Features of particular processes20
FEATURES OF PARTICULAR PROCESSES
SIGNS OF PHOTOSENSITIVITY (Fig. 2.1)
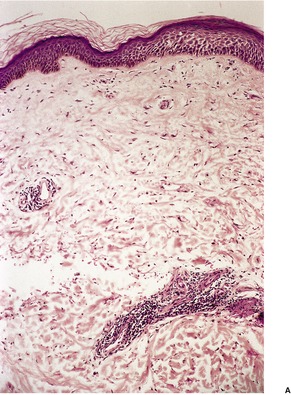
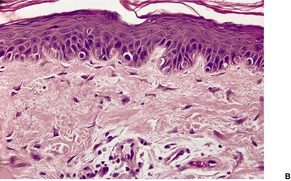
Fig. 2.1
SIGNS OF RUBBING/SCRATCHING (Fig. 2.2)
Acute, severe:
Pale pink epidermis, sometimes with loss of cell borders; pin-point erosions or larger ulcers; fibrin below the epidermis.
Chronic, persistent:
Psoriasiform epidermal hyperplasia; vertical streaks of collagen in the papillary dermis; stellate fibroblasts/dendrocytes; fibroplasia of varying amounts; enlarged follicular infundibula (as prurigo nodularis commences); compact orthokeratosis.
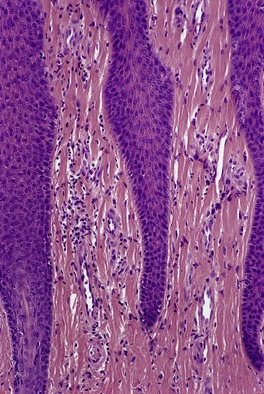
Fig. 2.2
SUBTLE CLUES TO DRUG REACTIONS
CLUES TO ELASTIC TISSUE ALTERATIONS
CLUES TO DEFICIENCY STATES
CLUES TO FUNGAL INFECTIONS (Fig. 2.3)
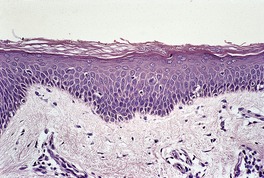
Fig. 2.3
SUBTLE CLUES TO A FOLLICULITIS (Fig. 2.4)
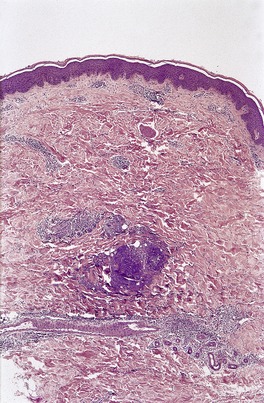
Fig. 2.4
‘LAST WEEK’S SIGN’ (Fig. 2.5)
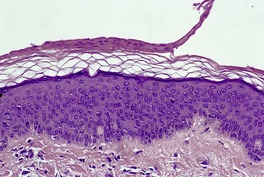
Fig. 2.5
LAGGING HISTOLOGY
HISTOLOGICAL FEATURES – WHAT DO THEY SUGGEST?
SUPERFICIAL AND DEEP INFLAMMATION (Fig. 2.6)
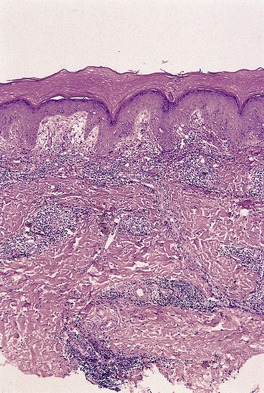
Fig. 2.6
8Ls
Drugs
A ‘BUSY’ DERMIS (Fig. 2.7)
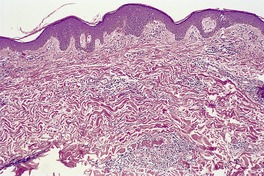
Fig. 2.7
ABSENT STRATUM CORNEUM
FILLED PAPILLARY DERMIS (Fig. 2.8)
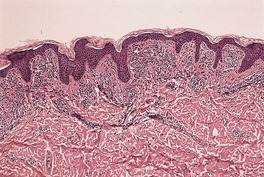
Fig. 2.8
PAPILLARY MICROABSCESSES (Fig. 2.9)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



Diagnostic clues
Signs of photosensitivity20
Signs of rubbing/scratching20
Subtle clues to drug reactions20
Clues to elastic tissue alterations20
Clues to deficiency states21
Clues to fungal infections21
Subtle clues to a folliculitis21
‘Last week’s sign’22
Lagging histology22
Histological features – what do they suggest?22
Superficial and deep inflammation22
A ‘busy’ dermis22
Absent stratum corneum23
Filled papillary dermis23
Papillary microabscesses23
Sparse perivascular neutrophils23
Thickened basement membrane23
Mid-dermal infiltrate and mucin24
Epidermotropism and exocytosis24
The epidermal/follicular ‘vacuum cleaner’24
Parakeratosis as a helpful sign25
Parakeratotic follicular lipping25
‘Chunks of coal’25
Interstitial eosinophils25
‘Bottom-heavy’ infiltrates26
The ‘bare underbelly’ sign26
Intraluminal giant cells/histiocytes26
Intravascular leukocytes26
High apoptotic (dyskeratotic) keratinocytes26
Vertical collagen bundles27
Loose pink fibrillary collagen27
Extravasated erythrocytes27
Pallor of epidermal cells27
Clear cell tumors27
Granular cell tumors28
Plexiform tumors28
Tumors with hemosiderin28
Clues to a particular disease29
Clues to herpes folliculitis29
Clues to Grover’s disease29
Clues to pityriasis rubra pilaris29
Clues to cicatricial pemphigoid29
Clues to epidermolysis bullosa acquisita29
Clues to mycosis fungoides29
Clues to alopecia areata30
Clues to androgenetic alopecia30
Late bullous lesions30
Granuloma annulare versus necrobiosis lipoidica30
Granuloma annulare versus lichen nitidus30
Clues to trichoepithelioma (over BCC)30
Clue to angiosarcoma30
Clues to Kaposi’s sarcoma30
Clues to bacillary angiomatosis30
Clues to amyloidosis30
Paraneoplastic dermatoses30
General helpful hints and cautions31
Beware of keratoacanthoma simulants31
Be cautious with amyloid stains31
‘Up it half a grade’31
‘Do serials, not deepers’31
Fungi may be missed on PAS stain31
Dermal neutrophils – often forgotten31
Itching ankles31
The demonstration of cryptococci32
The edge of Bowen’s disease32
False negative immunoperoxidase32
Miscellaneous hints32
Some of the clues that follow are original observations; many have been around for decades. An acknowledgement should be made here of the work of Bernard Ackerman, who has contributed more ‘clues’ to diagnostic dermatopathology than anyone else.
Like all ‘short cuts’, the following ‘clues’ must be used with caution. They are not absolute criteria for diagnosis and they are not invariably present at all stages of a disease. An attempt has been made to group the clues into several sections.
• Dilated vessels in the upper dermis
• Stellate fibroblasts/dendrocytes
• Deep elastotic fibers
• Deep extension of the infiltrate
• Epidermal ‘sunburn’ cells.
Photosensitivity reaction. (A) Note the mild telangiectasia, scattered stellate cells, deep extension of the infiltrate and mild deep solar elastosis. (B) Note the stellate cells. (H & E)
Note: The duration of the process and the underlying nature of the light reaction will influence the response. Only one or two features may be present, e.g. sunburn cells (apoptotic keratinocytes) are confined to phototoxic and photosensitive drug eruptions.
Chronic rubbing leading to vertical collagen in the papillary dermis and psoriasiform hyperplasia of the epidermis. (H & E)
• Superficial dermal edema
• Activated lymphocytes
• Eosinophils and/or plasma cells
• Red cell extravasation
• Endothelial swelling of vessels
• Exocytosis of lymphocytes
• Apoptotic keratinocytes.
The changes present will mirror the clinical types of reaction. In morbilliform reactions, lymphocytes extend into the lower epidermis and the apoptotic keratinocytes are in the basal layer.
• Small blue coiled/clumped fibers (pseudoxanthoma elasticum)
• Wavy epidermis (particularly in children)
• Elastophagocytosis
• Dispersed neutrophils (early cutis laxa)
• Unusually thickened collagen (connective tissue nevus).
• Confluent parakeratosis
• Superficial epidermal necrosis and/or pallor
• Mild psoriasiform hyperplasia
• Hemorrhage (in pellagra and mixed deficiencies).
Basically, these features should prompt the performance of a PAS stain. Many simulants exist.
Dermatophyte. The fungal elements are present in the region with compact orthokeratosis. Note the adjacent normal ‘basket-weave’ pattern. (H & E)
• Compact orthokeratosis with no other explanation
• Layering of epidermal cornification (‘sandwich sign’)
• Neutrophils in the epidermis/stratum corneum
• Spongiosis, particularly palmoplantar
• Suppurative folliculitis.
These signs refer to a likely folliculitis at deeper levels of the biopsy.
Folliculitis. There is deep dermal inflammation and an ‘uneven vasculitis’ more superficially. A ruptured and inflamed follicle was present on deeper levels. (H & E)
• Neutrophils on top of the stratum corneum
• Neutrophils at the edge of the tissue section
• Focal splaying of neutrophils and dust in mid dermis.
This refers to a dermatosis, no longer active, which is ‘playing itself out’. It was presumably more active some days earlier.
‘Last week’s sign’. The return to the production of normal basket-weave keratin beneath a layer of parakeratosis suggests there is little ongoing activity in this region. (H & E)
• Parakeratosis overlying basket-weave orthokeratin (the key feature)
• Mild hyperplasia of the epidermis
• Mild dermal inflammation.
This refers to several conditions in which the clinical appearances may be striking in comparison to the histology.
• Sclerodermoid GVHD may have ‘rock-hard skin’, but only subtle collagen deposition.
• Cicatricial alopecia can be similar.
• Urticaria – histology underestimates the edema because of dehydration during tissue processing.
• Prurigo nodularis – there may be clinical nodules but no histological swollen infundibula, only psoriasiform hyperplasia of lichen simplex chronicus.
• Pauci-cellular photodermatoses – there may be striking clinical changes but only telangiectasia and sparse inflammatory cells on histology.
The presence of a superficial and deep inflammatory cell infiltrate within the dermis should trigger the mnemonic ‘8Ls + DRUGS’.
A superficial and deep dermal infiltrate. This is one of the ‘L’ diseases – polymorphiclight eruption. (H & E)
• Light reactions
• Lymphoma
• Leprosy
• Lues
• Lichen striatus
• Lupus erythematosus
• Lipoidica (necrobiosis)
• Lepidoptera (and other arthropods)
• Dermatophyte
• Reticular erythematous mucinosis
• Urticarial stages (bullous pemphigoid)
• Gyrate erythemas
• Scleroderma (localized)
• And, of course, drug reactions
‘Busy’ refers to a dermis that appears focally hypercellular on scanning magnification and is not usually due to the usual inflammatory infiltrates.
A ‘busy’ dermis. There is hypercellularity in this case of interstitial granulomatous drug reaction. (H & E)
• Incomplete form of granuloma annulare
• Interstitial granulomatous dermatitis
• Interstitial granulomatous drug reaction
• Resolving vasculitis (increased mucin also)
• Chronic photodermatoses
• Folliculitis – at deeper levels (cells are neutrophils and dust)
• Desmoplastic melanoma (also perivascular lymphocytes)
• Kaposi’s sarcoma (early stage).
• Staphylococcal scalded skin syndrome
• Pemphigus foliaceus
• Peeling skin syndrome
• Psoriatic erythroderma (psoriasiform hyperplasia present)
• Artifacts.
The low power impression is that of a variably hypercellular papillary dermis. Excluded from consideration are nodular and diffuse infiltrates also involving the reticular dermis. The ‘LUMP’ mnemonic covers most cases: lichenoid, urticaria pigmentosa, mycosis fungoides, pigmented purpuric dermatoses. Expressed differently they are:
• Most of the lichenoid tissue reactions
• Pigmented purpuric dermatoses
• Cutaneous T-cell lymphoma
• Parapsoriasis (if not included above)
• Some mastocytomas
• Early lichen sclerosus et atrophicus.
The papillary dermis is filled. This is mastocytosis. (H & E)
• Dermatitis herpetiformis
• Linear IgA disease
• Cicatricial pemphigoid
• Localized cicatricial pemphigoid
• Bullous lupus erythematosus
• Epidermolysis bullosa acquisita
• Drugs
• Hypersensitivity vasculitis (rare)
• Rheumatoid neutrophilic dermatosis
• Pemphigoid gestationis (eosinophils)
• Deep lamina lucida pemphigoid





