead to ulceration and eventual blindness, especially if corneal sensation is impaired
a. Artificial tears can be helpful
b. Taping of the eyelid can provide some external support
c. Eye patches or moisture shields can reduce evaporative losses
d. Temporary tarsorrhaphy is required in refractory cases
2. Increased risk in patients with a poor Bell’s phenomenon
B. Botulinum toxin
1. Target-specific muscle groups on the normal side to achieve temporary facial balance while nerve regeneration occurs
2. Also used to treat synkinesis and blepharospasm
C. Oral corticosteroids and antivirals
1. Treats edema and compression of the nerve within the facial canal
2. Recommended within 72 hours of symptom onset
D. Physical therapy
1. Focuses on facial reeducation, especially if recovery is incomplete
2. Examples include EMG and mirror biofeedback
E. Although it does not treat the underlying cause, certain types of clothing and particular hairstyles can help mask or hide facial asymmetries
V. SURGICAL MANAGEMENT OF THE PARALYZED FACE
A. Patients are divided into two treatment groups based on duration of symptoms—are the facial muscles still usable?
1. Less than 18 to 24 months: Nerve operations
2. Greater than 18 to 24 months: Muscle operations
B. Nerve operations
1. Ipsilateral facial nerve available
a. Primary nerve repair if no nerve gap is present
b. Nerve grafting if nerve gap is present
c. Incidence of synkinesis is increased with nerve grafting due to the presence of two coaptations instead of one
d. If a hostile wound environment exists or concomitant injuries are prohibitive to surgery, then the nerve ends should be tagged for future exploration and repair.
2. Ipsilateral facial nerve not available
a. Cross-facial nerve grafting (CFNG)
i. A donor nerve graft (e.g., sural nerve) guides regenerating nerve fibers from a redundant facial nerve branch on the normal side to a distal nerve stump on the paralyzed side
ii. Provides greatest potential for spontaneous animation
iii. Nerve growth is monitored by an advancing Tinel’s sign
iv. Indicated when proximal ipsilateral nerve stump is unavailable for grafting and distal stump is present and the facial muscles are capable of function after reinnervation.
b. Nerve transfers
i. Powerful due to a greater number of nerve fibers being transferred compared to CFNG, but does not provide spontaneous animation
ii. Donor nerves: XII, XI, masseteric branch of V, ipsilateral C7 root, and phrenic nerve
iii. Complications: Hemiglossal dysfunction (XII), shoulder droop (XI), and hemidiaphragm paralysis (phrenic nerve)
c. Babysitter procedure
i. If the ipsilateral facial nerve is not available and denervation time is between 6 and 18 months, a CFNG can be combined with a minihypoglossal transfer
ii. XII “babysits” the facial muscles until the regenerating nerve fibers arrive from the CFNG
C. Muscle operations
1. Dynamic procedures restore facial movement
2. Static procedures achieve symmetry at rest
3. Upper face: Must address frontalis muscle
a. Supraciliary brow lift
i. Relieves brow ptosis by excising an ellipse of skin and frontalis muscle just above the eyebrow
ii. Alternatively, an endoscopic brow lift can be used
b. Botulinum toxin can temporarily reduce muscular tone in the contralateral normal forehead to match the paralyzed side
4. Midface: Must address orbicularis oculi muscle and the nostril dilators
a. Upper eyelid
i. Gold weight implantation or palpebral springs achieve lid closure by gravity assistance. Weight is placed just lateral of midline over the tarsus.
ii. In the supine position, the lids must be taped together
b. The lower eyelid is treated with lid-tightening procedures (refer to Chapter 19, “Eyelid Reconstruction”)
c. Nose
i. Nonanatomic alar contour grafts: Prevent external nasal valve collapse
ii. Spreader grafts: Prevent internal nasal valve collapse
d. Regional and free microneurovascular muscle transfers have been described to the midface, but the results are less effective compared to smile restoration
5. Lower face: Must address zygomaticus major and lower lip depressors
a. Smile restoration is the primary goal of any operation performed on the lower face—based on patient’s age and motivation level
b. Elderly
i. Static procedures are preferred
ii. Static slings establish oral symmetry in repose using grafts of temporalis fascia, fascia lata, palmaris/plantaris tendon, or alloplastic materials
iii. Unilateral rhytidectomy for patients with lax skin
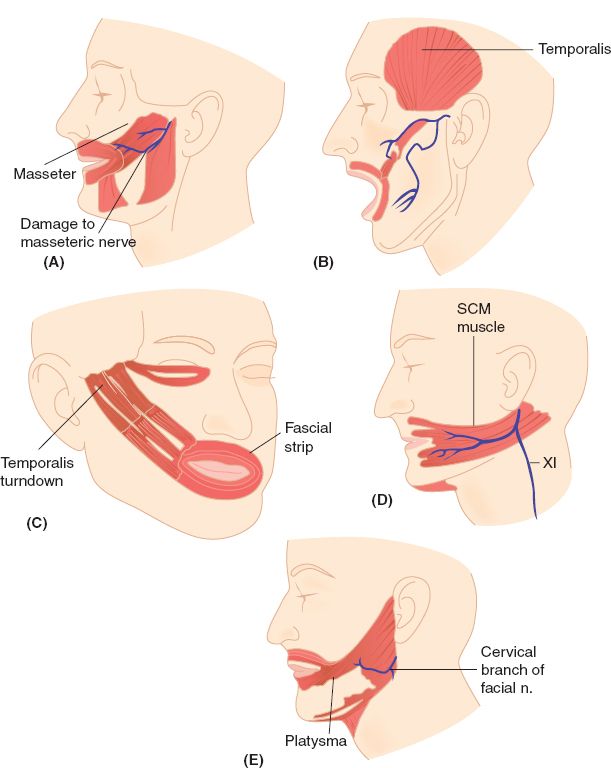
Figure 24-2. Examples of regional muscle transfer options for lower face reanimation in the adult. A: Masseter muscle transfer. B: Temporalis muscle transfer with fascial extension (McLaughlin procedure). C: Temporalis muscle turndown with fascial strip (Rubin procedure). D: Sternocleidomastoid (SCM) muscle transfer. E: Platysma muscle transfer.
c. Adults (Fig. 24-2)
i. Static slings or regional muscle transfers can be used
ii. Donor muscles: Masseter, sternocleidomastoid, and platysma muscles
iii. McLaughlin procedure: Transfer of the temporalis muscle insertion from the coronoid process with fascial extension
iv. Rubin procedure: Temporalis muscle turndown with fascial extension
v. Although touted as dynamic procedures, excursion is not as dramatic as seen in free microneurovascular muscle transfers
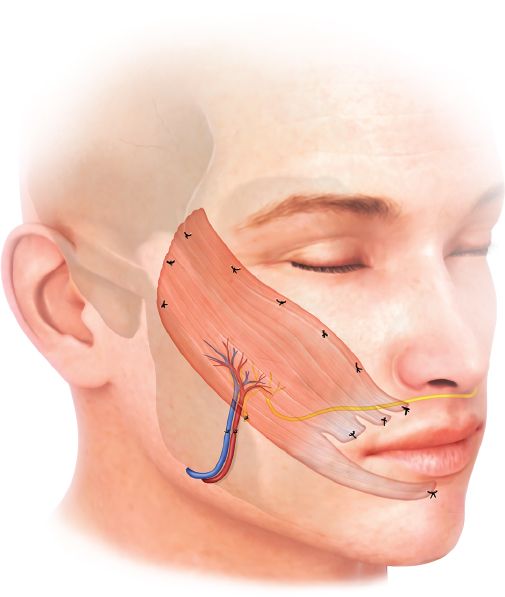
d. Young, highly motivated patients (Fig. 24-3)
i. *Best candidates for free microneurovascular muscle transfer
ii. Donor muscles: Gracilis (most common), latissimus dorsi, rectus abdominis, extensor digitorum brevis, serratus anterior, and pectoralis minor
Figure 24-3. Free microneurovascular gracilis muscle transfer.
iii. Double-stage: CFNG is performed during the first stage and muscle is transferred 9 to 12 months later during the second stage
iv. Single-stage: First stage is eliminated because the donor muscle has a long nerve for tunneling across the face or is coaptated to the ipsilateral XII or masseteric branch of V.
e. Lower lip symmetry can be achieved with botulinum toxin injection (temporary) or surgical division (permanent) of the contralateral lower lip depressors
PEARLS
1. Bell’s palsy is the most common cause of unilateral facial paralysis in adults (diagnosis of exclusion) and may be treated with oral corticosteroids and antivirals if started within 72 hours of symptom onset.
2. Children are obligate diaphragmatic breathers, so avoid using the phrenic nerve during nerve transfers.
3. All mimetic muscles are innervated on their deep surface, except for the buccinator, levator anguli oris, and mentalis.
4. An upper motor neuron lesion manifests as contralateral lower facial paralysis, whereas a lower motor neuron lesion manifests as ipsilateral total facial paralysis.
5. The paralyzed side of the face will display less fine wrinkling, but more tissue laxity (i.e., ptosis) compared to the contralateral normal side.
QUESTIONS YOU WILL BE ASKED
1. What three anatomic landmarks help identify the facial nerve as it exits the stylomastoid foramen?
Tragal pointer, tympanomastoid suture, and posterior belly of the digastric muscle.
2. Describe how to find the temporal branch of the facial nerve.
Follows the course of a line drawn from 0.5 cm below the tragus to 1.5 cm above the lateral brow.
3. What structures are continuous with the SMAS?
Superficial temporal fascia (temporoparietal fascia) superiorly and platysma inferiorly.
4. What nerves are commonly used to reinnervate paralyzed facial muscles?
Contralateral VII, masseteric branch of V, and XII.
THINGS TO DRAW
Draw the course of the extratemporal facial nerve.
Recommended Readings
Baker DC, Conley J. Regional muscle transposition for rehabilitation of the paralyzed face. Clin Plast Surg. 1979;6(3):317–331. PMID: 385211.
Harii K, Ohmori K, Torii S. Free gracilis muscle transplantation, with microneurovascular anastomoses for the treatment of facial paralysis. A preliminary report. Plast Reconstr Surg. 1976;57(2):133–143. PMID: 1250883.
Rubin LR. The anatomy of a smile: its importance in the treatment of facial paralysis. Plast Reconstr Surg. 1974;53(4):384–387. PMID: 4815693.
Terzis JK, Konofaos P. Nerve transfers in facial palsy. Facial Plast Surg. 2008;24(2):177-193. PMID: 18470829.
Wells MD, Manktelow RT. Surgical management of facial palsy. Clin Plast Surg. 1990;17(4):645–653. PMID: 2249385.
< div class='tao-gold-member'>