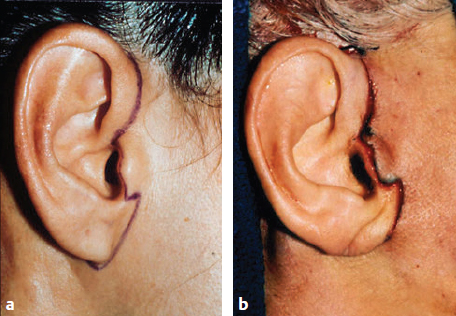
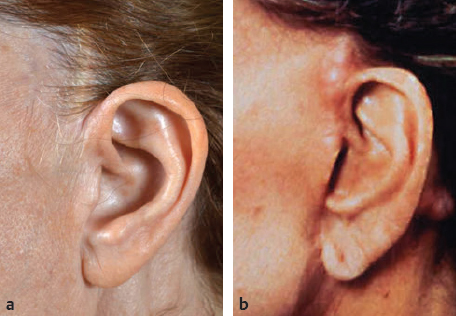
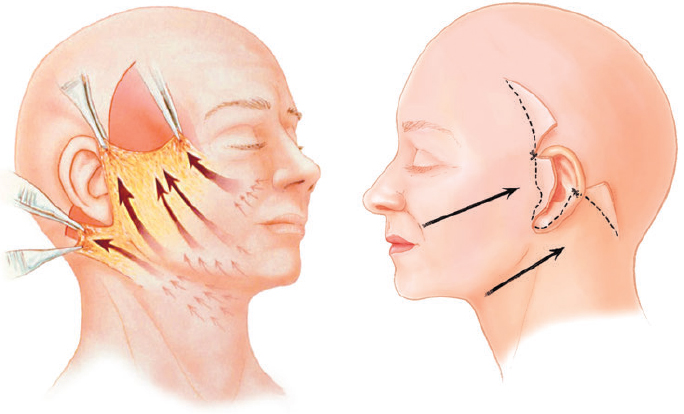
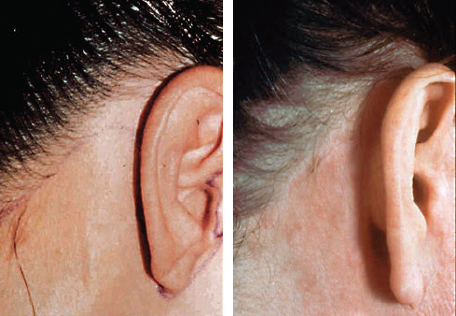
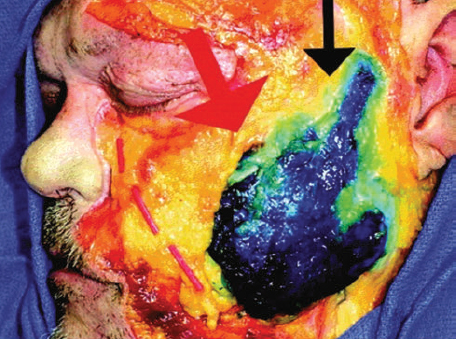
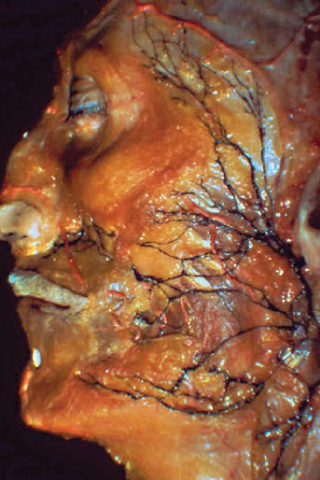
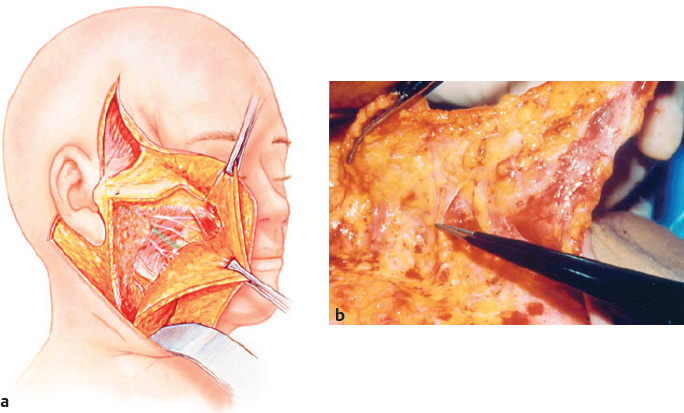
CHAPTER Surgical rejuvenation of the aging face is one of the most challenging procedures facing plastic surgeons interested in cosmetic surgery. The difficulties that the plastic surgeon encounters include individual variations in facial shape; variability in the quality of soft tissue; and the morphologic changes that occur with aging, which are patient specific. Skeletal support, the age of the patient, skin quality, the degree of descent of facial fat, the descent of the cervical platysma, and lipodystrophy of the face and neck all affect treatment planning and the postoperative result. There is no simple surgical algorithm in terms of technical approach that provides for consistency in results. Expectations are extremely high in most patients seeking a facelift. Although repositioning facial fat and correcting skin laxity will typically improve patient appearance, surgical rejuvenation of the aging face is not the “fountain of youth.” Patients will appear younger, but chronologic age dominates morphologic improvement. In some patients this leads to frustration, and in others the need for revision and further surgery to improve undercorrection. An understanding of the aesthetic ideal that is possible for a particular patient in terms of restoration of facial shape, in my opinion, is the key to consistency in results. Improving contour, while minimizing signs of surgical distortion, remains the main element in avoiding unfavorable results in facial rejuvenation. Summary Box Unfavorable Results and Complications in Face and Neck Rejuvenation Technical Errors • Incision design (pixie ear) • Inset of skin flap (hairline distortion) • Dissection of skin flap (overly thin or overly thick); venous congestion • Facial nerve injury Postoperative Care • Hematoma • Infection • Seroma Aesthetic Errors • Issues with skin tension (leading to hypertrophic scarring and alopecia) • Improper vectoring of facial skin (leading to misdirected, vertically oriented facial rhytides, as well as a flat contour along the lateral cheek [cross-cheek depression]) • Over defatting of the neck • Inadequate volume restoration • Undercorrection • Limited longevity of results • Recurrent platysma bands Technical errors in facelifting are unforgiving. Errors in an incision design and inset of the skin flap can lead to visible scarring. Errors in dissection of the skin flap can lead either to overly thin flaps prone to venous congestion or overly thick flaps that lead to a diminished utility for facial fat repositioning via a superficial muscular aponeurotic system (SMAS) flap. Inadvertent dissection deep to the superficial and deep fascia can lead to facial nerve injury. Improper defatting of the neck and jowls can lead to contour irregularities. Meticulous postoperative care of the patient is another factor in avoiding unfavorable results in facelifting. A postoperative hematoma, if untreated, can lead to scarring and delayed healing. Untreated infections can lead to skin slough. Untreated seromas, most commonly noted in the neck, may result in cervical irregularities. Postoperative complications commonly lead to further revision surgery and often a dissatisfied patient. Aesthetic errors in facelifting are perhaps more common than technical errors. The most common aesthetic error is the untoward use of skin tension, which can result in hypertrophic scarring and alopecia. Improper vectoring of facial skin can lead to misdirected, vertically oriented facial rhytides, as well as a flat contour along the lateral cheek, which aesthetically produces a tight unnatural facial appearance. Vertical vectoring of facial skin in a patient with lateral cheek deflation is also associated with the development of the so-called “lateral sweep,” or more medially what has been termed a cross-cheek depression, also known as a “joker line.” Overdefatting of the neck through the untoward use of liposuction can result in a harsh cervical appearance and accentuate underlying cervical irregularities. Inadequate volume restoration to correct deflation is typically noted in both the perioral region and central cheeks and requires volumetric enhancement as part of the original surgical procedure, as well as maintenance treatment to maintain correction. Because of the variations in the quality of soft tissue among patients, undercorrection in facial rejuvenation is common. This is especially true in treating elderly patients (older than 60 years) and patients with inelastic, sun-damaged skin.1 Simply put, poor-quality soft tissue does not maintain the contour correction after intraoperative repositioning, leading to recurrence of laxity over time. Undercorrection is typically most evident along the jawline and within the neck. Sun damage is more common in cervical skin than facial skin, is thinner, and tends to relax at a more rapid rate than the thicker facial skin. The most common area to develop recurrent cervical skin laxity is the region just cephalad to the sternal notch and clavicle. Recurrent platysma bands also occur despite a properly performed platysmaplasty. Undercorrection and recurrent laxity are a source of frustration for both surgeon and patient, and in some patients, revision surgery is necessary to correct recurrent laxity. Perhaps nothing concerns patients more than the quality of the access incisions used in facelifting. If the incisions are improperly planned or poorly inset, scars may widen, the tragus can appear distorted, and the earlobe can be pulled anteriorly. The unfavorable result of a poorly planned operative access incision is a noticeable scar, which is a telltale sign that the patient has undergone a surgical procedure. Surgical revision of poorly planned incisions typically improves the result, but the best chance for a good quality imperceptible scar is at the initial procedure. Preauricular incisions, which are designed anterior to the tragus, offer the advantage of allowing for more skin tension without disturbing tragal definition. The aesthetic difficulty with preauricular incisions is that the color differential between the skin of the cheek and the skin of the ear tends to be more abrupt and therefore more visible in an anterior location (Fig. 21.1) Tragal incisions usually provide better camouflage, but they can produce postoperative distortion of the tragus. To avoid tragal distortion, the access incision needs to be designed to provide a visible beginning along the cephalad border of the tragus, extend along the tragal margin, and then provide for a visual ending of the tragus, preserving the incisura along the caudal aesthetic unit of the cartilage (Video 21.1). Inset of the skin flap with minimal tension along the aesthetic subunit of the tragus is a key element for consistency in terms of scar perceptibility1,2 (Fig. 21.2) A pixie ear deformity occurs when excessive skin tension is used, and the earlobe is pulled anteriorly. To avoid the pixie ear deformity, it is often preferable to leave a small amount of cheek skin, approximately 2 mm, attached to the earlobe when designing the incision along the base of the earlobe. This leaves a rim of cheek skin immediately inferior to the lobule that can be used for reattachment at the time of closure, allowing for the creation of a detached earlobe that is separate from the cheek. When inserting the earlobe, it is also important to reposition approximately one centimeter of the skin flap pos terior to the earlobe, so the earlobe hangs separate and detached from the cheek skin. The earlobe should also be inset approximately 15 to 20 degrees posterior to the axis of the pinna, which provides for a more natural appearance and prevents the pixie ear deformity1,2 (Fig. 21.3). Fig. 21.1 Preauricular incisions, which are placed within the preauricular sulcus, avoid the tragus and prevent tragal distortion, and therefore tolerate the use of greater skin tension during flap inset. The disadvantage of preauricular incisions is that the color difference between the blush skin of the cheek and the pale skin of the ear is more noticeable in this anterior location. Fig. 21.2 (a) Intratragal incisions should be designed to parallel the descending visual width of the helix and establish a V-like intratragal notch along the superior aspect of the aesthetic unit of the tragus. The inferior limb of the intratragal incision should preserve the incisura along the caudal extent of the tragus, such that the rectangular shape of the tragus is preserved. A 2- to 3-mm cuff of cheek skin is left intact adjacent to the earlobe to allow for the creation of a detached lobe after flap inset. (b) The inset of the skin flap along the tragus needs to be precise, with little or no tension during flap closure. Fig. 21.3 (a) A pixie ear is a result of poor control of skin tension and is caused by insetting the earlobe along the longitudinal axis of the ear or anterior to the axis of the pinna. Creation of an earlobe that is directly attached to the cheek skin typically is unaesthetic and a common stigma associated with a facelift. To avoid the pixie ear deformity, the earlobe should be inset 15 to 20 degrees posterior to the longitudinal axis of the pinna, and skin tension around the earlobe should be limited so the lobule is not pulled anteriorly. Advancing approximately 1 cm of skin posterior to the lobule allows the creation of a detached earlobe distinct from the cheek, which appears more natural. (b) Well-designed tragal incisions often provide adequate scar perceptibility, appearing as a color difference between the blush skin of the cheek and the pale skin of the ear rather than an obvious scar. This patient’s detached earlobe that lies posterior to the longitudinal axis of the pinna has a natural appearance. Both the temporal and postauricular hairline can be distorted by facelift procedures. Temporal hairline distortion and elevation of the sideburns typically result from vertical skin flap redraping (Fig. 21.4). Surgeons who use a vertical skin redraping, such as in short-scar facelifting, therefore typically prefer to use a temporal hairline incision to avoid elevation of the sideburn. An alternative to temporal hair line incisions, which are often unpopular in patients who spend significant time outdoors, is to design the anterior incision within the temporal hair and avoid vertical vectors in skin flap redraping. My personal preference is to use vertical vectors for facial fat repositioning via the SMAS rather than more oblique repositioning of cheek skin, thereby avoiding temporal sideburn elevation. Judicious use of tension limits the possibility of alopecia1,3 (Fig. 21.5, Video 21.2) Fig. 21.4 (a) Vertical skin flap redraping can elevate the temporal hairline and sideburn unless the temporal incision is placed anteriorly along the temporal hairline. This patient has an unaesthetic elevated sideburn after a short-scar facelift with vertical skin flap redraping. (b) Another example of temporal hairline distortion and widening of the temporal scar associated with vertical skin flap redraping and the use of strong skin tension during skin flap inset. Fig. 21.5 An alternative to vertical skin flap redraping is to vector facial fat vertically using the superficial muscular aponeurotic system while using a more oblique vector for facial skin, which prevents vertical elevation of the sideburn. (Reproduced from Nahai F, ed. The Art of Aesthetic Surgery, Principles and Techniques. 2nd ed. New York: Thieme Medical Publishers; 2011.) Postauricular hairline shifts can occur if the incisions are not properly planned. In general, I prefer to use partial hairline incisions in the postauricular region to avoid stair-stepping of the postauricular hairline. After cervical skin flap redraping, most of the cervical skin excision occurs within the hairless superior aspects of the incision, whereas the inferior hairline is realigned to avoid stair-stepping. Obviously, the avoidance of excess of skin tension to produce a fine line scar is critical so patients can wear their hair up without fear of a noticeable scar (Fig. 21.6). Perhaps one of the most difficult technical aspects of performing a facelift is accurate subcutaneous undermining of the cheek. Because of the variations in terms of facial subcutaneous fat thickness among patients, in some the skin flap will be quite thin, whereas in others, it will be robust and thick. Overly wide dissection of the skin flaps, especially in thin patients, can lead to venous congestion and should be avoided if possible. If the skin flap appears to be overly thin with little subcutaneous fat, it is perhaps best to limit the dissection within the lateral cheek rather than to risk wide undermining and subsequent skin flap ischemia. I find the most helpful method for precisely performing accurate subcutaneous undermining is the use of transillumination and skin flap dissection performed under direct vision (Fig. 21.7). When dissecting the skin flap in the subcutaneous plane, the terminal fibers of the retaining ligaments that compartmentalize subcutaneous fat will be encountered. Typically, the dissection in the preauricular region is fibrous and vascular dissection is performed within the fibrous lateral fat compartment. Approximately 4 cm anterior to the preauricular incision, the dissection will become less fibrous, and a thicker skin flap will be more easily dissected as the surgeon operates within the middle fat compartment. For subcutaneous undermining, I prefer to dissect thick skin flaps in the middle compartment, dissecting caudally along the interface between the subcutaneous fat and SMAS to preserve flap thickness and vascularity. Superiorly, in the region along the zygomatic arch and malar eminence, where the SMAS is going to be dissected, I prefer to dissect thin skin flaps, leaving the subcutaneous fat intact overlying the SMAS flap. Differential thickness in subcutaneous cheek dissection helps to preserve vascularity of the skin flap while allowing the extended SMAS flap to be raised with sufficient thickness to avoid tearing during dissection4 (Fig. 21.8). Fig. 21.6 Postauricular incisions are typically planned as partial hairline incisions; the superior limb is designed along the hairline to allow removal of non–hair-bearing skin and inferiorly extends into the occipital hair. Partial hairline incisions provide for cervical skin removal while preventing stair-stepping of the postauricular hairline. Control of skin tension is an important aspect of limiting scar perceptibility. Fig. 21.7 Transillumination is a useful technique that allows for precise skin flap dissection. To perform transillumination, a light (such as the contralateral operating room light) is placed on the opposite side of the patient from the surgeon and is directed through the skin flap to illuminate the interface between the subcutaneous fat and the superficial muscular aponeurotic system. This allows the surgeon to operate under direct vision and dissect precise skin flaps. Fig. 21.8 Facial subcutaneous fat is divided into a series of fibrous compartments. The initial subcutaneous dissection begins within the lateral compartment. Most of the dissection in the cheek is within the middle compartment, which is thicker and easier to dissect (stained blue). When the fibrous zygomatic ligaments are encountered lateral to the malar eminence (large red arrow), care is required to prevent dissecting deep to the superficial muscular aponeurotic system, because the zygomatic branches of the facial nerve are superficial in this location. (Reproduced from Rohrich R, Pessa J. The fat compartments of the face: anatomy and clinical applications. Plast Reconstr Surg 2007;119:2219–2297.) The most important point in avoiding facial nerve injury in a facelift is to understand the plane of dissection and recognize the danger zones during specific regions of the procedure. In general, if the subcutaneous dissection is carried superficial to the SMAS, motor branch injury will be prevented. Similarly, in dissecting an SMAS flap, dissecting in the interface between superficial and deep fascia, and avoiding dissection deep to the deep fascia, will protect the underlying facial nerve branches. The most common danger zone in dissecting subcutaneous fat of the cheek is in the region directly inferior and lateral to the zygomatic eminence where the upper masseteric ligaments are encountered. This tends to be a fibrous area of dissection, and the underlying zygomatic nerve branches are superficially positioned directly deep to the SMAS in this location. When encountering this fibrous region of dissection inferior to the zygomatic eminence, it is helpful to recognize that this is a danger zone and dissect this area carefully, ensuring that the dissection is subcutaneous and not subSMAS in this specific location (Fig. 21.9; see also Fig. 21.8). In terms of elevation of the SMAS flap, one useful element to provide safety in SMAS dissection is to dissect directly along the posterior surface of the superficial fascia and leave the subSMAS fat intact along the underlying deep facial fascia. Dissecting along the undersurface of the SMAS and not within the subSMAS fat provides greater soft tissue protection for the underlying facial nerve branches and decreases the risk of motor branch injury. The most dangerous region for nerve injury during an extended SMAS dissection is directly inferior and lateral to the zygomatic eminence when releasing the upper masseteric ligaments. Similar to the cutaneous plane, the zygomatic branches are in close proximity in this region, and careful dissection just along the undersurface of the SMAS is essential in preventing zygomatic nerve injury in this area. Once the dissection is carried anteriorly into the mobile region of the SMAS, anterior to the retaining ligaments, the dissection should be terminated, because facial nerve branches become more superficial in this location. Further dissection anteriorly within the mobile area of the cheek increases potential morbidity without recruiting greater movement of the SMAS and is not necessary to obtain adequate SMAS mobilization5 (Fig. 21.10). Hematoma is the most common postoperative complication after a facelift (approximately 70% of all complications).6 The range of hematoma formation is between 1 and 8% in most series, and males have a higher incidence of hematoma formation compared with females.6 Fig. 21.9 A cadaver dissection of the facial nerve branches. During subcutaneous dissection, two danger zones, where the facial nerve is superficially positioned just beneath the superficial muscular aponeurotic system (SMAS), are located along the superior and inferior border of the masseter associated with the upper and lower masseteric ligaments. Dissection deep to the SMAS in these regions can lead to injury of either the zygomatic or cervical branches of the facial nerve. (This dissection and image are provided courtesy of Dr. Julia Terzis.) Fig. 21.10 (a) In an extended superficial muscular aponeurotic system (SMAS) dissection, to liberate the SMAS from the restraints of the retaining ligaments, the SMAS is dissected from the parotid, the accessory lobe of the parotid, the lateral zygomatic ligaments, and the upper masseteric ligaments. Dissecting in the interface between the undersurface of the SMAS and the subSMAS fat (leaving the subSMAS fat down on the parotid capsule and deep fascia) provides safety in terms of prevention of facial nerve injury. (b) This intraoperative photograph shows the upper masseteric ligament (forceps) dissected at the termination of SMAS elevation, because just distal to this ligament the zygomatic branches course superficially. (Reproduced from Stuzin JM, Baker TJ, Baker TM. Refinements in face lifting: enhanced facial contour using Vicryl mesh incorporated into SMAS fixation. Plast Reconstr Surg 2000;105:290–301.) Although it is impossible to completely eliminate this postoperative complication, most authors have noted that the incidence of hematoma formation decreases with blood pressure maintenance. Many surgeons have noted that decreasing systolic blood pressure below 150 mm Hg both intraoperatively and postoperatively is important,6 and in my practice we try to keep the systolic blood pressure below 120 mm Hg in the recovery room. Patients who take antihypertensive medication preoperatively should maintain their medication regimen both preoperatively and postoperatively. Another important factor in limiting hematoma formation is to be proactive in preventing nausea and vomiting. Judicious use of narcotics to prevent nausea is similarly prudent. Although it seems obvious, perhaps one of the most important factors in avoiding a hematoma is the time spent intraoperatively performing hemostasis. I prefer to allow the epinephrine to wear off before closure and meticulously perform electrocautery hemostasis of all areas dissected. Although this is a tedious operative procedure, it typically pays dividends. In general, a very dry intraoperative field leads to a very low hematoma rate postoperatively. Patients who are relaxed and comfortable in the postoperative period typically have a more uneventful postoperative recovery. The use of antianxiety medication is often helpful in the early postoperative period, and these are typically not associated with nausea or vomiting. Most facelift patients do not have a significant amount of pain, and we have found that antianxiety medication is often helpful in providing comfort to the patient without any of the side effects associated with opiates. Seroma formation is most common in the cervical region, which typically heals slower than the face. Seroma formation is not only a nuisance to the patient, because it commonly requires serial aspiration, but it often leads to an untoward result that includes wrinkling and induration of sun-damaged cervical skin. Patients who develop seromas of the neck may require later surgical revision. Drains and tissue adhesives are useful in decreasing seroma formation. I favor drains, and I tend to leave drains in the cervical region in place for longer periods, often for 3 to 5 days. In terms of removing the drains, I am not necessarily guided by the amount of output, but rather leave the drains until the cervical skin is totally adherent to the underlying platysma muscle. I have found that tissue adherence rather than drain output is the best guide for seroma prevention. If a seroma does develop after drain removal, I see the patient daily and monitor the seroma with serial aspiration. In larger seromas (greater than 5 mL), I typically place a seroma catheter and leave it in place for 1 to 2 days until the cervical skin is adherent. Infection is rare in facelift patients, and it is most commonly secondary to Staphylococcus.6,7 Prophylactic antibiotics are helpful in minimizing this problem. An increasingly common type of Staphylococcus coagulase-negative infection is being noted in facelift patients around the country.6,7 I believe this largely has to do with the evolving microbiology and antibiotic resistance of Staphylococcus epidermidis to cephalosporins. Patients who develop coagulase-negative Staphylococcus infections typically present on day 3 postoperatively with small impetigo-type milia lesions in regions of venous congestion of the skin flap. If recognized, these patients should have the milia lesions evacuated and begin using topical antibiotic ointment. Daily administration of antibiotics with action against Staphylococcus (such as intravenous vancomycin) is important in preventing the progression of an S. epidermidis infection to cellulitis and flap necrosis (Fig. 21.11). If the condition is recognized early, typically 3 to 5 days of antibiotic treatment is all that is required. If the infection is allowed to proceed unabated to progressive cellulitis and purulence beneath the skin flaps, an invasive infection may develop and require hospitalization. The key to avoiding facelift infections is to see the patient on a regular basis and, if any signs of erythema or infection develop, to proceed aggressively, before skin erythema progresses to cellulitis.
21
Face and Neck Rejuvenation
Categorizing Unfavorable Results and Complications in Face and Neck Rejuvenation
Technical Errors
Aesthetic Errors
Undercorrection and Limited Longevity of Result
Avoiding Unfavorable Results and Complications in Face and Neck Rejuvenation
Avoiding Technical Errors
Incision Planning
Avoiding Pixie Ear
Avoiding Hairline Distortion
Avoiding Technical Errors in Dissection of the Cheek
Avoiding Facial Nerve Injury
Minimizing Postoperative Complications
Hematoma
Hemostasis
Patient Comfort
Seroma
Infection
Plastic Surgery Key
Fastest Plastic Surgery & Dermatology Insight Engine