Endemic (Nonvenereal) Treponematoses: Introduction
|
Introduction
The endemic, or nonvenereal, treponematoses are infections caused by bacteria that are closely related to Treponema pallidum pallidum, the etiologic agent of venereal syphilis. These include Treponema carateum (pinta), Treponema pallidum pertenue (yaws), and Treponema pallidum endemicum (bejel or endemic syphilis). The diseases are distinguished from venereal syphilis by mode of transmission, age of acquisition, geographic distribution, and clinical features. Unlike syphilis, they are transmitted mostly among children living in tropical and subtropical climates, chiefly by casual contact rather than sexual contact, and congenital infection is unusual. As many as 2.5 million persons are believed to be infected with nonvenereal treponematoses. However, a significant proportion of infected persons remain asymptomatic. Like venereal syphilis, the diseases progress through successive clinical early (primary and secondary) and late stages usually separated by periods of latency.1
Without treatment, patients remain potentially infectious indefinitely, although the skin lesions may become inconspicuous or subclinical. Patients do not develop lifelong immune resistance. Cross-immunity is absent in the early stages of endemic syphilis, yaws, and pinta but is variable in late stages. Notably, patients with late pinta are resistant to syphilis, but those with yaws or syphilis at any stage are susceptible to pinta. The level of cross-protection may be proportional to the severity of the initial infection.1 Untreated treponematoses are nonfatal but may cause cutaneous lesions and deformities of the bone and cartilage. This potentially leads to significant disfigurement, pain, disability, and social isolation, thus incurring a significant economic burden on already disadvantaged populations.
Microbiology
The different treponemal species causing venereal and nonvenereal treponematoses are morphologically and serologically identical and induce comparable histopathological changes. This reflects the high antigenic relatedness among these organisms and justifies the long-standing controversy about the origin of these diseases. Some authors had even claimed that the morphologically identical treponemes represent the same organism causing different clinical manifestations under different climatic conditions.2 Over the past two decades, evidence from molecular studies has accumulated supporting the argument for species specificity. Molecular data have allowed the elucidation of genetic features differentiating T. pallidum pallidum from the nonvenereal treponemes.3–7 It was not until recently that Centurion et al identified subspecies-specific genetic signatures in the trp gene family that allow differentiation among the T. pallidum subspecies.8
Pinta (Carate, Mal De Pinta, Azul)
Pinta is an ancient disease that was first described in the sixteenth century in Amerindians.9 The causative organism is T. carateum, which is the least antigenically related to the other human treponemes as it is a separate species from T. pallidum. The name of the organism derives from the Colombian word for the disease (“carate”), in reference to the color changes seen in persons having the disease. The organism can be propagated only in primates, and no isolates are known to exist.10 Consequently, much less is known about this treponeme than any of the others.
The incidence of the disease has remarkably decreased over the last few decades. Today, pinta remains prevalent in scattered foci in rural areas of Central and South America (Southern Mexico, Brazil, Colombia, Venezuela, Peru, and Ecuador), where people still live in crowded, unhygienic conditions. People of all ages may be infected. However, half of all patients are younger than 15 years of age.11 The exact mechanism of disease transmission is not fully elucidated, but repeated direct lesion-to-skin contact is the most likely mode. Transmission through insects is unlikely.1 Because cell-mediated immunity is not completely effective against this organism, untreated infection persists indefinitely.
Pinta is the most benign of the endemic treponematoses with the skin being the only organ of involvement. As in syphilis, there are three distinct clinical stages. Lesions at different stages may be present in a single patient. Lymphadenopathy may develop during any stage.
A small number (1–3) of erythematous macules or papules appear at the site(s) of inoculation after an incubation period of 1–8 weeks. Primary lesions are usually nonpruritic and do not ulcerate. Sites of predilection include exposed areas of the extremities in addition to the face and neck. The initial lesions expand or coalesce with other lesions over several weeks to months, forming irregular scaly lichenified plaques that can reach a diameter of up to 20 cm (Fig. 201-1).12 Over time, the center of the lesions becomes hypochromic, grayish, light blue, or pale mauve.1 Eventually, lesions may heal spontaneously with residual depigmentation13 or may persist for years.
After several months and occasionally up to 10 years after the initial infection, secondary lesions (pintids) start to appear. These are highly infectious lesions teeming with spirochetes.12 Like the primary lesions, pintids start as erythematous scaly papules that enlarge and coalesce into psoriasiform plaques. However, they tend to be smaller and more extensive than the primary lesions. They may encircle the sites of the primary lesions or erupt generally on the body. Pintids may occur on the palms, soles, and groin.1 Some lesions may be circinate or annular with raised borders where the number of treponemes is highest. Over time, lesions display remarkable variation in color ranging from copper colored to gray to slate blue.11
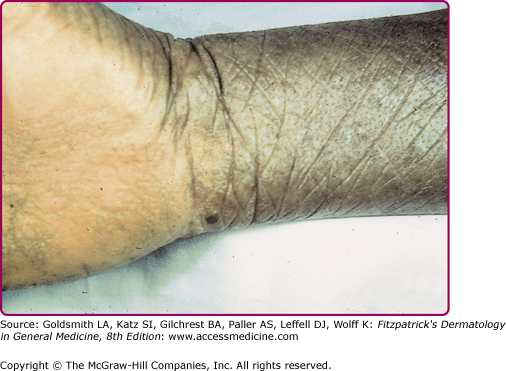
Late lesions usually develop 3 months to 10 years after the appearance of the secondary lesions. Typically, patients have dyschromic patches that are hyperchromic, hypochromic, and achromic, which impart a mottled pattern with a variegated palette of white, brown, blue, red, and violet. The lesions have irregular borders and vary in size. The most commonly involved areas are the wrists, palms, ankles, and elbows as well as the skin around and within old lesions (Fig. 201-2). It is common for periarticular lesions of pinta to exhibit scarring and atrophy (“cicatricial lesions of pinta”).9 This is in contrast to extensor surface plaques that tend to be hyperkeratotic.14 Patients with only late-stage lesions may appear to have vitiligo (“vitiligo of pinta”).
Differential Diagnosis
Most Likely
|
Consider
|
Always Rule Out
|
Yaws (Framboesia Tropica, Pian, Buba, Paru, Parangi)
Yaws is caused by T. pallidum pertenue. The spirochete can be propagated in laboratory animals, and various strains have been isolated for investigation.1 The infection affects rural populations along the tropical belt in areas with high humidity, heavy rain, and annual temperatures at and above 27°C.15 The spread of the spirochete is facilitated in the setting of poor hygiene, scanty clothing, and overcrowding.11
Yaws is the most prevalent nonvenereal treponematosis. An estimated average of 50 million persons was infected in the early 1950s. Massive WHO supported treatment campaigns were carried from the mid-1950s to the early 1960s, which resulted in a dramatic decrease in the prevalence of the disease.16 However, due to relaxed surveillance and control measures, under-diagnosis, and the persistence of poor sanitary conditions, a resurgence of yaws has been documented in regions of Africa and Southeast Asia. Sizable foci have been reported in several tropical regions of western and central Africa (Ghana, Togo, Benin, and the Central African Republic), and residual foci remain in South America (Colombia, Guyana, Peru, Ecuador, and Brazil), Haiti, Dominica, Southeast Asia, Indonesia, Papua New Guinea, and the Solomon Islands.11 Approximately 75% of new cases arise in children younger than 15 years of age.17,18 Currently, at least 100 million children are estimated to be at risk of becoming infected.1
The main route of transmission of yaws is direct skin-to-skin contact and via contact with open wounds, excoriations, or bites.19 Some experts claim that the disease can be transmitted through domestic utensils or by the eye flies (eye gnats) that are 1.5–2.5 mm long and do not bite but rather feed on body fluids of various animals including humans.1
Yaws shares numerous clinical characteristics with venereal syphilis. In contrast to pinta, the disease is not skin-limited. Among the nonvenereal treponematoses, the disease is characterized by the most destructive and disfiguring skeletal involvement.
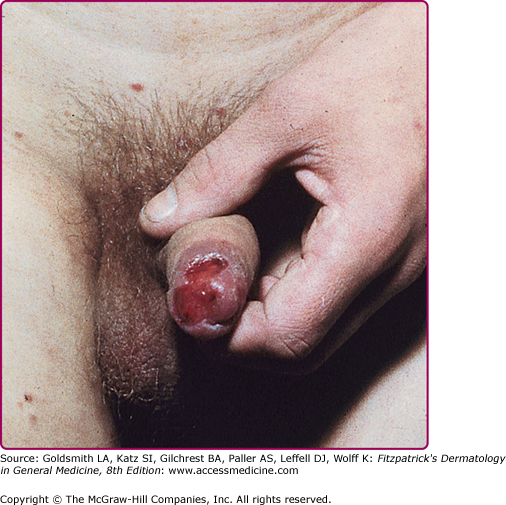
In the primary stage, skin lesions appear after an incubation period of 10–90 days (on average 3 weeks). Classically, the initial presentation is a single nontender but often pruritic erythematous infiltrated papule (mother yaw or buba madre) that often acquires a papillomatous surface.1 Its location often indicates the site where the spirochete penetrated the skin, usually the legs, feet, or buttocks.20 Satellite papules may be present. Over time, the mother yaw enlarges radially reaching up to 5 cm in diameter and occasionally merges with the smaller satellite lesions forming a larger plaque. It often ulcerates, forming the “chancre of yaws”, and develops a yellow–brown crust which ultimately sloughs off, uncovering a moist soft base that is often likened to a raspberry, hence the synonym “framboesia” (Fig. 201-3). The ulcer is very rich in treponemes. Fever, regional lymphadenopathy, and arthralgias may accompany this stage.14 The mother yaw heals over 3–6 months but sometimes remains through the secondary stage of the disease. It typically leaves a depigmented pitted scar with dark margins.21
The lesions of secondary yaws, known as “daughter yaws” or pianomas, may appear while the mother yaw is still present, but may take up to 2 years to develop.1 These lesions resemble the mother yaw but are smaller (up to 2 cm) and more disseminated (Fig. 201-4A). They are often accompanied by constitutional symptoms such as fever, malaise, and generalized lymphadenopathy. Over time, daughter yaws may ulcerate and secrete a fibrinous exudate teaming with infectious treponemes (Figs. 201-4B and 201-4C).
Figure 201-4
A. Early secondary lesions of yaws (daughter yaws) appearing as eroded and crusted papules and plaques. B. Warty secondary-stage papillomas (daughter yaws). C. Eroded papillomas covered by fibrinous exudate. (B and C used with permission from H.J.H. Engelkens, MD, J. van der Stek, MD, and E. Stolz, MD.)
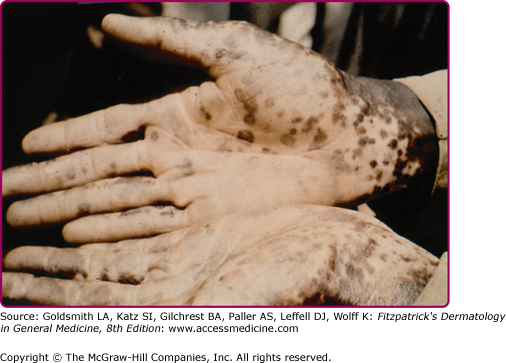
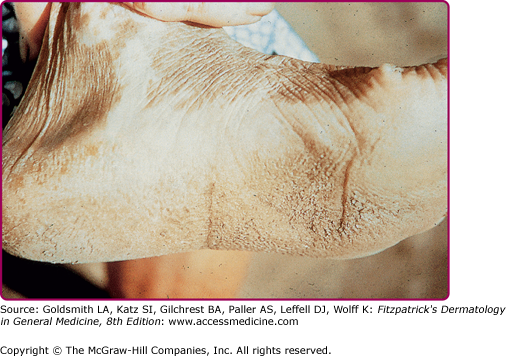
The exudate attracts flies, which can cause great suffering to the affected person. Lesions usually favor perioroficial locations, such as around the mouth and nose.14 In addition to the characteristic exudative papillomas, dry papulosquamous patches (pianides), comparable to those seen in venereal syphilis, may appear on any body part.20 Occasionally, central clearing results in an annular morphology simulating a fungal infection and these have been called “tinea yaws.”14 In the body folds, secondary lesions simulate condyloma lata. More rarely, the mucous membranes, especially the oral cavity, are involved in the form of hypertrophic mucous patches.1 Hyperkeratotic lesions, affecting mainly palms and soles, are characteristic. They are referred to as “crab yaws” because they get fissured and infected resulting in a painful “crablike” debilitating gait (Fig. 201-5).17 Periungual hyperkeratosis results in a paronychia which is known as “pianic onychia.”22 Of special interest is the influence of the climate on the clinical expression of yaws. During wet seasons, lesions tend to be more florid and diffuse whereas they are less exudative and confined to the moist intertriginous areas in the setting of a dry climate.11 They also tend to assume atypical morphologies in dry seasons. Some reports describe an attenuated, less contagious form of yaws in areas of low disease prevalence. This form is less florid with few (even single), small, dry, lesions that are often limited to skin folds.1
Bone and joint manifestations may already occur during this early stage of the disease.23 These consist of painful osteoperiostitis of the forearm or leg, in addition to the proximal phalanges of the hands or feet. The characteristic “ghoul (monster) hands” appearance reflects swelling of the proximal two phalanges.1 Some of the early bone changes can be seen on radiographs. Periosteal thickening can often be palpable.24
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree