Summary
Do not let exposed cartilage become an issue, almost all cartilage defects with intact perichondrium will heal well secondarily.
The majority of ear reconstruction cases can be done with simple full-thickness skin grafting.
Use caution with primary closure or Antia–Buch flaps to not distort the repaired ear compared to the contralateral side.
Leave the normal contralateral ear alone.
For large defects in elderly patients, consider a prosthetic ear reconstruction.
19.1 Algorithm for Ear Reconstruction
19.1.1 Anatomical Considerations
Anatomical considerations of ear reconstruction encompass both aesthetic as well as functional issues (▶ Fig. 19.1 and ▶ Fig. 19.2). Functionally, it is important to maintain the vertical height of the ear in relation to the normal contralateral side as this is the platform for eyeglass wearing and maintenance of symmetry is important. Also, the accompanying effect of the ear to wide binaural localization, and therefore prevention of external auditory canal stenosis, is important. 1, 2 From an aesthetic standpoint, it is quite important to maintain the continuity of the helical rim as any step-off, even small, will draw the viewer’s attention much as a vermilion border step-off on the lip. Additionally, the ear has limited laxity and does not tolerate significant soft-tissue closure, and any attempt at this without cartilage resection often results in forward buckling of the ear. Conversely, the presence of cartilage throughout the ear provides an excellent framework for full-thickness grafting and with successful full-thickness grafting, the antihelix and helix shape and contour can be successfully re-created.
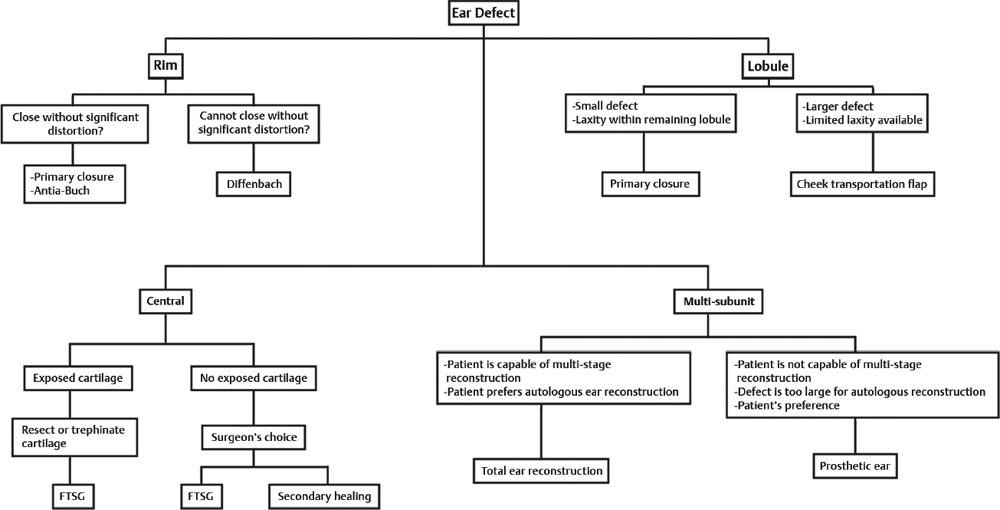
Fig. 19.1 Algorithm for ear reconstruction.
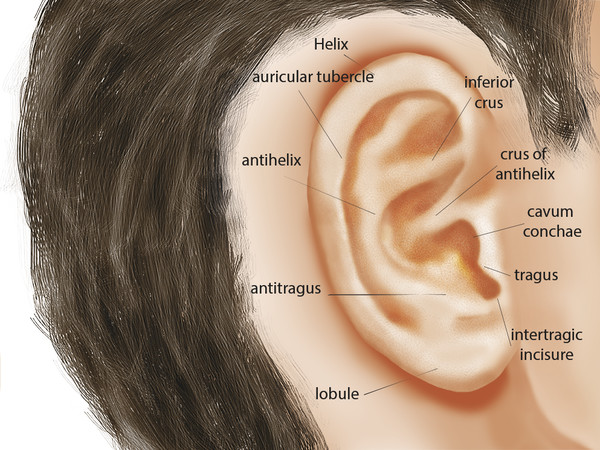
Fig. 19.2 Anatomy of external ear.
19.2 Commonly Applied Methods of Closure
Allow wound to heal in secondarily.
Full-thickness skin grafting.
Local wedge or flap closure.
Folded postauricular flap two-stage reconstruction.
Prosthetic ear.
19.2.1 Secondary Closure
Large areas of the ear can heal secondarily with no secondary contraction as long as the perichondrium is intact. 3, 4 Careful monitoring and wound care is required for uneventful wound healing. Traditionally, we provide just a simple topical antibiotic ointment that is converted to Vaseline ointment after approximately 10 days. We allow the patient to shower on the second postoperative day and then a nonstick dressing (Xeroform) is applied at night. We will dress the ear with a simple stockinette dressing if the patient desires. 5 Tape is avoided at all times. The presence of exposed cartilage with absent perichondrium is not a contraindication to secondary healing, given this can be simply resected and the remaining area be allowed to heal. 3 The use of assistive wound healing devices including acellular dermis can provide faster healing with reduced requirements for dressing changes by the patient (▶ Fig. 19.3).

Fig. 19.3 A 67-year-old male status post 3.5 × 2 cm Mohs excision of basal cell carcinoma at right tragus. Wound was allowed to heal secondarily. Results shown 2 months after resection.
19.2.2 Full-Thickness Skin Grafting
Full-thickness grafting constitutes the majority of our ear reconstruction cases. 6 It is a very safe and highly reliable technique. The full-thickness skin is harvested from the ipsilateral neck and significantly thinned to match the thickness of the skin native to the host site on the ear. The key to ensure complete graft take is careful bolster placement on the graft, which frequently requires the majority of operative time. 7 The graft itself is sewn in place with 5–0 plain gut suture and then multiple mattress sutures of through-and-through 4–0 plain gut with a straight Keith needle are utilized to adhere the full-thickness graft to the underlying graft contours. If the graft area is large (>20% of the ear), we will use a surgical foam bolster that is secured with through-and-through 3–0 double-armed Prolene suture. This is kept dry and removed on the fifth postoperative day. Postoperative or oral antibiotics are not given; however, ciprofloxacin otic solution is given and the patient is instructed to liberally coat the sponge and healing graft for the first 3 postoperative days (▶ Fig. 19.4 and ▶ Fig. 19.5).
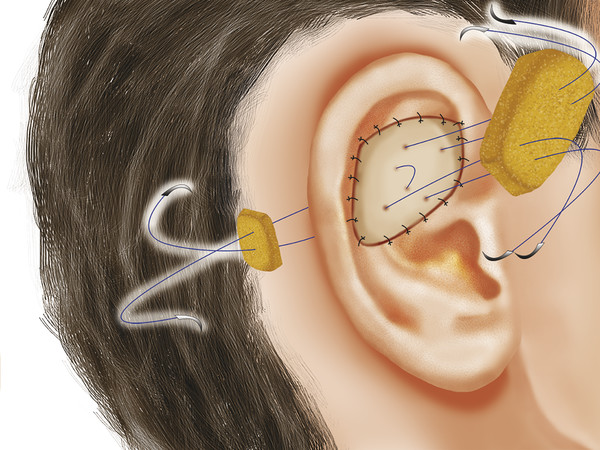
Fig. 19.4 Illustration of bolster placement following inset of full-thickness skin graft.
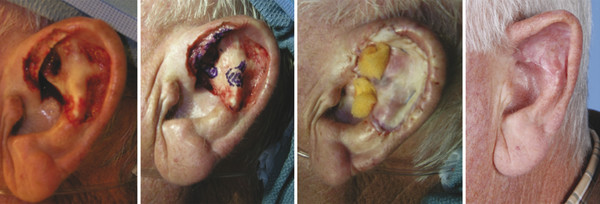
Fig. 19.5 A 60-year-old male status post 4 × 4 cm Mohs excision of melanoma in situ at left upper ear. Wound was repaired with color-matched full-thickness skin graft. Postoperative results shown at 2 months.
19.2.3 Local Flap Wedge or Local Flap Closure
We consider a simple wedge closure to a Antia–Buch type closure as techniques on a continuum that are performed from simple closure and alignment of the auricular rim to near-complete undermining, degloving of the ear, and advancement of bilateral chondrocutaneous flaps. 8, 9, 10 These can provide ideal postoperative results when executed for appropriately sized defects; however, it is important to proceed with caution. It is not uncommon to be able to get the two edges of the auricular rim approximated, but the resulting ear will have a significantly different shape and height than the unaffected ear on the contralateral side (▶ Fig. 19.6 and ▶ Fig. 19.7).
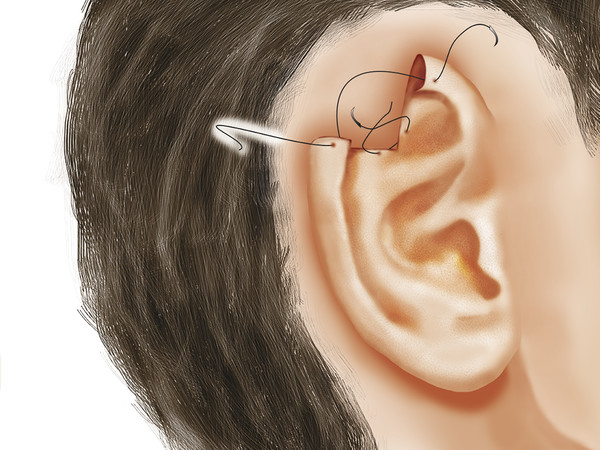
Fig. 19.6 Primary closure following wedge resection.

Fig. 19.7 A 49-year-old male status post 1 × 1 cm Mohs excision of basal cell carcinoma at right superior helical rim. Wound was closed with modified Antia–Buch advancement flap.
19.2.4 Folded Postauricular Two-Stage Ear Flap Reconstruction (Dieffenbach Flap)
For large segmental defects of usually the middle ear—although it can be applied to upper third defects also—the folded postauricular flap is exceedingly useful. 11, 12 This flap utilizes the non–hair-bearing postauricular skin that is elevated to the insertion of the ear into the scalp. It is also thickly elevated into the hair-bearing scalp in a slight wedge pattern to allow tucking of the ear and then the ear is simply tethered to the scalp with the skin overlying it. Vicryl 3–0 pop-off sutures are utilized to tether the cartilage portion of the ear to the scalp and then the remaining flap is simply inset with 5–0 either gut, or this is one instance where we will use chromic sutures on the ear. Nonstick dressings and antibiotic ointment are placed on the ear, which are removed on the second postoperative day. After 4 days, the patient may be allowed to shower and continue their daily activities, the only care required being a simple antibiotic dressing placed over the ear by the patient. 13 Understand that there have been numerous descriptions of complicated dressing techniques requiring nonstick dressings or red rubber catheters to maintain the separation on the ear, but in our experience with over 40 of these flaps, there have been no postoperative infections with simple antibiotic ointment and showering. 13 Since these are so well tolerated by the patient, and there is not that significant of an aesthetic deformity, the flaps are able to be left at a minimum of 3 and oftentimes up to 6 to 7 weeks for development of maximum vascularity. Understand that on division and inset, the skin can be simply folded on itself and sutured with through-and-through 4–0 double-armed Prolene sutures to restore the normal contour of the helical rim. No cartilage is required (▶ Fig. 19.8, ▶ Fig. 19.9, ▶ Fig. 19.10).
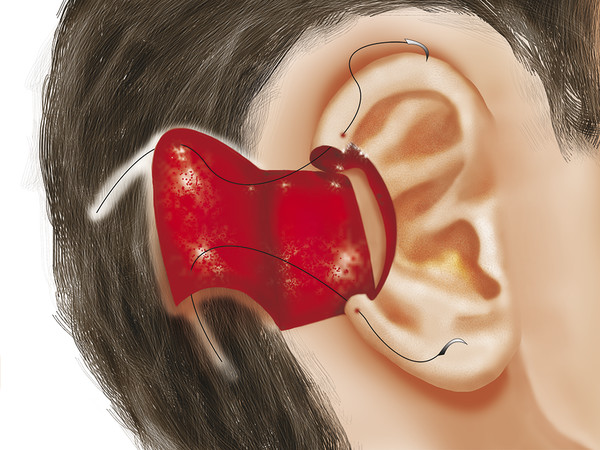
Fig. 19.8 Folded postauricular two-stage flap during initial flap elevation and inset.

Fig. 19.9 A 62-year-old male with middle third auricular rim skin and cartilage defect after Mohs resection. The third picture in the series shows flap after division and inset. Flap is folded on itself to recreate auricular rim with no additional cartilage support required. Scalp donor site is repaired with color-matched full-thickness skin graft.

Fig. 19.10 A 73-year-old male status post 4 × 3 cm Mohs excision of melanoma in situ at left antihelical rim. The lobe was then reconstructed with an anteriorly based transposition flap. Postoperative results shown at 10 months.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree