CHAPTER 6 Facelift anatomy, SMAS, retaining ligaments and facial spaces
Anatomically correct facial rejuvenation surgery is the basis for obtaining natural appearing and lasting results. The complexity of the anatomy of the face, and especially that of the midcheek, accounts for the formidable reputation of facial surgery. This is to the extent that many surgeons design their rejuvenation procedures around an avoidance of anatomical structures, and thereby limit the intent to camouflaging of the aging changes.
Functional evolution of the face
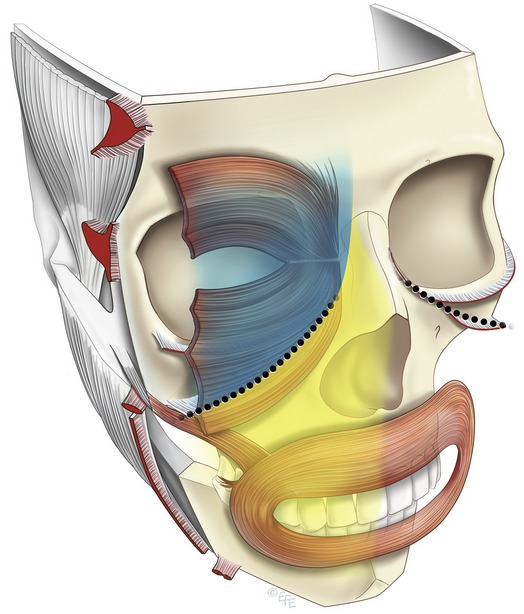
The anatomy of the face is more readily understood when considered from the perspective of its evolution and the function of its components (Fig. 6.1). Located at the front of the head, the face provides the mouth and masticatory apparatus at the entrance to the embryonic foregut, as well as being the location for the receptor organs of the special senses: eyes, nose and ears. The skeleton of the face incorporates a bony cavity for each of these four structures. Those for the special senses have a well-defined bony rim, in contrast to the articulated broad opening of the jaws covered by the oral cavity. The soft tissues of the face, integral to facial beauty and attraction, are in reality, dedicated entirely to their functions.
Regions of the face
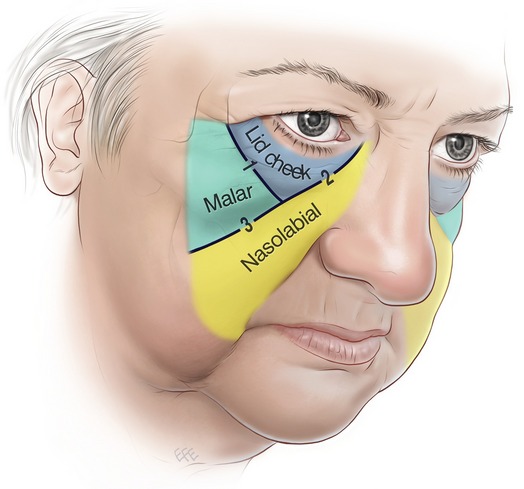
The traditional approach to the face in thirds (upper, middle and lower) while useful, limits conceptualization, as it is not based on the evolving structure. The significant muscles of facial expression are all located on the front of the face (anterior aspect) predominantly around the eyes and mouth, where their effect is seen in communication. For these functional reasons the anterior aspect of the face contains the more delicate expressive areas, which are prone to developing aging changes (Fig. 6.2).
In contrast, the lateral face is relatively immobile as it passively overlies the structures to do with mastication, which are all deep to the investing deep fascia. These are the temporalis and masseter on either side of the zygomatic arch, along with the parotid and its duct. The only superficial muscle in the lateral face is the platysma in the lower third, which reaches no higher than the oral commissure. Internally, a distinct boundary separates the mobile anterior face from the lateral face. The vertically oriented line of retaining ligaments attached to the facial skeleton forms this boundary (Fig. 6.2).
From the perspective of priorities in rejuvenation surgery, the midcheek is the most important area of the face, because of its prominent central location between the two facial expression centers, the eyes and the mouth. The periorbital and the perioral parts overlap in the midcheek (Fig. 6.2). The periorbital part overlies the body and orbital process of the zygoma, while the perioral part overlies the maxilla, a bone of dental origin. The functional parts are inherently mobile and meet at the relatively immobile boundary that extends in an oblique line across the midcheek. This is the midcheek groove formed by the dermal extensions of the zygomatic ligaments (Fig. 6.3).1
The facial nerve in relation to regions of the face
The level in which the facial nerve branches travel relates to the region of the face (Fig. 6.4). In the lateral face below the zygomatic arch the branches remain deep to the investing deep fascia. In the anterior face (and above the lower border of the zygoma) the branches are more superficial in relation to their muscles. The transition in levels occurs at the retaining ligament boundary, which is the last position of stability before the mobile anterior face. The nerves are protected here as they course outward to their final destination
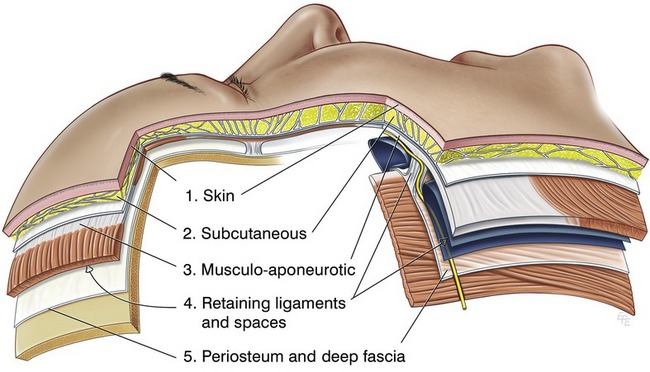
Fig. 6.4 The layers of the face. The five layers of the scalp are a prototype of facial anatomy and the simpler basis for the more complex structure elsewhere on the face. Layer 4 is the most changed layer, consisting of alternating spaces and ligaments. The course of the facial nerve changes level at the ligamentous boundary transition from the lateral to the anterior face. Mendelson BC, Jacobson SR. Surgical anatomy of the midcheek: facial layers, spaces, and the midcheek segments; Clin in Plast Surg 2008;35:395–404.
Layers of the face
The principles of facial structure can be summarized quite simply:
1. The scalp is the basic prototype for understanding facial anatomy, as it is the least differentiated part of the face (Fig. 6.4).
2. The face is constructed of concentric soft tissue layers over the bony skeleton.
3. The five layers of the scalp are: (i) skin; (ii) subcutaneous; (iii) musculo-aponeurotic; (iv) areola tissue; (v) deep fascia.
4. The layers are not homogenous over the face proper, as they are modified in areas of function.
5. The key areas of function overlie the bony cavities, especially the eyelids and the cheeks and mouth.
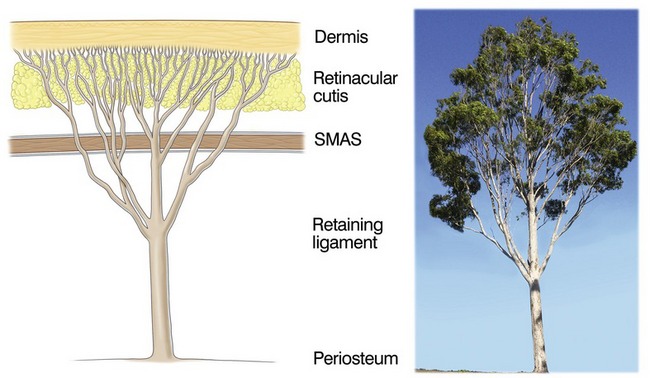
6. A multilinked fibrous support system supports the dermis to the skeleton (Fig. 6.5). The components of the system pass through all layers.2
7. At the transition between that over the skeleton to that overlying the cavities (eyelids and mouth) there is a modification of the anatomy.
8. The complexity of the facial structure results from the balance required between mobility and stability (ligamentous support).
Details of the layers
Layer one – skin
The structural collagen of the dermis is the outermost part of the fibrous support system and is intrinsically linked, both embryologically and structurally, with the collagenous tissue of the deeper layers. The thickness of the dermal collagen relates to its function, and tends to be in inverse proportion to its mobility. The dermis is thinnest on the eyelids and thickest on the forehead and nasal tip. The thinner, more mobile dermis is susceptible to an increased tendency for aging changes.
Layer two – subcutaneous
Each of the three midcheek segments has a distinctly different thickness of subcutaneous fat. The subcutaneous layer is thinnest in the lid–cheek segment adjacent to the lid proper. In the malar segment the layer is moderately thick and uniform, whereas it is markedly thicker in the nasolabial segment, which has the thickest layer of subcutaneous fat of the face. Where the subcutaneous fat is thicker, the retinaculum fibers are lengthened and more prone to weakness and distension. The thick subcutaneous fat in the nasolabial segment is named the malar fat pad, which is confusing terminology given that its position is predominately medial to the prominence of the zygoma in the perioral part of the midcheek3,4 (Fig. 6.2).
Within the subcutaneous layer, the attachment to the overlying dermis is stronger than on its deep surface, due to the tree-like arrangement of the retinacular cutis fibers (Fig. 6.5). In superficial, i.e. subdermal, dissection of the subcutaneous layer, many fine retinacula cutis fibers are encountered. At the interface with the underlying layer 3, there are fewer, though larger fibers and less subcutaneous fat, which appears not to descend fully to the interface where it overlies the superficial muscles, orbicularis oculi and platysma.
The retinacular fibers are not uniform across the face, but vary in their orientation and arrangement according to the region. This variation mirrors the anatomy of the underlying 4th layer. As will be more apparent when the 4th layer is discussed, the line of retaining ligaments continue vertically through the subcutaneous layer to form septae, that form boundaries which compartmentalize between more mobile areas.5 Accordingly, where the subcutaneous layer overlies spaces (in the 4th layer) there are no vertically oriented subcutaneous ligaments extending through. In contrast, the retinacular fibers overlying the spaces have a predominantly horizontal orientation, being in strata-like layers that are less restrictive to underlying movement.
Layer three – musculo-aponeurotic
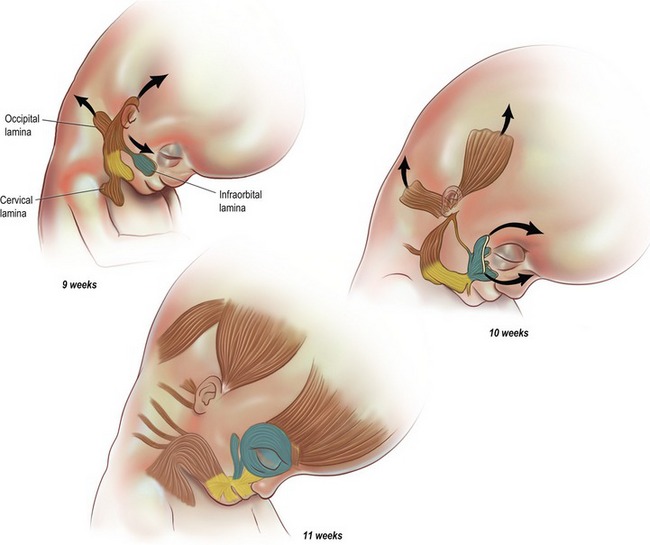
In the prototype scalp, the third layer demonstrates key principles about the facial muscles. The superficial muscle, occipito-frontalis, moves the overlying soft tissues including the skin of the scalp and forehead. While the muscles have a minimal area of bony origin, which is remote (on the superior nuchal line), they have an extensive area of insertion into the overlying soft tissues.
The fibrous sheath enclosing the frontalis and occipitalis is continuous across the entire scalp, whereas the enclosed muscles are discontinuous. Where the fascia is present without intervening muscle, the superficial and deep layers of the sheath are apposed and fused to form the galea aponeurotica. This is the basis for the aponeurotic part of the 3rd layer. The superficial fascial layer is thin where it overlies the muscle, and in areas such as over the forehead, muscle fibers extend into the subcutaneous layer. In contrast, the deep layer of the fascia is thicker, more supporting and provides a gliding surface at the interface with the underlying 4th layer. The original description of the SMAS (superficial muscloaponeurotic system) in 1976 was essentially a description of this 3rd layer, as is applies to the mid and lower thirds of the face.6 The flat superficial muscle component predominates in some areas of layer 3, while in areas without muscle the aponeurotic element predominates.
The definitive muscles in level 3 have a layered arrangement. The broad flat muscles form the superficial layer that covers the anterior aspect of the face: frontalis overlies the upper third and orbicularis oculi the middle third. The platysma, over the lower third extends onto the lateral face, presumably related to jaw movement, which functionally dominates the lower third. The superficial muscles are more closely related to the overlying subcutaneous layer than they are to the deeper structures. The superficial flat muscles have a minimal direct attachment to the bone. They are indirectly stabilized to the skeleton by a ligament, located at the lateral border of the muscles. The frontalis is fixed by the superior temporal ligament along the superior temporal line, the orbicularis oculi is stabilized by the main zygomatic ligament at its inferolateral border and the platysma is stabilized at its upper border by the upper key masseteric ligament (Fig. 6.15).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree