Key words
cheeks, nose, lips, scarring, flaps, Z-plasty, microstomia
Synopsis
The burned face presents a challenging problem that must be addressed in a comprehensive and thoughtful manner. This is further complicated by the demand for not only a functional result but also one that is esthetically acceptable. Of the many facial structures that are affected in burn injury, this chapter will focus in particular on the cheeks, the nose, and the lips.
Clinical Problem
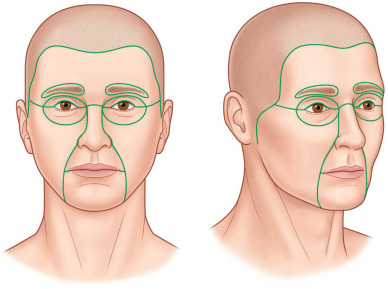
The face is a complex, three-dimensional structure comprising myriad tissue components that are altered or destroyed by burn injury. The simplest method of reconstruction may not be the preferred or optimal approach in burn reconstruction, and thoughtful deviation from the traditional “reconstructive ladder” may be appropriate. Burned tissue scars cause changes that are readily noticeable in the face: contractures; decreased pliability; alopecia; changes in surface, color, and texture; and fragility of tissues and structures. Furthermore, wound bed scarring impairs revascularization of grafted tissues. The cheeks, nose, and lips regions are of varying importance in their contribution to the appearance of the face and must be approached differently ( Fig. 4.4.1 ). The nose and lips are central facial units; they are of critical importance to the appearance of the face. The cheek is a peripheral unit of the face and is of secondary importance to the appearance of the face. Absolute symmetry is less vital between the two cheeks than with other structures. Regardless of the structure, there are common goals to the reconstruction of all facial burns. In his 1995 paper, Rose describes the following goals: a “normal” appearance at conversational distance, a face that is balanced and symmetrical, distinct esthetic units connected by inconspicuous scars, a soft skin texture that will bear corrective makeup, and the ability for dynamic and natural facial expression.
Burn reconstruction in the developing world poses a number of distinctive challenges, most notably the lack of resources and technology that surgeons have at their disposal. Without lasers or microsurgical capabilities, burn reconstruction in the developing world relies primarily on scar release and skin grafting as well as local tissue rearrangement and locoregional flaps for releasing contractures and resurfacing scarred regions.
Pre-Operative Management
The cheek is a peripheral unit of the face. It traces the preauricular contours of the ear, across the zygoma and inferior to the temporal fossa, to the lower eyelid-cheek junction, along the sidewall of the nose to the nasolabial fold and marionette line. The color of the skin is similar to that of the rest of the face; it is hair-bearing with a fine matte hair in women and with a beard in men. Although it is largely flat, it has some important contours, including those at the malar eminences and adjacent to the nasolabial folds.
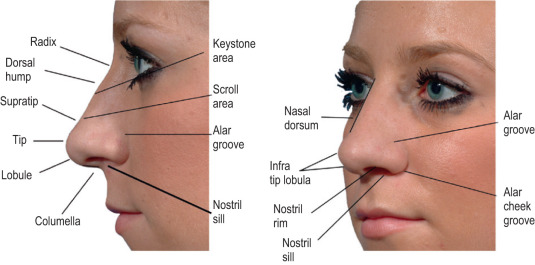
The nose poses a unique challenge among facial structures because of its complex three-dimensional structure and underlying bony and cartilaginous skeleton. The structure is, of course, divided into the subunits of radix, dorsum, tip, columella, two sidewalls, two ala, and two soft triangles ( Fig. 4.4.2 ). Functionally, the goal is a functional nose that allows for normal breathing and speech. As such, the prevention and correction of nasal stenosis is crucial.
Like the nose, the lips and perioral region are central features of the face. The normal lip is similarly a complex structure with distinct features including the oral commissures, the philtrum and Cupid’s bow, and the vermilion and moist lines. Reconstruction, as with elsewhere in the face, should be aimed at restoration of normal esthetics as well as a functional mouth. Microstomia and lower lip eversion are common functional deficits encountered with burns to the lips and perioral region.
Typically, no additional pre-operative testing is needed for treatment of facial burns, other than routine laboratory work as needed.
The timing and approach to facial burn reconstruction is a nuanced discussion in its own right. Early reconstruction focuses on covering vital structures such as bone and cartilage, limiting the formation of contractures, and preventing functional problems such as ectropion, nasal stenosis, contractures limiting facial movements, and microstomia. This is addressed through debridement and grafting of the initial burn. As with any wound, the burn must be under control, clean, and no longer progressing before reconstruction should be pursued. Once scars have formed, the traditional approach is excision down to at least the level of superficial muscular aponeurotic system (SMAS) or superficial fascia, followed by reconstruction. However, modern burn reconstruction provides additional options to the traditional excision and full-thickness skin graft approach. When burn scars affect the cheek and central face, reconstruction should be staged. The cheek scars should be managed first to better control for scar contracture from any cheek reconstruction.
Supplies needed for most burn reconstructive surgery with skin grafting, tissue rearrangement, and locoregional flaps are limited to standard surgical instruments, a source of cautery, sutures, and dressings. More advanced techniques such as lasers and microsurgery will require specialized equipment, which may not be available in the developing world.
Communication with the anesthesiologist is critical, however, to ensure that the choice of airway does not interfere with the surgical site, and to minimize fire risk. Additionally, records should be obtained with regard to previous tracheostomy, and the surgeon should look with a scope pre-operatively if releasing the neck near the previous tracheostomy site to ensure no fistula. Anesthesia is typically general endotracheal anesthesia, though sedation and local anesthesia can be used for smaller operations. If the patient has microstomia from his or her burns, an awake fiber-optic intubation may be indicated. Finally, nasotracheal intubation may be needed if release of the lips and perioral area is being performed.
Surgery
The Cheek
In the cheek, it is typically unnecessary to excise all adjacent normal tissue in the unit just to resurface a segment of it. Functionally, management of cheek scars is important to preserve the function of adjacent structures such as the lower lid and the mouth. Skin grafts are an appealing option for resurfacing regions of the cheek due to their technical simplicity, but they are almost by requirement different in color and texture from their recipient site, and can cause a patchy appearance accordingly. If they are to be used, care must be taken to use skin that is most like that of the recipient region, such as supraclavicular skin. Fig. 4.4.4 demonstrates a patient who had good results from debridement and sheet grafting to the cheeks, which was later revised with further release and full-thickness skin graft to the left cheek and laser treatments to the face. Deep wounds to the cheek can be troublesome for reconstruction because of the risk of facial nerve involvement or scarring around the facial nerve, involvement or scarring of the parotid (Stensen’s) duct, and the need for thickness of the soft tissues and a functional oral lining. When there are deficits of the latter two, fat-grafting and de-epithelialized pedicled or free flaps can provide thickness to the buccal region and oral lining if needed.
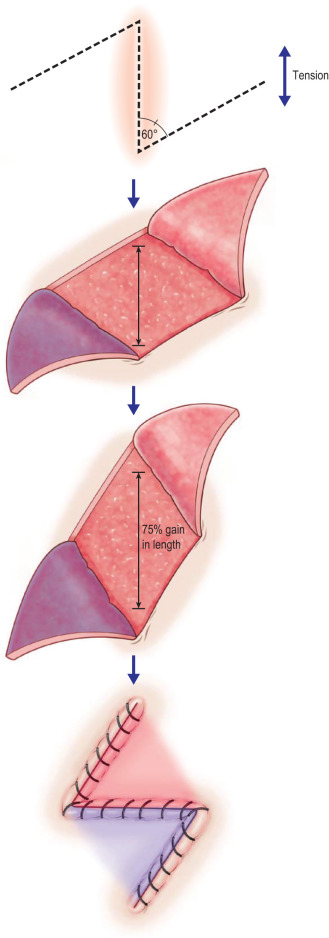
Cheek defects can often be approached with a number of local flaps. Small defects can be closed primarily if it can be done without distorting surrounding structures. Moderately sized defects can be closed with rotation and advancement flaps from adjacent tissue; cervical advancement is useful for lower cheek defects. When using random and local flaps and local tissue rearrangement such as Z-plasties, technique is essential. Tissue should be handled gently with skin hooks rather than forceps. Flaps should be made thick enough to ensure that vascularized tissue is included, incorporating the fascia when possible. The tips of small flaps can be blunted to decrease tip necrosis. In our experience, truncating the tips of Z-plasty flaps appears to improve the viability of flap tips ( Fig. 4.4.3 ).