Edema
Peter J. Lynch
Genital edema occurs as a result of fluid buildup in the subcutaneous tissue of the genitalia. The fluid may be related to plasma or lymph. The former is termed angioedema and is generally transient (acute genital edema), whereas the latter is termed lymphedema and is persistent (chronic genital edema). The term elephantiasis is often used for lymphedema that is chronic and massive. In some instances, especially when vessel-damaging inflammation is present, angioedema may transition into lymphedema blurring the line of identification between these two forms of edema.
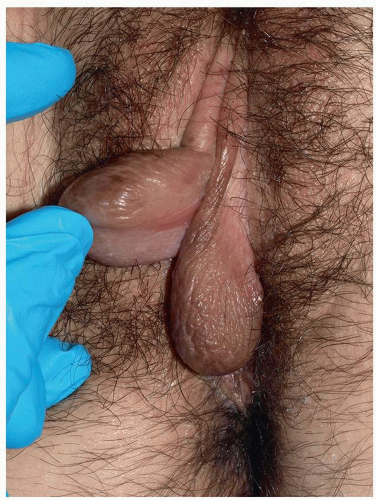
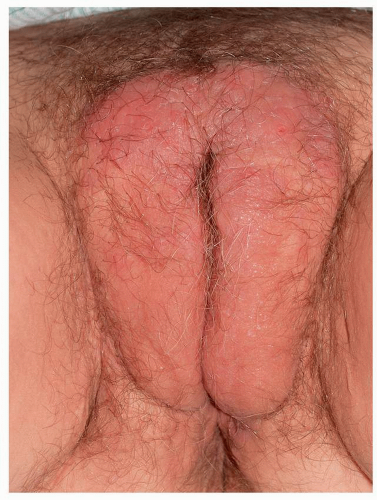
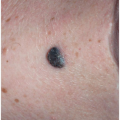
For the most part, the clinical presentation in both forms of edema is quite similar in that the tissue of the genitalia is distended to greater or lesser degree. However, in acute genital edema, the tissue on palpation is softer, “pits” more easily, and is more variable in duration and extent (Fig. 12.1). Chronic lymphedema, on the other hand, is more firm on palpation, pits less easily, lasts longer, and is more likely to be stable in severity and extent (Fig. 12.2).
Both forms of edema are usually asymptomatic though with sudden distention, stretching of the tissue may lead to some pain. Acute genital edema due to allergic reactions may be associated with varying degrees of itching.
Acute Genital Edema (Angioedema)
Most instances of acute genital edema are due to allergic reactions occurring as a result of topical applications or systemic ingestion of products to which the patient, because of prior exposure, has developed immune reactivity. This form of edema develops over minutes to hours and evolves over hours to days. The tissue returns to its former normal size and appearance after each episode of edema.
Immunoglobulin E-mediated Acute Edema
The most important and dangerous forms of acute genital edema are those that occur as a result of immunoglobulin E (IgE) reactions. Individuals with such reactions are potentially liable to develop anaphylaxis. The two most common allergens causing localized genital IgE-mediated reactions are latex and semen.
Latex Allergy
Latex allergy occurs in about 4% of health care workers and about 1% of the general population. Awareness of the problem caused by latex allergy has led to a decrease in the use of latex products, notably latex-containing examination gloves, and the prevalence of latex reactions seems to be decreasing. However, latex still is present in some condoms and contraceptive diaphragms, and therefore, genital edema due to these sources is still a potential problem. Confirmation of suspected latex allergy as a cause for genital edema can be obtained through radioallergosorbent (RAST) testing and skin prick tests.
Semen Allergy
There are only several hundred reports of genital edema in women who were allergic to their male partner’s semen (seminal plasma), but it is probably much more prevalent than this figure suggests. In fact, there may be as many as 40,000 women in the United States who are affected (1). Semen allergy should be suspected when vulvovaginal symptoms, especially that of vulvar swelling, occur shortly after unprotected coitus. Women who develop systemic reactions do so as part of an IgE response to seminal fluid, whereas the type of immune reaction is appreciably less clear in those who experience only local reactions (2). A suspected diagnosis can usually be confirmed through the observation that no reaction occurs after an intercourse in which a condom is used. Irritant (traumatic, prolonged intercourse) and allergic reaction to Candida sp. should be considered in the differential diagnosis of suspected semen allergy. Specific immunologic treatment for this problem lies outside the scope of this book.
Genital edema as part of a more widespread reaction with edema occurring at other sites, sometimes in association with anaphylaxis, can also occur with IgE allergy to ingested foods such as peanuts and shellfish. Prophylactic and/or therapeutic use of oral antihistamines may be of some help in these IgE-mediated reactions, but they are
seldom sufficient by themselves. Consultation with an allergist is usually desirable.
seldom sufficient by themselves. Consultation with an allergist is usually desirable.
Genital edema can be related to topically applied products. This type of reaction generally is a type 4, cellmediated immune response. Most often, this presents as a form of contact dermatitis with attendant eczematous morphology, but a few cases of anaphylaxis have occurred due to the application of the common topical antibiotics, neomycin and bacitracin. Such reactions can result in genital edema, but they differ from the IgE reactions in that they occur many hours after exposure, are accompanied by more redness, and may have an eczematous appearance in addition to the genital swelling. These types of allergic contact dermatitis and the products that most frequently cause them are covered in the eczematous disease section of Chapter 6.
Bradykinin Pathway-mediated Acute Edema
Genital edema can also occur in patients with non-IgE allergic reactions mediated by way of the bradykinin pathway (3).This type of edema most commonly occurs in patients receiving angiotensin-converting enzyme inhibitors. Such patients make up 30% to 40% of patients seen for angioedema in emergency departments (4). Genital involvement occurs in a small percentage of these patients (5). Similarly, genital involvement occurs in some patients with the rare disorder, hereditary angioedema, another condition mediated through the bradykinin pathway. The angioedema in both of the situations responds well to icatibant, a bradykinin B2 receptor antagonist (4).
Acute Genital Edema Related to Infection
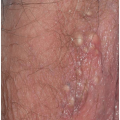
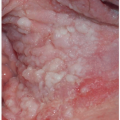
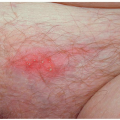
Genital edema can also occur in the setting of infection most notably cellulitis in both sexes and in women with vulvovaginal candidiasis and males with epididymitis (Figs. 12.3 and 12.4). Acute-onset genital edema accompanied by malaise, chills, fever, and WBC elevation may indicate the initial symptoms and signs of necrotizing fasciitis (Fournier gangrene). This represents an impending, potentially fatal medical emergency that should
result in hospitalization and immediate consultation with experts.
result in hospitalization and immediate consultation with experts.
Acute Genital Edema Related to Trauma
Rarely, acute genital edema occurs in settings of trauma, notably that due to long stints of bicycle riding (6). Traumatic edema is usually apparent from history but can also occur as a result of unrecognized “hair coiling” with resultant “strangulation.” This most often involves the clitoris in women and the glans penis in men. Other infrequently encountered instances of acute genital edema occur during procedures such as peritoneal dialysis and paracentesis (7,8). Acute and subacute vulvar edema occurs in women in pregnancy, especially pregnancy with preeclampsia, and following parturition after a difficult delivery.
Idiopathic Acute Genital Edema
Acute idiopathic scrotal edema (AISE) is an uncommon condition occurring in boys and adolescents that has mostly been reported in the urology literature (9). It occurs in mid to late childhood and presents with an acute onset of asymptomatic redness and edema of the scrotal sac (10). The involvement is unilateral in most of the cases, and the entire process generally resolves spontaneously in a matter of a few days. Sometimes the process is recurrent (10). The cause is unknown, and there is no specific recommended therapy. It must be differentiated from testicular torsion and epididymitis. This can usually be accomplished by ultrasound (9).
Chronic Genital Edema (Elephantiasis)
Chronic genital edema occurs as a result of lymphatic flow disruption secondary to infection, noninfectious inflammation, surgery, radiation therapy, and congenital abnormalities and also as a seemingly idiopathic process. In all of these situations, the process is disfiguring and extraordinarily troublesome to patients both physically and psychologically. Unfortunately, treatment is never curative and is only rarely of significant help.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree