Extensor Tendon Surgery
Mark E. Puhaindran
INTRODUCTION
The extensor system is complex and intricate. A fine balance exists between the long extensors, innervated by the radial nerve, and the intrinsic muscles of the hand, innervated by the median and ulnar nerves. The superficial location on the dorsum of the hand makes the extensor system vulnerable to injury. Because small variations in tendon length and tension result in significant functional deficits, outcomes of treatment may be suboptimal.
The purpose of this chapter is to review the anatomy of the extensor system and the surgical management and rehabilitation of commonly encountered injuries and conditions that affect the extensor system.
ANATOMY
There are 12 extensor muscles, all of which are innervated by the radial nerve directly or its terminal motor branch, the posterior interosseous nerve (PIN). The brachioradialis, anconeus, and extensor carpi radialis longus (ECRL) are innervated by the radial nerve. The extensor carpi radialis brevis (ECRB) innervation may arise from the radial nerve or the PIN. All other extensor muscles are innervated by the PIN. The most distally innervated muscle is the extensor indicis proprius (EIP).1 The brachioradialis, ECRL, and ECRB muscles originate from the lateral supracondylar ridge and epicondyle of the distal humerus, and from the mobile wad of muscles in the proximal forearm. The extensor digitorum communis (EDC), extensor digiti minimi (EDM), extensor carpi ulnaris (ECU), and anconeus originate from the common extensor origin at the lateral epicondyle of the humerus, and the other muscles originate more distally in the forearm. The extensor muscles are arranged in two layers, superficial and deep, within the forearm—the anconeus, ECRL, ECRB, EDC, EDM, and ECU form the superficial layer. The deep layer consists of the supinator, abductor pollicis longus (APL), extensor pollicis brevis (EPB), extensor pollicis longus (EPL), and EIP.2
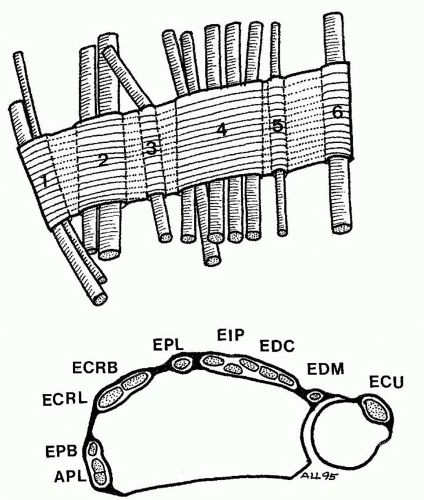
At the wrist, the tendons of the extensor muscles run under the extensor retinaculum and are separated into six compartments (five fibro-osseous and one fibrous). The first compartment contains the APL and EPB tendons and the second contains the ECRL and ECRB tendons. The EPL winds around Lister tubercle and occupies the third extensor compartment. The EDC and EIP tendons run in the fourth compartment, the EDM runs in the fifth compartment—the only fibrous compartment—and the ECU runs in the sixth compartment (Figure 78.1).3
Over the dorsum of the hand, there are bands, the juncturae tendinae, that connect the ring EDC tendon to the EDC of the middle and small fingers, as well as from the middle to the index finger.4 The EIP and EDM tendons lie ulnar to their respective EDC tendons and insert at the level of the metacarpophalangeal joint (MCPJ).
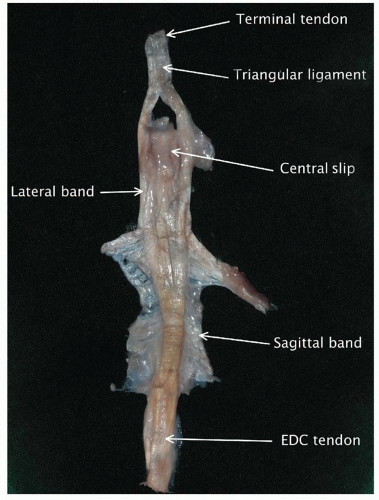
At the MCPJ, the extensor tendon is held in position by the sagittal bands, a sling that arises from the volar plate of the MCPJ and intermetacarpal ligaments.5 These bands facilitate extension of the MCPJ through a lasso effect around the base of the proximal phalanx. The extensor tendon becomes broad and thin over the dorsum of the proximal phalanx where the EDC tendon trifurcates, with the central portion becoming the central slip that inserts into the base of the middle phalanx, and the lateral portions joining the tendons of the interosseous muscles and lumbricals to form the lateral bands (Figure 78.2). These lateral bands come together over the middle phalanx and form the most distal part of the extensor tendon that inserts into the base of the distal phalanx.6 The lateral bands translate in a palmar-dorsal direction relative to the axis of rotation during proximal interphalangeal joint (PIPJ) flexion and extension and are prevented from subluxation in a dorsal direction by the transverse retinacular ligament (TRL), or in a volar direction by the triangular ligament, found over the dorsum of the middle phalanx. The oblique retinacular ligaments, originally described by Landsmeer,7 originate from the distal aspect of the second annular pulley and travel obliquely and insert into the extensor tendon over the middle of the distal phalanx. They are not easily identified in all digits and help coordinate extension in between the PIPJ and DIPJ (distal interphalangeal joint).
Many variations to the classic anatomy of the extensor system are found.8 Examples include the presence of accessory muscles like the extensor carpi radialis intermedius and extensor medii proprius, which are present in 10% of hands.9 Variations exist in the number of EDC slips to the digits and anatomy of the juncturae tendinae over the dorsum of the hand.8 There is also variation within the EDC muscle, which has been described to have a common muscle belly. Intramuscular branching of the nerve in the muscle may occur,10 and this allows independent index finger extension following EIP harvest for tendon transfer.
EXTENSOR TENDON INJURIES
Finger extension is achieved through a balance of two separate systems—the radial nerve innervated extrinsic extensors and the intrinsic muscles, innervated predominantly by the ulnar nerve, with some contribution from the median nerve. Distal to the MCPJ, the extensor tendon is thin, making core repairs difficult. Furthermore, there is a precise balance between the various components of the tendon during movement, which is difficult to restore following injury.6 Although there is more excursion of the tendon at the level of the wrist, there is minimal excursion at the level of the PIPJ and DIPJ, with 0.6 mm of excursion for every 10° of movement at the DIPJ; hence, tendon shortening at this level from tendon repair will result in significant loss of movement.11
Extensor tendon injuries are classified based on eight anatomical zones described by Kleinert and Verdan.12 Odd numbered zones are located over the joints, whereas even numbered zones are found in between (i.e., zone 1 lies over the DIPJ, zone 3 over the PIPJ, zone 5 over the MCPJ, etc.) (Figure 78.3). In the thumb, the interphalangeal joint (IPJ) is zone 1 and MCPJ is zone 3.
Several difficulties and pitfalls in the clinical assessment of patients with acute extensor tendon injuries are highlighted:
Juncturae tendinae—Digit extension at the MCPJ may still be possible after complete EDC laceration because of the variable interconnections between the EDC tendons over zone 6.8 This has to be taken into account when assessing patients with dorsal hand lacerations. Surgical exploration is frequently the best way to determine if the EDC tendon has been cut.
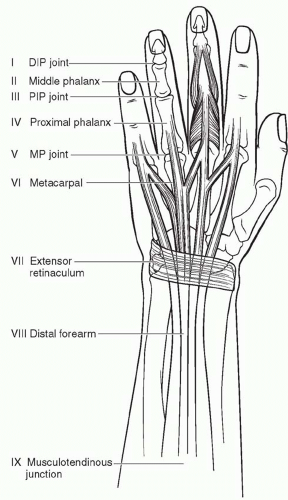
FIGURE 78.3. Zones of injury for the extensor system. DIP, distal interphalangeal; PIP, proximal interphalangeal; MP, metacarpophalangeal.
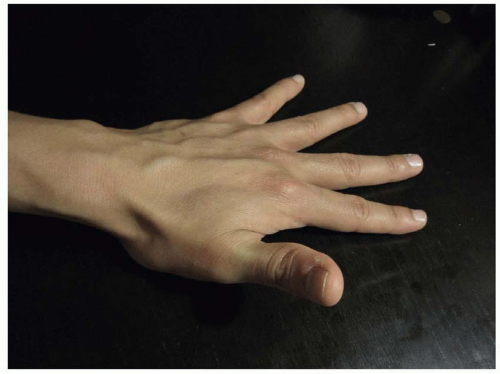
Testing for the EPL—The EPL tendon functions mainly to extend the IPJ of the thumb. It also extends the MCPJ (together with the EPB) and the carpometacarpal joint (together with the APL), and it adducts the thumb toward the palm when the thumb is in full extension. However, the EPB, APB, and FPB can also cause IPJ extension due to their insertion on the extensor apparatus. Hence, the best way to assess for EPL function to ask the patient to lift the thumb up while the palm placed flat on a table (Figure 78.4).
Testing for a closed central slip rupture—This test was first described by Elson.13 The PIPJ of the patient is maximally flexed by the examiner and the patient asked to extend the PIPJ while the examiner resists (Figure 78.5). Should the central slip be ruptured, minimal extension power is felt at the PIPJ while more power is felt at the DIPJ because of the force generated through the intact lateral bands.
MANAGEMENT OF ACUTE EXTENSOR TENDON INJURIES
Zone 1 Injuries
Injuries over the DIPJ (zone 1 injuries) have been classified into four types by Doyle (Table 78.1).14 Type I or closed injuries are the most common and can be treated by splinting the DIPJ in extension for 6 to 8 weeks, followed by night splinting for another 6 weeks. Patients presenting a few months after injury can still be treated using this technique.15 Alternatively, the joint can be splinted internally using a Kirschner wire for patients who cannot tolerate an external splint or for patients who must continue working, such as a surgeon. Patients are advised to continue moving the PIPJ while the DIPJ is splinted. Long-term, slight extensor lag of 10° is to be expected following conservative treatment, and patients are counseled about this limitation at the start of treatment.16 A similar splinting protocol can also be used for patients with closed thumb mallet injuries.17
TABLE 78.1 CLASSIFICATION OF MALLET FINGER DEFORMITIES | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree