Surface Anatomy
The eyelids provide globe protection, contribute to tear production, and distribute tears. The adjacent forehead and midface influence correct eyelid positioning. Understanding these relationships is essential in eyelid surgery.
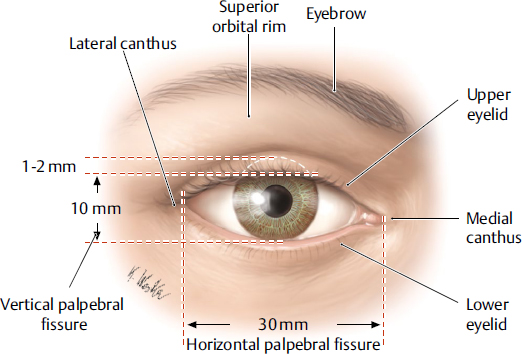
The upper and lower eyelids, along with the upper and lower puncta, oppose the globe. The upper lid naturally rests 1 to 2 mm below the superior limbus and peaks 1 mm medial to the center of the pupil. The lower lid rests at the inferior limbus and peaks 1 mm lateral to the center of the pupil. Horizontal and vertical interpalpebral fissures are about 30 mm and 10 mm, respectively. The lateral canthal angle is about 2 mm higher than the medial canthal angle. The medial canthal angle is slightly rounded compared with the sharply peaked lateral canthal angle (Fig. 15.1).
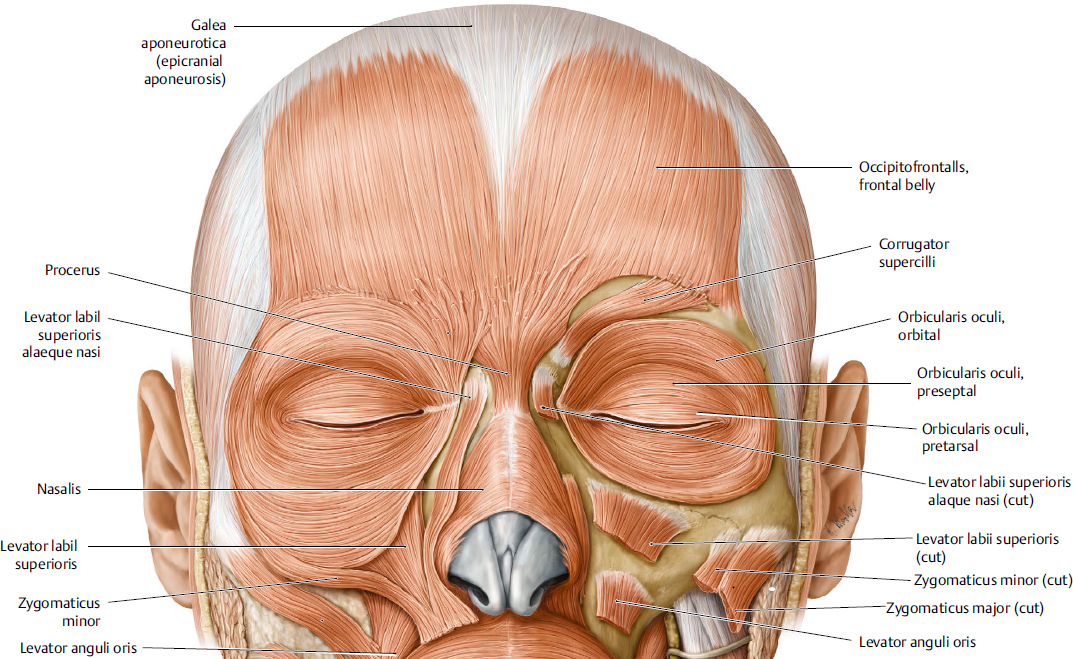
The eyebrows set above the superior orbital rim but slightly lower at the rim in males. The brow usually peaks at the lateral limbus. The forehead extends from the hairline to the glabella and superior orbital rim. The midface extends from the lower lids tapering medially to the nasolabial folds to encompass a triangular area. Facial mimetic muscles, those contributing to facial expression, influence brow position, and also cause skin furrows, including in the forehead, periorbital region, and midface.
Eyelid Anatomy
Upper Eyelid Layers
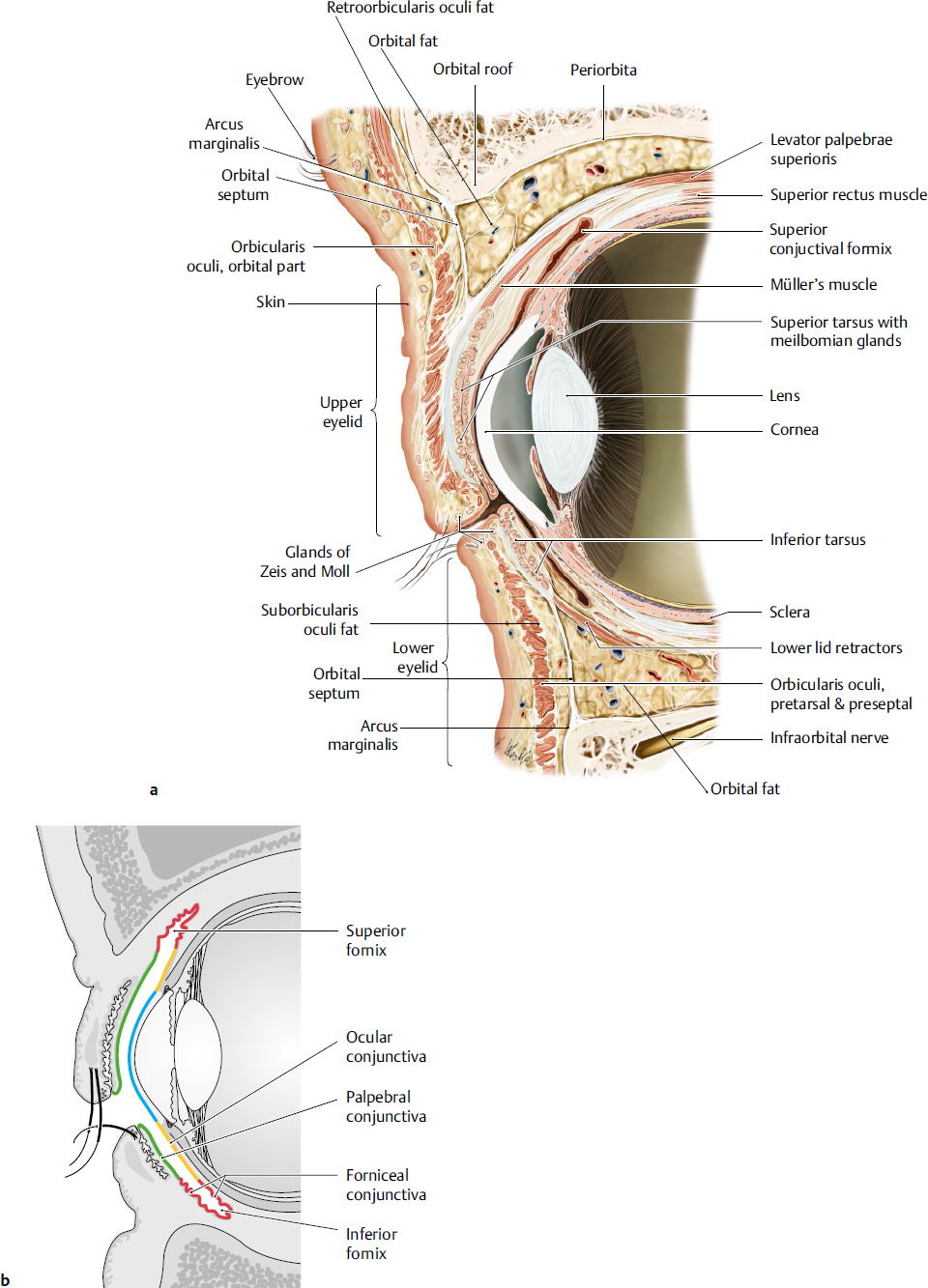
The layers of the upper eyelid vary depending on the location in the eyelid (Fig. 15.2a). Anterior to the tarsus, the structures from anterior to posterior include skin, orbicularis oculi muscle, tarsus, and conjunctiva. A few millimeters above the tarsus, structures include skin, orbicularis, orbital septum, orbital fat, levator palpebrae superioris muscle, Müller muscle, and conjunctiva. The orbital septum fuses with the levator muscle about 2 to 5 mm superior to the tarsus in non-Asians and anterior to tarsus in Asians. Orbital fat descends inferiorly to fill the space between the septum and levator, which results in a fuller lid appearance.
Lower Eyelid Layers
The layers of the lower lid are similar those of the upper except that the lid retractors consist of the capsulopalpebral fascia, analogous to the levator muscle, and the inferior tarsal muscle, analogous to Müller muscle (Fig. 15.2a).
Skin
The eyelid skin is the thinnest in the body. The lid also lacks subcutaneous tissue so the skin attaches directly to the underlying orbicularis muscle. In the upper lid, the levator muscle sends fascial attachments to the overlying orbicularis and skin to create an upper lid crease. The crease is about 10 mm or 8 to 9 mm above the lid margin in females and males, respectively. In Asians, it may be closer to the lid margin or absent. The upper lid skin is continuous with that of the thicker skin of the brow. The superior sulcus is located below the brow and tends to hollow with age.
Protractors
Orbicularis oculi muscle contraction results in eyelid closure. Its fibers are concentric around the eyelids. It is divided into the pretarsal, preseptal, and orbital regions (Fig. 15.3). The pretarsal and preseptal orbicularis are involved in involuntary blink, whereas the orbital portion is involved in voluntary lid closure. The orbicularis oculi contributes to the lacrimal pump.
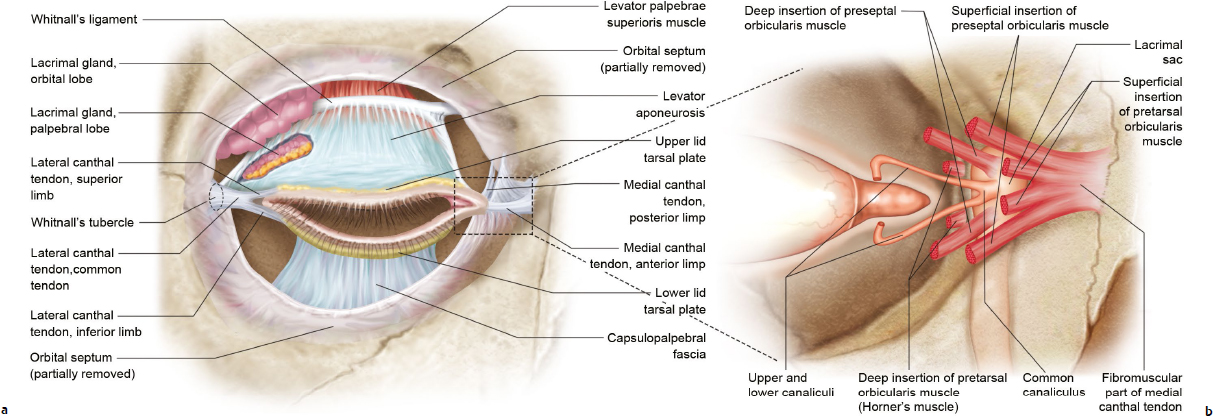
The pretarsal orbicularis oculi divides into a superficial and deep head at the medial canthus. The superficial head fuses with the medial canthal tendon (Fig. 15.4). The deep head, also known as Horner’s muscle, inserts onto the posterior lacrimal crest. Contraction pulls the lid medially and posteriorly against the globe. Laterally, the fibers from the upper and lower lids fuse into a common tendon and insert onto Whitnall’s tubercle.
The preseptal orbicularis also divides into a superficial and deep head that insert onto the medial canthus. The superficial head inserts onto the medial canthal tendon and the deep head inserts onto the lacrimal sac fascia. Laterally, the upper and lower fibers join to form the lateral palpebral raphe and connect to the underling lateral canthal tendon.
Fig. 15.1 Surface anatomy of periorbital region. Right eye, anterior view. (Modified from THIEME Atlas of Anatomy, Head and Neuroanatomy. © Thieme 2010, Illustrations by Karl Wesker.)
The orbital orbicularis arises from the medial orbital rim, broadens outward in concentric bands superiorly and inferiorly, and joins at the lateral orbital rim to form a continuous ellipse. It extends beyond the orbital rim.
Lateral and Medial Canthal Tendons
The medial canthal tendon (MCT) splits into anterior and posterior limbs, which attach to the corresponding lacrimal crest encircling the lacrimal sac (Fig. 15.4).The anterior limb of the MCT gives the lid structural support whereas the posterior limb keeps the eyelid apposed to the globe. The lateral canthal tendon is formed by superior and inferior limb that fuses to form a common tendon inserting onto Whitnall’s tubercle.
Surgical Annotation. Lateral and Medial Canthal Reanchoring
In lateral canthal anchoring (canthoplasty or canthopexy), the lid is sutured to inner aspect of the lateral orbital rim (about 10 mm posterior to the anterior rim) and slightly above the medial canthal angle. Usually the suture is secured to periosteum, but a drill hole may be helpful if the periosteal tissue is inadequate (i.e., scar). In patients with a prominent globe, the lid should be reanchored slightly more anteriorly on the inner aspect of the rim in order to avoid slipping of the lower lid under the globe.
Medial canthal tendon reanchoring or tightening of the anterior limb is to the anterior lacrimal crest. Tightening of the posterior limb presents a greater challenge given the lacrimal sac obscures access to the posterior lacrimal crest.
Orbital Septum
The orbital septum is a connective tissue structure that forms from the periosteum of the orbital rim at the arcus marginalis (Fig. 15.2a). It divides the lid into anterior (skin and orbicularis) and posterior (tarsus, conjunctiva, and lid retractors) lamella.
Orbital Fat Pads
Orbital fat, also known as preaponeurotic fat, is sandwiched between the septum and the lid retractors. As discussed in Chapter 14, there is a medial and central fat pad in the upper lid and a medial, central, and lateral fat pad in the lower lid. These fat pads can atrophy with age, creating a hollowed superior or inferior sulcus or a bulge behind a weakened septum, causing orbital fat prolapse and bulging.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree