I. FACTORS CONTRIBUTING TO FACIAL AGING
A. Sun damage (photoaging): Atrophy, loss of skin tone, and pigmentation changes
B. Significant weight gain or loss. Increased facial fat deposits will confer a more youthful appearance.
C. Chronic use of alcohol and/or cigarettes
D. Chronic medical conditions such as diabetes and renal failure
E. History of facial trauma
F. Facial paralysis. The paralyzed side develops fewer deep wrinkles, but becomes more ptotic compared to the normal side.
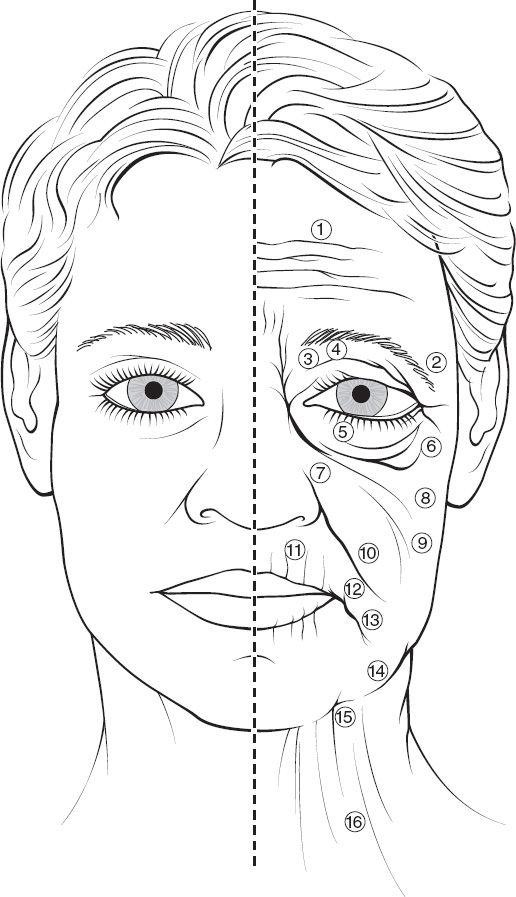
II. CHANGES IN FACIAL APPEARANCE WITH AGING (Fig. 31-1)
A. Skin changes
1. Decrease in dermal thickness (especially reticular dermis), loss of elasticity, and reduction in dermal appendages cause fine rhytides
2. Hyperpigmentation, keratoses, and papules
3. Decreased amount of subcutaneous adipose tissue
4. The total amount of collagen in skin decreases, and the proportion of collagen type III increases
5. Larger sebaceous glands
B. Soft tissue changes
1. Overall loss of volume, most pronounced in middle and upper third
2. Progressive laxity of the retaining ligaments of the face
3. Irregularities and facial creases occur from a juxtaposition of lax tissues with fixed ligaments (e.g., nasojugal groove and jowls)
C. Facial skeletal changes
1. Loss of bone mass in infraorbital rim and anterior maxilla contributes to decreased mid and lower facial height
2. Loss of dentition further decreases alveolar bone and causes loss of lower facial height
3. The orbit expands inferolaterally and superiomedially with increasing age
4. Increased prominence of the chin, supraorbital rim, and zygomatic arch
D. Perioral changes
1. Vertical rhytides extend radially out from the upper and lower lip margins
2. Decreased fullness and flattening of the upper lip. There is about 1 mm loss of incisor with each decade of age due to gravity.
3. Downturning of the oral commissures
4. Deepening of the nasolabial folds and formation of marionette lines around the chin
E. Cervical changes
1. Skin laxity and wrinkling
2. Formation of vertical platysmal bands from diastasis of the platysma muscles
3. With laxity and increase in submental fat, a more obtuse cervicomental angle develops.
4. Ptosis of the submandibular glands
______________
*Denotes common in-service examination topics
Figure 31-1. Aging changes in the face. 1. Forehead and glabella creases. 2. Ptosis of the lateral brow. 3. Redundant upper eyelid skin. 4. Hollowing of the upper orbit. 5. Lower eyelid laxity and wrinkles. 6. Lower eyelid bags. 7. Deepening of the nasojugal groove. 8. Ptosis of the malar tissues. 9. Generalized skin laxity. 10. Deepening of the nasolabial folds. 11. Perioral wrinkles. 12. Downturn of oral commisures. 13. Deepening of labiomental crease. 14. Jowls. 15. Loss of neck definition and excess fat in neck. 16. Platysmal bands.
F. Periocular changes
1. Dermatochalasis: Excess and laxity of eyelid skin
2. Eyelid edema and hyperpigmentation
3. Protrusion of the periorbital fat due to laxity of the obital septum
4. Ptosis of the lacrimal glands
5. Ptosis of the eyelid due to attenuation of the levator aponeurosis
III. PRINCIPLES OF FACIAL REJUVENATION
A. Improve the quality of the skin with chemical peels, laser, and dermabrasion (see on nonsurgical treatment of facial aging)
B. Address the loss of volume (both soft tissue and bone) with fillers, bone, or skeletal implants
C. Return tissues to their original anatomical place (i.e., lift what has fallen and tighten what has become lax)
D. Excise redundant tissue (e.g., facial skin and orbital fat)
IV. FACELIFT (RHYTIDECTOMY)
A. Anatomy
1. Soft tissue of the face is constructed in concentric circles around the cavities of the facial skeleton (the orbits and oral cavity).
2. The areas of fixation such as the mandibular, zygomatic, and orbicularis retaining ligaments contrast with the areas of laxity in these areas to cause jowling and deepening of the nasojugal groove.
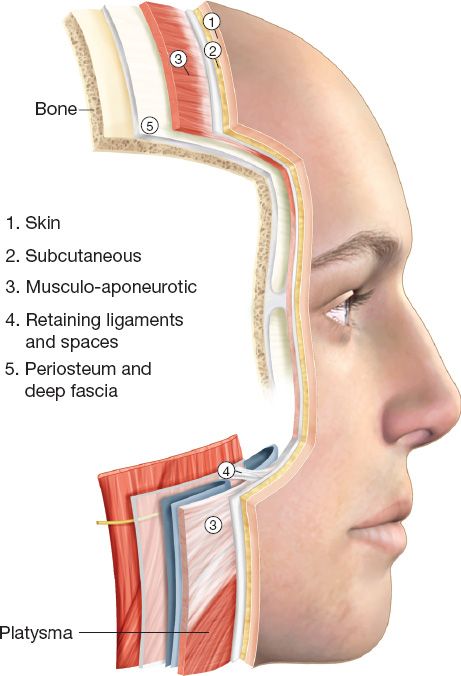
3. Layers of the face (Fig. 31-2): Skin, subcutaneous fat, superficial musculoaponeurotic system (SMAS), and deep facial fascia (parotidomasseteric fascia). In the cheek, the facial nerve, parotid duct and buccal fat pad are all deep to the parotidomasseteric fascia.
Figure 31-2. The five layers of the face, analogous to layers of the scalp and neck. The facial nerve travels deep to or within the SMAS layer.
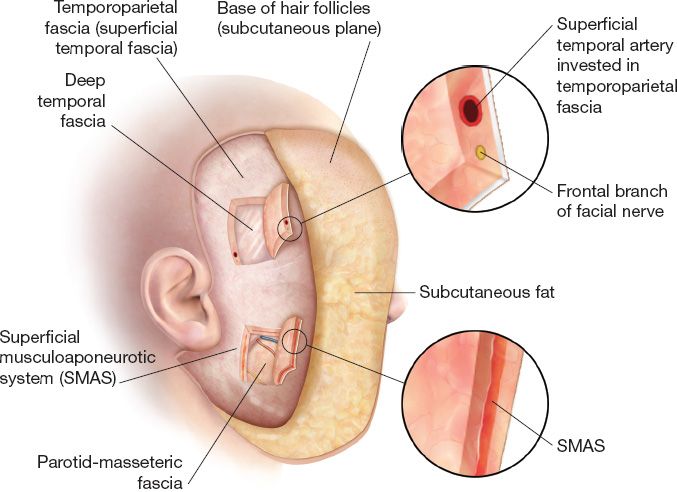
4. SMAS: Term coined by Tessier (Fig. 31-3)
a. *Thin fascial layer that invests the superficial mimetic muscles and separates the overlying subcutaneous fat from the underlying parotidomasseteric fascia.
b. Continuous with the galea, the superficial temporal fascia (temporoparietal facia), superficial cervical fascia, and the platysma
5. Mimetic muscles: Four layers from superficial to deep
a. Depressor anguli oris, zygomaticus minor, and orbicularis oris
b. Depressor labii inferioris, risorius, platysma (innervated by cervical branch of facial nerve)
c. Zygomaticus major, levator labii superioris alaeque nasi
d. *Deep muscles (innervated on their superficial surface): Levator anguli oris, buccinator, and mentalis
6. Parotidomasseteric fascia
a. Continuous with the deep layer of cervical fascia.
b. Facial nerve branches within the cheek lie just deep to this layer laterally and become more superficial medially.
c. Loré fascia (also known as tympanoparotid fascia, platysma-auricular ligament, and parotid-cutaneous ligament) is an area of dense fibrous tissue in front of the earlobe. Some techniques place anchoring sutures here.
7. Temporal region
a. Three fascial layers: Temporoparietal fascia, superficial layer of deep temporal fascia, and deep layer of deep temporal fascia
b. Superficial and deep layers of deep temporal fasica separated by superficial temporal fat pad
Figure 31-3. The superficial musculo-aponeurotic system (SMAS). The SMAS is continuous with the temporoparietal fascia (superficial temporal fascia). Within the temporoparietal fascia runs the superficial temporal artery and the frontal branch of the facial nerve.
a. Primarily from branches of external carotid
i. Anterior: Facial, labial, supratrochlear, and supraorbital
ii. Lateral: Submental, zygomatico-orbital, and anterior auricular
iii. Forehead and scalp: Occipital, superficial temporal, and posterior auricular
b. Rhytidectomy divides fasciocutaneous perforators from lateral facial arteries leaving flap dependent on medially based musculocutaneous perforators.
9. Facial nerve (CN VII)
a. The deep and superficial lobes of the parotid gland are separated by the trunks of the facial nerve.
b. Branches exit the parotid anteriorly and travel along the superficial surface of the masseter, deep to the parotidomasseteric fascia.
c. Anterior and medial to the masseter, the nerve branches lie over the buccal fat pad
d. Branches penetrate the parotidomasseteric fascia to innervate the overlying mimetic muscles.
e. Once the frontal branch crosses the zygomatic arch (crosses midway between tragus and lateral canthus), it comes to lie within or just deep to the SMAS (temporoparietal fascia). It is here that the nerve is most susceptible to injury during a rhytidectomy.
f. Most of the facial muscles lie superficial to the plane of the facial nerve and receive their innervation from their deep surfaces. However,*the muscles innervated from their superficial surface are the buccinator, levator anguli oris, and mentalis muscles.
g. *The marginal mandibular nerve
i. Exits the parotid 4 cm below the base of the earlobe just anterior to the angle of the mandible.
ii. In most cases (81%), the nerve courses above the mandibular border. It runs superficial to the facial artery and vein and can be identified where the facial vessels cross the mandibular border, just anterior to the insertion of the masseter.
iii. Innervates: Depressor anguli oris, mentalis, depressor labii inferioris, and part of risorius and orbicularis oris
h. Buccal and zygomatic branches
i. Rarely symptomatic injury long term due to multiple interconnections
ii. Branches deep to SMAS
10. Great auricular nerve (C2–C3)
a. *Crosses at the midportion of the sternocleidomastoid muscle 6.5 cm below the external auditory canal.
b. *Courses in the same plane as the external jugular vein, which is a useful landmark during dissection.
c. *Most commonly injured symptomatic nerve during rhytidectomy.
d. Division of nerve causes numbness of posterior ear
11. Auriculotemporal nerve
a. Runs with superficial temporal artery
b. *Division during facelift can cause Frey’s syndrome where facial skin receives sympathetic reinnvervation causing gustatory sweating.
B. Indications and patient assessment
1. Address the specific complaints of each patient and tailor the operative plan individually.
2. The rhytidectomy preoperative evaluation includes assessment and documentation of facial asymmetries as well as skin redundancy, abnormal fat accumulations, platysma laxity, and salivary gland laxity.
3. The contour of the jawline and neckline and the status of the nasolabial folds are evaluated.
1. Subcutaneous rhytidectomy
a. Described in early 20th century, the first facelift was skin excised anterior to the ear and temporal hairline. With evolution of this technique, operations involved more extensive undermining of skin.
b. Relies on skin tension to tighten the underlying soft tissues, which can cause skin necrosis, widened scars, and facial distortion.
c. Although surpassed by the following techniques, it still may be useful in thin patients with skin-only excess and without ptosis of deeper structures.
2. Deep subcutaneous rhytidectomy
a. Flaps are raised in plane immediately superficial to SMAS, bringing fat up with the skin flap, which is then contoured.
b. Benefits include a more robust flap and a reduction in risk of facial nerve damage by leaving the SMAS down.
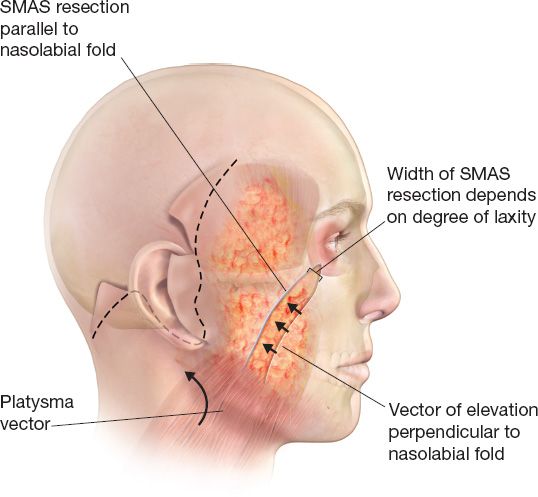
3. Subcutaneous rhytidectomy with SMAS plication or resection
a. This is the standard facelift for many plastic surgeons and there are many personalized variations.
b. The incision is begun just at or 1 cm posterior to the temporal hairline, continued down in front of the ear (either pretragally or retrotragally) around the base of the lobule, and then upward and posterior around the back of the ear to finish in the postauricular scalp
c. *Beveling the temporal incision cuts across the hair shaft perpendicularly which promotes hair growth through the scar.
d. Preauricular incision: Made along anterior border of helix to tragus and then along posterior border of tragus.
e. Postauricular incision: Retroauricular sulcus with higher extension of the incision for less severe laxity.
f. Skin flap dissection is performed in a lateral-to-medial direction, leaving a small layer of fat on the flap. Dissection ends just lateral to the nasolabial folds.
g. Either the SMAS is plicated or a narrow ellipse is excised. The direction of pull should be superior and lateral across the midface parallel to the nasolabial fold.
h. The main advantage of this technique is the ability to manipulate the skin and SMAS separately, so that the SMAS can be repositioned vertically and skin can be re-draped laterally with minimal tension (Fig. 31-4)
4. Minimal access cranial suspension (MACS) lift
a. *Preauricular and pretemporal incisions. The SMAS is elevated in a vertical vector with purse-string sutures that are then anchored to the deep temporal fascia.
b. The skin incision is similar to that described above but without the extension to the postauricular scalp.
5. Deep-plane rhytidectomy
a. Described by Tord Skoog, this is a reliable technique to specifically address deep nasolabial folds.
b. A sub-SMAS dissection is extended over the zygomaticus muscles and medially beyond the nasolabial folds, totally releasing all SMAS attachments and creating a thick flap composed of skin, subcutaneous fat, and platysma
c. The total release of the SMAS allows all components of the flap to be lifted and advanced back to their original position.
d. The correct plane is below the SMAS and just above the thin parotidomasseteric fascia, which serves to protect the branches of the facial nerve.
e. Expectedly, the deep-plane technique is associated with a slightly higher risk of facial nerve injury.
6. Minimal incision rhytidectomy with lateral SMASectomy
a. A facial rejuvenation technique that minimizes retroauricular incisions; the attempt is to avoid retroauricular skin flap ischemia.
b. Ideal candidates are usually relatively young (40s) with aging primarily in the midface and lower face with moderate jowls.
c. A standard incision is utilized with a truncated postauricular extension
Figure 31-4. Rhytidectomy with SMAS excision or plication. The SMAS and facial fat are repositioned in an upward manner, while the skin is re-draped in a more posterior direction.
d. Skin flaps are elevated in the standard fashion
e. The SMAS flap is created by incising along the medial edge of the parotid
f. A tongue of inferiorly based SMAS is created and then sutured to the mastoid fascia to achieve the desired pull (perpendicular to the nasolabial folds).
7. Subperiosteal rhytidectomy
a. Developed by Tessier, this extensive approach can specifically address structural laxity in the midface.
b. Complications include an increased incidence of facial nerve injuries as well as prolonged facial edema.
c. This procedure may be performed in patients with significant facial aging and extensive ptosis of the central area of the face, including the eyebrows, nasoglabellar soft tissue, nose, nasolabial folds, cheeks, angle of the mouth, and jowls.
d. The operative technique involves degloving of the upper face and midface and elevation of tissues in the subperiosteal plane.
8. Midface lift (concentric malar lift)
a. This technique directly addresses ptosis of the malar fat pad through a lower lid blepharoplasty incision (either subciliary or transconjunctival).
b. Wide subperiosteal dissection over the anterior maxilla from the level of the inferorbital rim is performed.
c. The infraorbital nerve is carefully preserved.
d. The periosteum is released, allowing repositioning and fixation of the cheek mass to the infraorbital rim or the temporalis fascia.
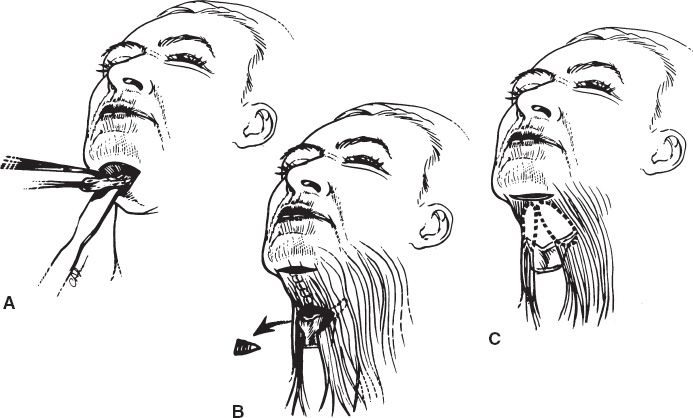
9. Neck lift (Fig. 31-5)
a. Corrects cervicomental obliquity and platysmal banding.
b. Supra- and subplatysmal fat is removed by either liposuction or direct excision.
c. The platysma can be tightened by plicating it in the midline (with or without transecting it inferolaterally), or pulling the platysma superiolaterally and fixating to Loré fascia.
Figure 31-5. Treatment of medial platysma and platysma bands. Alternatives include A: defatting of the anterior platysma without muscle modification; B: midline platysmaplasty with wedge excision and plastymal plication; C: resection of platysmal bands without midline approximation. If a submental incision is elected, option (B) is usually the best alternative.
i. Make incision just posterior to submental crease.
ii. Subcutaneous and interplatysmal fat can be excised.
D. Complications of rhytidectomy
1. Hematoma
a. Most common complication and accounts for 70% of all rhytidectomy complications
b. More common in men than in women
c. More common in secondary rhytidectomy
d. Must be evacuated to prevent overlying skin necrosis and scarring
e. *Perioperatiave blood pressure control and avoidance of substances that can interfere with clotting mechanisms (e.g., aspirin and NSAIDS) are the most important preventative measures.
2. Flap loss and/or ischemia, most commonly affecting smokers
3. Infection is a rare complication (<1%)
4. Asymmetry: this should be addressed prior to surgery
5. Great auricular nerve injury
a. *Presents as numbness of the lower ear and earlobe
b. If inadvertent transection is identified intraoperatively, the nerve should be repaired and good sensory results expected.
6. Facial nerve injury and palsy
a. The most commonly injured branch of the facial nerve is the buccal branch. However, injury is frequently unrecognized due to overlap of innervation with other facial nerve branches.
b. *Injury to a cervical branch can mimic injury to the marginal mandibular branch producing lower lip depressor weakness. However, patients with a marginal mandibular nerve injury cannot purse their lower lip (mentalis and orbicularis function).
c. Spontaneous recovery expected in 80% of patients because most injuries are due to neuropraxia or stretch. Re-exploration in the early postoperative period is rarely described, but in individual cases may be warranted if the index of suspicion for a transection is exceedingly high.
7. Excessive scarring or temporal alopecia
8. Pixie ear deformity refers to a lobule that has been pulled inferiorly and anteriorly, caused by insetting the lobule under tension
V. FACIAL AUGMENTATION AND FACIAL IMPLANTS
A. The chin is the most commonly augmented site, followed by the malar region.
B. *Augmentation is useful in combination with rhytidectomy to compensate for soft tissue and bony atrophy that occurs with aging.
C. Alloplastic materials
1. Silicone
a. The most commonly used material because it is biocompatible, stable, and the shape can be easily modified.
b. Silicone implants become encased by a tissue capsule and can be easily removed if necessary.
2. Polyethylene (Medpor)
a. Used for rigid skeletal augmentation.
b. Available in a variety of shapes to augment the orbital rim, malar area, piriform, mandibular angle, chin, and nasal dorsum.
c. Polyethylene is porous and allows tissue ingrowth with a theoretical advantage of fewer complications from infection, extrusion, and malposition.
d. For this reason, polyethylene is more difficult to remove than silicone.
3. Hydroxyapatite: Used for cranial reconstruction, alveolar ridges, and other bony facial structures
D. *The ratio of soft tissue response to facial skeletal change is approximately 0.66. For example, an implant with 1 cm of projection will usually result in 0.66 cm of soft tissue augmentation projection. In general, chin implants usually provide more reliable projection than malar implants due to their location and surrounding soft tissue contour.
E. Chin implants are placed subperiosteally via intraoral or submental approaches.
F. Common complications include hematoma, lower lip dysfunction (mentalis injury), infection, extrusion, malposition, and mental nerve injury.
PEARLS
1. Change to the facial skeleton with aging include decrease in height of the midface and lower face, increased prominence of the chin, increased prominence of the zygomatic arch, and increased facial depth. These changes must be considered when altering the soft tissue envelope during facelift surgery.
2. Preoperative photographs are invaluable during surgical planning, patient discussion, postoperative counseling, and documentation for medicolegal purposes
3. Patients should be informed that the effects of facelifts are considered to last for about 10 years, although this is depend on many factors, such as the age at which the procedure is performed and the general health status of the patient
4. Ehlers–Danlos syndrome is a rare genetic connective tissue condition typified by atrophic, thin, hyperextensible, friable skin, and hypermobile joints. Cosmetic surgery is not indicated.
5. Cutis laxa is a condition that causes degeneration of elastic fibers in the dermis and is associated with pulmonary sequelae and hernias. Cosmetic surgery is feasible in this population but recurrence of laxity is likely.
QUESTIONS YOU WILL BE ASKED
1. Which muscles are innervated on their superficial surface?
Levator anguli oris, buccinators, and mentalis muscles.
2. What is the SMAS?
Superficial musculo-aponeurotic system, a thin fascial layer investing the mimetic muscles of the face.
3. What is the most commonly injured branch of the facial nerve?
Buccal.
4. What is the most common symptomatic nerve injury?
Great auricular nerve.
5. What complication do you expect when operating on a smoker?
Skin flap necrosis.
6. How do you avoid a pixie ear deformity?
Tension-free inset of the lobule.
Recommended Readings
Agarwal CA, Mendenhall SD 3rd, Foreman KB, Owsley JQ. The course of the frontal branch of the facial nerve in relation to fascial planes: an anatomic study. Plast Reconstr Surg. 2010;125(2): 532–537. PMID: 20124839.
Baker DC. Minimal incision rhytidectomy (short scar face lift) with lateral SMASectomy. Aesthet Surg J. 2001;21(1):68–79. PMID: 19331876.
Baker DC, Conley J. Avoiding facial nerve injuries in rhytidectomy. Anatomical variations and pitfalls. Plast Reconstr Surg. 1979;64(6):781–795. PMID: 515227.
Feldman JJ. Corset platysmaplasty. Plast Reconstr Surg. 1990;85(3):333–343. PMID: 2304983.
Hester TR Jr, Codner MA, McCord CD, Nahai F, Giannopoulos A. Evolution of technique of the direct transblepharoplasty approach for the correction of lower lid and midfacial aging: maximizing results and minimizing complications in a 5-year experience. Plast Reconstr Surg. 2000;105(1):393–406; discussion 407–408. PMID: 10627009.
Mitz V, Peyronie M. The superficial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plast Reconstr Surg. 1976;58(1):80–88. PMID: 935283.
Shaw RB Jr, Katzel EB, Koltz PF, et al. Aging of the facial skeleton: aesthetic implications and rejuvenation strategies. Plast Reconstr Surg. 2011;127(1):374–383. PMID: 20871486.
Yaremchuk MJ, Kahn DM. Periorbital skeletal augmentation to improve blepharoplasty and midfacial results. Plast Reconstr Surg. 2009;124(6):2151–2160. PMID: 19952674.
< div class='tao-gold-member'>