Endovenous Laser Ablation
 INTRODUCTION
INTRODUCTION
When saphenous system reflux is present, it must be addressed prior to treatment of visible and associated varicosities, reticular veins, or telangiectasias. Endovenous occlusion techniques using radiofrequency (RF) or laser have become the standard of care in the United States. When using laser, they are termed ELT or ELA, which are abbreviations for endovenous laser therapy or treatment or endovenous laser ablation, respectively. Without elimination of reflux, the patient will be doomed to recurrence after recurrence of varicosities below the level of saphenous vein reflux. Previously, the only treatment option for these patients with varicose veins from saphenous insufficiency was surgical ligation and stripping of the vessels under general anesthesia. This procedure resulted in significant postoperative down time, with surgical scars, swelling, bruising, and pain. The expense of a hospital stay and missed work, along with an unacceptable rate of recurrence, has greatly decreased the popularity of this procedure and relegated it to low technology medical arenas (see Chapter 23). Like many other fields of medicine, varicose vein treatment in the 21st century has evolved and adopted less-invasive methods. RF ablation started the minimally invasive varicose vein trend with approval in March 1999 by the U.S. Food and Drug Administration (FDA) as the Closure® procedure (VNUS Medical Technologies, San Jose, CA). Endovenous ablation techniques utilizing lasers were subsequently filed as U.S. FDA 510(k) applications as substantially equivalent procedures to RF ablation. The first laser FDA cleared by substantial equivalence to RF was the 810-nm diode laser, which was cleared for marketing in 2000.
The advances in endovenous ablation have revolutionized in-office varicose vein treatment for physicians and patients. Table 21-1 summarizes the laser endovenous systems and their trade names. Lasers can be thought of in two categories: hemoglobin absorption predominant and water absorption predominant. The water absorption predominant wavelengths are primarily above 1100 nm in which hemoglobin is no longer a chromophore (Figure 21-1). There are numerous advantages to predominant water absorption, which are discussed below.
TABLE 21-1
Endovenous Lasers and Associated Trade Names
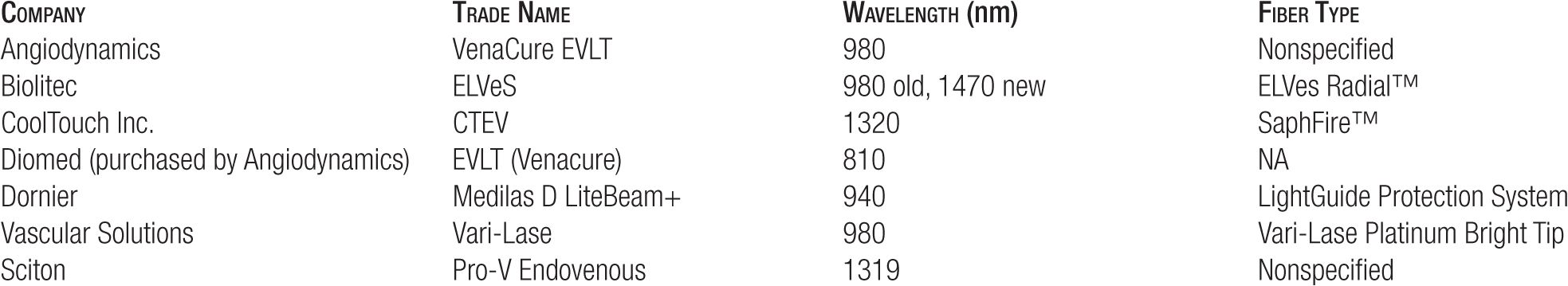
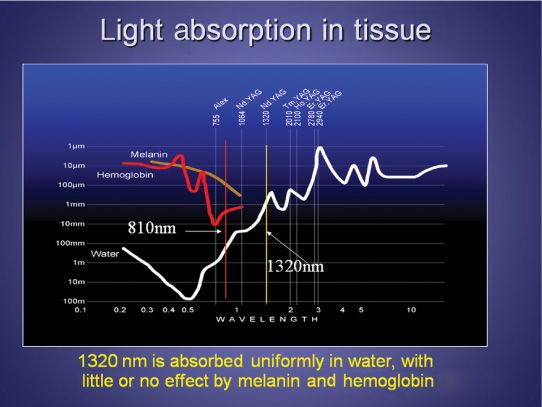
![]() FIGURE 21-1 Absorption curves of light through infrared wavelengths. There is virtually no absorption by hemoglobin beyond 1100 nm. Water is the target of 1320 nm.
FIGURE 21-1 Absorption curves of light through infrared wavelengths. There is virtually no absorption by hemoglobin beyond 1100 nm. Water is the target of 1320 nm.
 LASERS WITH HEMOGLOBIN ABSORPTION PREDOMINANT (810, 940, 980, AND 1064 nm)
LASERS WITH HEMOGLOBIN ABSORPTION PREDOMINANT (810, 940, 980, AND 1064 nm)
Endovenous laser treatment with these wavelengths is designed to produce endothelial and vein wall shrinkage by nonspecific heating of the vessel, often by a superheated coagulum at the fiber tip or by the heating of hemoglobin within red blood cells to create steam bubbles.1 The target for lasers with 810-, 940-, 980-, or rarely 1064-nm wavelengths is the intravascular red blood cell. Without the presence of blood in the vein, such as in an experimental situation in which the vein is filled with saline, laser-induced vessel wall injury is confined to a small site of direct laser impact. By contrast, blood-filled veins exhibited thermal damage in more remote areas including the vein wall opposite to the laser impact. Steam bubbles are generated in hemolytic blood by all four lasers, while no bubbles can be produced in normal saline or plasma.1 Therefore, the success of these lasers is highly dependent on correct placement of tumescent local anesthesia to have a thin layer of blood surrounding the laser fiber while having enough anesthesia to protect the surrounding nerves and muscles from injury. This can be difficult to achieve and results in unpredictable pain and recurrence.
Direct thermal effects on the vein wall without the presence of blood may lead to small spots of wall injury with resulting pain and early recanalization of the treated vein.2 Less consistent clinical results are seen than with RF ablation (Chapter 23) or with 1320-nm endovenous laser (discussed later). Considerable site-to-site variation in success rates and postoperative pain for ELT have been reported.3,4 This is understandable given that these lasers are dependent on so many different factors, including the amount of blood in the lumen, the rate of pullback, pulsed versus continuous laser output, and the amount of tumescent anesthesia placed around the vein. Overall long-term efficacy of hemoglobin targeting lasers is less than that of water-absorbing lasers.
Endovenous Laser Therapy (EVLT) 810 nm
This wavelength was the first to be utilized in an endovenous application. Termed EVLT to abbreviate ELT, EVLT was trademarked for the 810-nm diode laser. Patent infringement lawsuits were filed and successfully litigated on the basis of the EVLT patent application. Initial reports showed the endovenous ablation technique with an 810-nm diode laser to have good short-term efficacy in the treatment of the incompetent great saphenous vein (GSV), with 96 percent or higher occlusion at nine months with a less than 1 percent incidence of transient paresthsia.4,5 In one follow-up study of 810-nm laser treatment, 93.4 percent of GSVs followed for two years remained closed.6 Our long-term success rates with this laser are in the range of 70 percent at three years.
This wavelength is problematic as some patients experience major degrees of postoperative ecchymosis and discomfort (Figure 21-2). Skin burns have been reported for 810 nm7 and we have seen consultations for skin burns (Figure 21-3). When using a wavelength strongly absorbed by hemoglobin, such as 810 nm, there is a lot of intraluminal blood heating with transmission of heat to the surrounding tissue through long heating times. We have found superheating of blood during these procedures in an animal model to a maximum of approximately 1200°C measured by a thermocouple at the tip of the laser fiber.2 Even several millimeters away from the tip, temperatures greater than 400°C were recorded.2 When we have tried ex vivo vein treatment without blood, the 810-nm wavelength simply chars the inside of the vein without shrinkage of the vein wall. When blood is added to the ex vivo veins and then treated with 810 nm, numerous vein perforations due to overheating are observed (Dr. M. Hirokawa, Tokyo, Japan, personal communication, 2005). When treating goat jugular vein in an experimental model, vein perforations occur at each site of laser impact.2
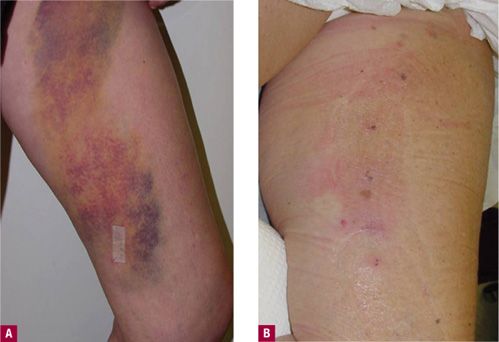
![]() FIGURE 21-2 One-day postendovenous laser ablation. A. 810-nm diode demonstrates bruising. B. Endovenous RF ablation shows no bruising.
FIGURE 21-2 One-day postendovenous laser ablation. A. 810-nm diode demonstrates bruising. B. Endovenous RF ablation shows no bruising.
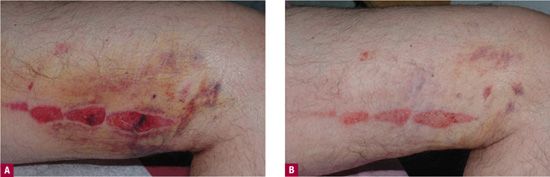
FIGURE 21-3 A. Skin burns caused by diffusion of heat from 810-nm diode endovenous laser seen at four days after procedure. B. After treatment by photomodulation at 11 days after procedure.
In our experience, patients treated with an 810-nm diode laser have shown an increase in post-treatment purpura and tenderness when compared with treatment with RF or 1320-nm CTEV™ (CoolTouch Corporation, Roseville, CA) laser ablation as shown in Figure 21-2. Most of our patients treated with 810 nm do not return to complete functional normality for two to seven days as opposed to up to 24-hr “down-time” with CTEV™ and 24–72 hr with RF ClosureFast™. There is even less down time with CTEV™ as discussed later, with most patients returning to work the next day.
For a time, the vein perforations seen with 810-nm diode were blamed on pulsing of the laser versus continuous operation. Studies were published, which stated that pulsed 810-nm diode laser treatment posed an increased risk for vein perforations as opposed to continuous treatment.2 Pulsing versus continuous mode was initially blamed for the vein perforations and increased symptoms with 810-nm laser versus RF treatment. This was found to be related to the 810-nm wavelength and superheating of hemoglobin and not the pulsing of the laser. Our experience with trying to vary the fluence and treating with a continuous laser pull-back versus pulsed pull-back has not resulted in an elimination of vein perforations using the 810-nm diode laser (Figure 21-4).
![]() FIGURE 21-4 Perforations seen in goat vein using 810-nm diode laser in pulsed mode. Contrast material oozes into surrounding tissue through the perforations.
FIGURE 21-4 Perforations seen in goat vein using 810-nm diode laser in pulsed mode. Contrast material oozes into surrounding tissue through the perforations.
Medilas D LiteBeam+ 940 nm
One in vitro study model has predicted that thermal gas production by laser heating of blood in a 6-mm tube results in 6-mm of thermal damage.1,8 These authors used a 940-nm diode laser with multiple 15-J, 1-s pulses to ablate the GSV. A median of 80 pulses (range 22-116) were applied along the treated vein every 5–7 mm. Histologic examination of one excised vein demonstrated thermal damage along the entire treated vein with evidence of perforations at the point of laser application described as “explosive-like” photo-disruption of the vein wall. Formation of bubbling blood is the proposed mechanism of action for heating surrounding tissue with generation of steam bubbles that heat the vein wall more completely.8 The generation of steam bubbles is believed to be the most reliable method of vein wall ablation. A longer wavelength such as 940 nm has been hypothesized to penetrate deeper into the vein wall resulting in increased efficacy, but this wavelength penetration may be entirely due to the intensity of absorption by hemoglobin and/or water.
A report of 280 patients with 350 treated limbs with 18-month follow-up demonstrated complete closure in 96 percent.9 Twenty vein segments were examined histologically. Veins were treated with 1-s duration pulses at 12 J. Perforations were not present. When the fluence was increased to 15 J with 1.2- and 1.3-s pulses, microperforations did occur and were said to be self-sealing. Essential components of treatment were use of tumescent anesthesia and laser parameters of 12 J or less. These measures limit significant perforations and enhance efficacy. Tumescent anesthesia has been a critical component for the success of all endovenous ablation techniques (see Chapter 23 and also the discussion in this chapter). Studies comparing 940-nm hemoglobin targeting ELT of the GSV versus water targeting 1320-nm Nd:YAG laser have demonstrated that 1320 nm causes fewer side effects compared with 940-nm diode laser.10 This is mostly likely due to increased absorption by water.
Vena-Cure, ELVeS 980 nm
This wavelength emitted from a diode laser has also been used in endovenous ablation. One study reports four-year results in 500 patients using this wavelength.11 In the immediate postoperative period, the closure rate was 98.0 percent and remained constant during the four-year follow-up to reach 97.1 percent.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


