Fig. 56.1
Schematic representation of the model. The flat epineural sheath graft was obtained by incising the removed nerve segment. (a–c) Repair of the defect was performed using one strip (d) two strips (e) and full rectangular epineural sheath graft (f)
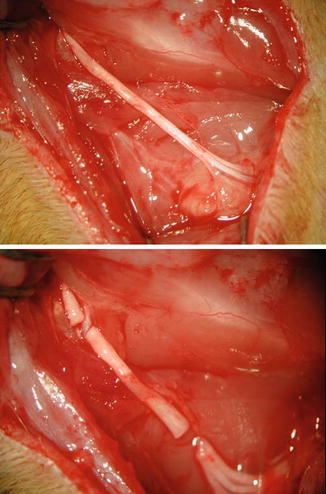
Fig. 56.2
Exposing the sciatic nerve from sciatic notch to bifurcation of tibial and peroneal branches (upper). Creation of sciatic nerve defect by removing 1.2 cm nerve segment (lower)
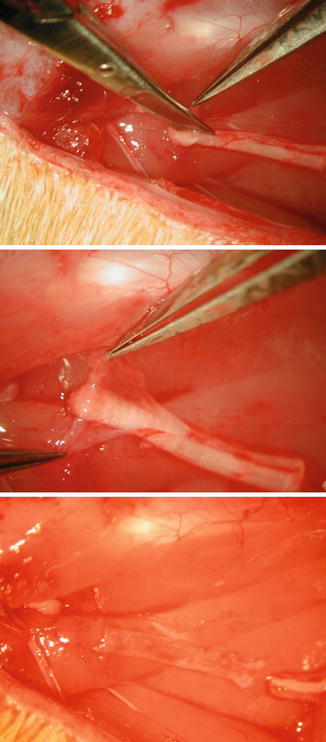
Fig. 56.3
The epineurium of the removed segment was incised (upper) and the fascicules within the segment were removed obtaining a flat rectangular-shaped epineural sheath graft (middle and lower)

Fig. 56.4
Close up view of the epineural sheath graft
Experimental Groups
In Group 1 (n = 6), after resection of the 1.2 cm segment of the sciatic nerve, the defect was left without repair. This group served as a control. In Group 2 (n = 6), the removed sciatic nerve segment was sutured back to its original place using the standard epineural technique with four interrupted 10.0 nylon sutures placed 90° apart. In Group 3 (n = 6), two epineural strips were obtained by splitting the flat rectangular epineural sheath graft longitudinally, and one strip was used to bridge the defect. The single epineural strip was secured to the proximal and distal stumps of the sciatic nerve by one centrally placed horizontal mattress suture using 10.0 nylon suture (Fig. 56.5). In Group 4 (n = 6), both epineural strips, that were obtained by longitudinal splitting of the epineurium, were used as a graft for bridging the defect. The strips were sutured to both ends of the sciatic nerve and placed 180° apart from each other. Each graft was secured by one epineural 10.0 nylon suture (Fig. 56.6). In Group 5 (n = 6), the flat rectangular epineural sheath was used to repair the defect as a full sheath graft without longitudinal splitting. The sheath was sutured to the proximal and distal stumps with two epineural sutures placed 180° apart (Fig. 56.7).
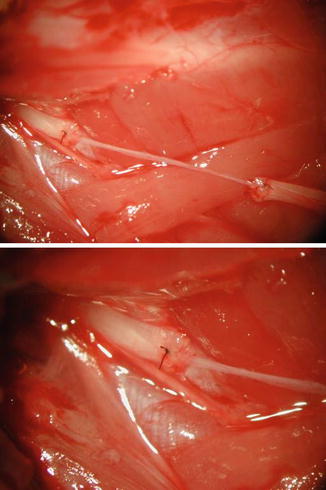
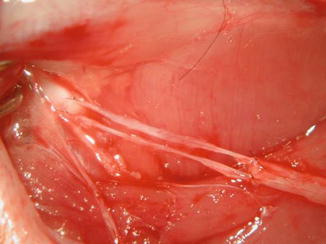
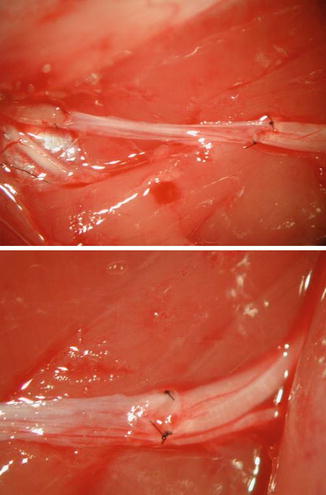
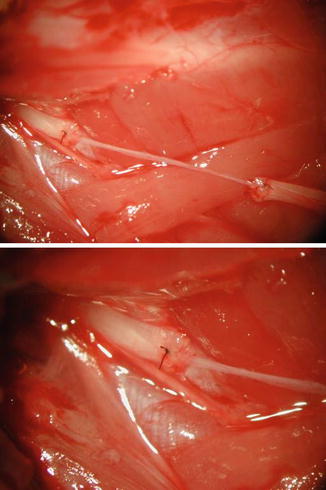
Fig. 56.5
Postoperative view following bridging nerve defect using one-strip of epineural sheath graft (upper) and close up view of the suture site at the proximal stump (lower)
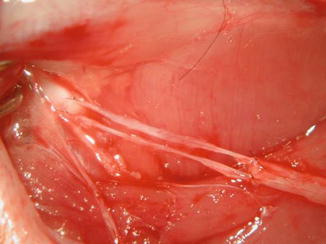
Fig. 56.6
Postoperative view following bridging the defect using two-strips of epineural sheath graft
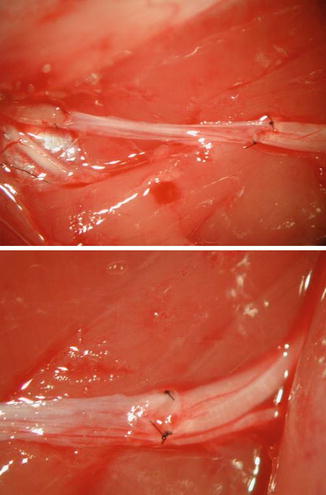
Fig. 56.7
Postoperative view following bridging nerve defect using full rectangular epineural sheath graft (upper) and close up view of the suture site at the distal stump (lower)
Following nerve repair in all groups, the gluteal fascia and the skin was closed with 4/0 vicryl suture.
Evaluation Techniques
Functional Evaluation
Clinical evaluation was performed using pin-prick test, toe-spread tests and somatosensory evoked potential test electrophysiologically (SSEP).
Pin Prick Test
Pin prick test was used for evaluation of sensorial recovery and this test was performed at 3, 6 and 12 weeks after nerve repair. The pin-prick test was performed by applying pinching stimuli with a standardized forceps to the hind-limb skin from the knee to the toes until a withdrawal of the extremity was obtained in response to the pain stimulus [12]. The withdrawal reflex was graded as 1 when obtained above the knee, as 2 when obtained distal to ankle and proximal plantar region and 3 when obtained at the toe level. The grade was accepted as 0 in the absence withdrawal reflex.
Toe-Spread Test
The toe-spread test was used for testing motor recovery and performed at postoperative weeks 3, 6 and 12. The rats were held by the tails and their toe-spread movements were graded between 0 and 3 in the following manner. The absence of any movement was graded as “0”, the presence of any sign of toe-spread was accepted as grade “1”; toe abduction as grade “2”, and both abduction and extension of the toes were accepted as grade “3” [12].
Electrophysiological Test
Electrophysiologic assessment was performed by somatosensory evoked potential evaluation (SSEP) at postoperative weeks 6 and 12 under general anesthesia. The positive and the negative potentials of the waveform morphology in the SSEP measurement were obtained and the initial negative wave was marked as N1 and the following positive wave as P1. The second negative potential was marked as N2. P1 and N2 potentials were used for comparison of sensory recovery between the groups as he P1 and N2 potentials are the most robust and consistent potentials.
Histomorphometric Evaluation
Evaluation of Gastrocnemius Muscle Atrophy
In each animal, gastrocnemius muscles were harvested from both sides at 12 weeks and wet-muscle weight measurements were taken immediately. The wet weight of the operated site was compared with the non-operated contralateral side and the ratio is calculated as the gastrocnemius muscle index (GMI). One hundred percent GMI is considered as full recovery. Then, the muscle underwent histopathological evaluation to determine the extent of atrophy.
Evaluation of Nerve Morphometry and Morphology
At postoperative week 12, a 1.5 cm segment of sciatic nerve including host proximal and distal segment and the connecting epineural sheath graft was excised and parameters such as nerve cross-sectional area (square mm), myelinated nerve density (per mm square), total number of myelinated nerve fibers, axonal diameter (μm) and myelin thickness (μm) were evaluated.
Statistical Analysis
The data was statistically analyzed using the Kruskal-Wallis Test for comparison between groups and the Mann-Whitney U Test for comparison within groups using SPSS 10.0 for Windows.
Results
Functional Evaluation
Pin-Prick Test
At 6 weeks, pin-prick test results revealed that the animals treated with full sheath graft and two-strip graft showed similar recovery and the results in these rats were better than one-strip group. Withdrawal at the toe level was observed in all groups at 12 postoperative weeks (Table 56.1).
Table 56.1
Functional evaluation results at postoperative 12th week
Groups | Pin-prick | Toe-spread | SSEP (mm/s) | GMI (WO/WC) | |||
|---|---|---|---|---|---|---|---|
Non-operated site | Operated site | ||||||
P1 | N2 | P1 | N2 | ||||
Autograft | 3.0 ± 0 | 2.83 ± 0.40 | 16.38 ± 0.89 | 21.56 ± 1.14 | 17.47 ± 1.62 | 24.84 ± 2.14 | 0.48 ± 0.10 |
One-strip | 2.33 ± 0.51 | 1.16 ± 0.40 | 15.79 ± 0.67 | 22.61 ± 3.00 | 19.06 ± 3.02 | 26.25 ± 2.48 | 0.23 ± 0.13 |
Two-strip | 2.83 ± 0.40 | 2.0 ± 0.63 | 16.19 ± 1.24 | 22.58 ± 3.10 | 17.47 ± 1.57 | 24.98 ± 2.08 | 0.38 ± 0.09 |
Full-sheath | 2.66 ± 0.51 | 2.16 ± 0.40 | 16.19 ± 0.78 | 22.47 ± 0.84 | 16.24 ± 1.85 | 24.61 ± 2.36 | 0.47 ± 0.09 |
Toe Spread Test
Toe spread test showed better motor recovery in animals treated with full epineural sheath grafts and autografts at 6th week. At 12 weeks postoperatively, these animals showed better values for abduction and extension of toes indicating full regeneration (Table 56.1). No sign of movement was observed in the non-treated group at 12 weeks.
Somatosensory Evoked Potential
The P1 and N2 latencies are shown in Table 56.1. At 6 weeks postoperatively, the P1 and N2 latencies were significantly prolonged in operated limbs in the treated groups compared with the contralateral normal limbs. These values were comparable in animals treated with the nerve autograft, full epineural sheath grafts and two-strip grafts (Fig. 56.8). The latencies did not reveal improvement in the animals treated with one strip graft; however, there were no statistically significant differences in the P1 and N2 latency values between the treated groups at 12th week.
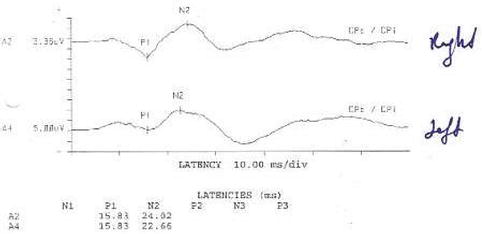
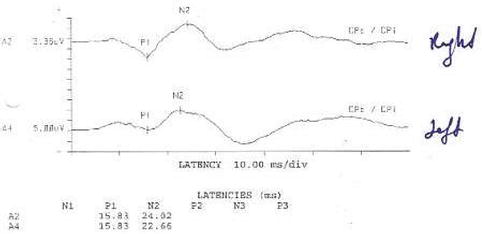
Fig. 56.8
An example of the appearance of P1 and N2 waves and latencies obtained by SSEP test in an animal repaired with full epineural sheath. Superior wave is obtained from operated side and the inferior wave from the ipsilateral control limb. Both waves show similar patterns
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








