CHAPTER 3 Evaluation of the Cosmetic Oculoplastic Surgery Patient
The preoperative evaluation of the candidate for cosmetic oculoplastic surgery is extremely important and cannot be overemphasized. In addition to helping determine the specific procedures required by the patient, evaluation aids in selecting candidates for surgery. Moreover, the initial visit provides a setting in which to prepare patients for surgery and to inform them about its possible complications, thereby ensuring a smoother postoperative course.
One of the most important aspects of evaluation is to establish what patients find objectionable in their appearance and what they expect surgery to accomplish. I usually determine this by handing patients a mirror and asking them to hold it at eye level as they point out their objectionable features (Fig. 3-1). Frequently, patients emphasize their most minor blemishes and dismiss the major defects noted by the surgeon. The surgeon should therefore make sure that the patient has realistic expectations.
History
In taking a medical history, the surgeon questions the patient about illnesses, medications, allergies, and edema. Emphasis is on ruling out thyroid disease, heart failure, hypertension, bleeding tendencies, and unusual edema. For example, patients with thyroid disease may look as if they need cosmetic surgery, but the treatment needed is frequently medical, not surgical. Also, patients with thyroid disease must be followed up for at least 6 months until their eyelid retraction measurements and amounts of eyelid edema and herniated fat are stable before surgery can be considered. Patients should also be questioned about intake of aspirin or anti-inflammatory medications, such as ibuprofen, vitamin E, anticoagulants and herbal remedies. These drugs must be discontinued for several weeks pre-operatively to avoid the possibility of complications of bleeding during and after surgery.
Forehead and eyebrow examination
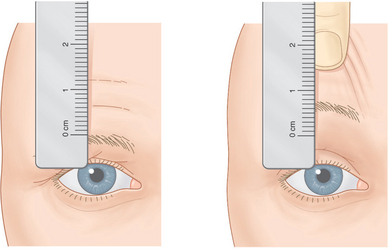
The amount of brow ptosis can be determined in several ways. The first is to line the zero mark of a millimeter ruler with the central superior brow edge (Fig. 3-2). The brow is then elevated to a cosmetically acceptable level with the examiner’s finger, and the amount of excursion of the brow is noted on the ruler where the superior central brow edge meets the ruler. This measurement is repeated over the temporal and nasal aspects of the brow about 10 mm from the brow ends, and similar measurements are made over the opposite brow.
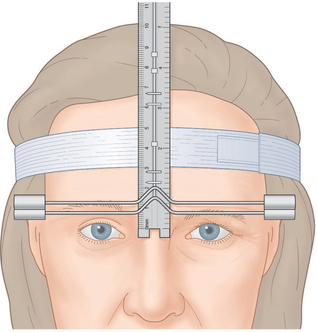
Still another method of measuring brow ptosis or asymmetry is to use the ocular asymmetry measuring device (Bausch & Lomb Storz® Instruments),1 an instrument that Chalfin and I devised. It consists of a headband, a ruler, and a T-shaped crosspiece. When the band is placed around the patient’s forehead, it fixes the ruler vertically over the midforehead. The crosspiece line intersects the medial canthus and levels the crosspiece. The crosspiece is then aligned with the central superior brow, and the location where the indicator is positioned on the ruler is noted (Fig. 3-3). The brow is elevated with the examiner’s finger to a cosmetically acceptable level. The crosspiece is then elevated to the new superior central brow position, and the excursion of the indicator on the ruler is noted. The measurements are repeated temporally and nasally and on the opposite brow.
Examination of the upper eyelid
Eyelid crease examination
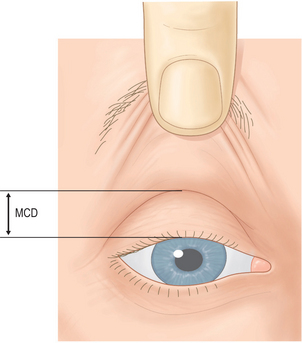
The examiner can find the upper eyelid crease by lifting the eyebrow and asking the patient to look downward first, then slightly upward, and then downward again. The distance from the central upper eyelid margin to the central crease as the patient looks down and as the eyelid fold is elevated with the examiner’s finger determines the margin crease distance (MCD) measurement described by Urist and me (Fig. 3-4). Normally, this is 9–11 mm. If the distance is much less, reconstruction of the eyelid crease and excision of the skin fat should be considered (see Chapter 7). If the MCD is much greater than normal, a disinsertion of the levator aponeurosis should be suspected. As the levator aponeurosis recesses into the orbit, it frequently elevates the eyelid crease upward.
To predetermine the position at which to reconstruct an upper eyelid crease, the surgeon will need a curved instrument for compression of the upper eyelid skin. I formerly used an unwound, slightly curved paper clip and pressed it at various positions of the upper eyelid. Many of my patients reacted negatively to the use of a paper clip to determine the eyelid crease, saying how crude an instrument it was. This negative reaction led to my development of a more sophisticated instrument, the upper eyelid creaser (Bausch & Lomb Storz® Instruments).2
This creaser consists of a 4-cm, curved, thin metal wire attached to a handle (Fig. 3-5). The wire has a curvature similar to the normal upper eyelid crease, but it is flexible and can be bent by the examiner if the curve needs to be flattened or extended. The examiner holds the handle and presses the wire into the upper eyelid at various positions until the surgeon and patient agree on a desirable level at which the reconstruction is to be performed (Fig. 3-6). A measurement is made between the upper eyelid margin and the chosen position and is used intraoperatively to determine the position for reconstructing the crease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree