Fig. 25.1
Endoscopic view of left middle meatus. Thin arrow pointing to the uncinate process; thick arrow pointing to the bulla ethmoidalis (With permission Andrew N. Goldberg, MD, MSCE, FACS)
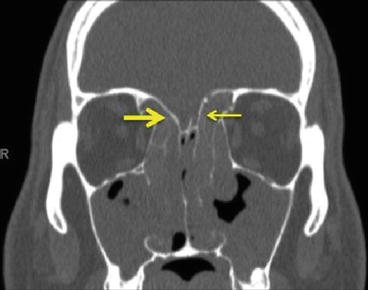
Fig. 25.2
Coronal CT demonstrating slope variation of the fovea ethmoidalis. Note the more steeply oriented left fovea (thin arrow) as compared to the right fovea (thick arrow) (With permission Andrew N. Goldberg, MD, MSCE, FACS)
In part due to differing drainage pathways, the ethmoid sinus is subdivided into anterior and posterior groups. The separation of the anterior and posterior ethmoids is the middle turbinate attachment to the lateral nasal wall, also known as the basal lamella. Anteriorly, cells drain into the middle meatus; posteriorly, drainage occurs into the superior meatus.
Variations of air cell anatomy exist throughout the paranasal sinuses. One variant unique to the ethmoid sinus is the Haller cell, described as an infraorbital cell that may cause narrowing of the infundibulum and maxillary sinus ostium. This cell can originate from either the anterior or posterior ethmoid group. A sphenoethmoidal air cell, or Onodi cell, is a posterior ethmoid air cell that aerates the optic nerve and typically extends superior or superior/lateral to the sphenoid sinus. Ethmoid air cells may also be found in a supraorbital location extending into the frontal bone.
Arterial supply to the ethmoid mucosa is primarily from the anterior and posterior ethmoid arteries. These are located in a septation of bone traversing lateral to medial from the orbit across the roof of the ethmoid sinus. Anterior and posterior ethmoidal nerves, arising from the nasociliary nerve, and parasympathetic branches of the pterygopalatine ganglion provide sensory innervation to the ethmoid sinus mucosa. On a coronal CT scan, the anterior and posterior ethmoid arteries can be identified medially and superiorly in the orbit, exiting the orbit medially from a pinch in the bone (Fig. 25.3). The anterior ethmoid artery can also be identified approximately 24 mm posterior to the anterior lacrimal crest roughly corresponding with the posterior end of the globe and is usually associated with the basal lamella. The posterior ethmoid artery is located an additional 12 mm posterior to the exit of the anterior ethmoid artery and is associated with the anterior face of the sphenoid sinus. Both arteries are typically located in the bone of the skull base, but with pneumatization of a supraorbital ethmoid cell, the vessels can also traverse the ethmoid inferior to the skull base in what is characterized as a “low-hanging ethmoid artery” (Fig. 25.4). The optic canal is located an additional 6 mm posterior to the posterior ethmoid artery.
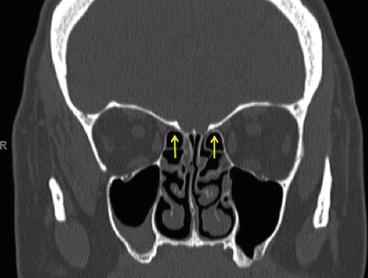
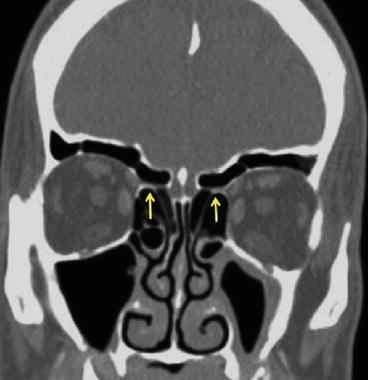
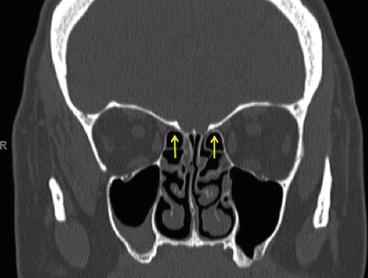
Fig. 25.3
Coronal CT, arrows pointing to anterior ethmoid arteries (With permission Andrew N. Goldberg, MD, MSCE, FACS)
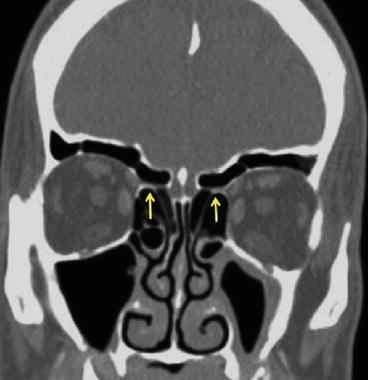
Fig. 25.4
Arrows pointing to “low-hanging” anterior ethmoid arteries (With permission Andrew N. Goldberg, MD, MSCE, FACS)
CT Scan Review
A systematic review of the CT scan is performed in the operating room prior to surgery. The review is conducted from anterior to posterior on the coronal CT one image at a time for the medial orbital wall and then for the skull base. This is followed by inspection of the height of the posterior ethmoid and sphenoid sinus configuration. Then the axial and sagittal images are then reviewed. The sagittal view is specifically inspected for the slope of the skull base from anterior to posterior.
Coronal CT
Medial orbital wall (integrity/dehiscence, relationship to uncinate, anterior ethmoid artery, Haller cell).
Skull base (integrity/dehiscence, lateral to medial slope, depth of cribriform).
Height of posterior ethmoid (measure from roof of maxillary sinus to fovea).
Sphenoid sinus configuration (integrity/dehiscence, course of sphenoid septum, Onodi cell).
Diseased areas and synthesis of the above features for formulation of a surgical plan. Special attention is paid to the frontal recess if it is to be addressed surgically.
Axial and Sagittal CT
Slope of the skull base
Ethmoid boundaries
Indications
Typically, the principal indication for surgical ethmoidectomy is for adult patients with chronic sinusitis or recurrent acute sinusitis that fail to respond to appropriate, maximal medical therapy. Generally, it is thought that enhanced drainage and ventilation of the sinuses may restore mucociliary clearance, encourage drainage through natural ostia, and facilitate the delivery of patient-administered nasal irrigations and topical medications. In the case of surgical ethmoidectomy, rarely is it performed alone. Most often, ethmoidectomy is performed in concert with a maxillary antrostomy to facilitate middle meatus drainage. In patients with diffuse pansinus disease, total ethmoidectomy is part of the surgical procedure to open all the involved paranasal sinuses.
Rarely is ethmoidectomy required urgently. However, in the case of rapidly progressive sinusitis with orbital and/or intracranial extension, formation of abscesses, or threat to patient survival, surgery may be more acutely indicated.
There are few absolute contraindications to ethmoidectomy. As with any surgery, patients not healthy enough to undergo anesthesia are considered poor surgical candidates. Caution should be used in any patient with a bleeding disorder, and appropriate preoperative counseling and referrals should be made. With the advent of image guidance and high-resolution video imaging, dehiscent orbital wall and skull base with exposed contents do not preclude the patient from undergoing surgery.







