Chapter 19 Diagnosis and treatment of inhalation injury
![]() Access the complete reference list online at http://www.expertconsult.com
Access the complete reference list online at http://www.expertconsult.com
![]() IN THIS CHAPTER
IN THIS CHAPTER ![]() Video Content Online • PowerPoint Presentation Online
Video Content Online • PowerPoint Presentation Online
Introduction
Inhalation injury is a non-specific term that refers to damage to the respiratory tract or pulmonary parenchyma by heat or chemical irritants carried into the airways during respiration. Inhalation injury remains one of the most critical injuries following thermal insult. It may occur in conjunction with cutaneous burns or in isolation. The severity of injury varies, depending on the chemical composition of the agent(s) inhaled, the intensity of exposure, temperatures reached during combustion and pre-existing comorbidities. There are three basic classes of inhalation injury: direct thermal injury, tissue damage due to inhalation of chemical irritants, and systemic effects of inhaled toxins. Direct thermal injury is generally restricted to the upper airway and rarely involves subglottic structures.1 The upper airway serves as an efficient heat exchanger that protects lower structures from extremes of heat or cold. Laryngeal closure also protects subglottic areas. Exceptions are the inhalation of steam due to the much higher specific heat of water vapor, and blast injuries that can force hot gases past the glottic opening. Inhaled irritants are generally present in smoke as a mixture of gases, fumes, and mists, and the chemical composition of smoke produced from various fuels has been described.2 Fumes consist of particles of various size dispersed in inhaled gases. Mists are aerosolized liquids. The intensity of exposure along with the size and chemical composition of these particles and droplets determines how far distally they will migrate in the respiratory tract and the nature of the tissue injury.2 Large particles and droplets of lipid-soluble liquids are more likely to adhere to airway surfaces and do not reach as far distally as smaller particles and more water-soluble droplets. Systemic toxicity occurs when toxins such as carbon monoxide or cyanide are present in the inhaled gases.
The reported incidence of inhalation injuries has varied greatly over time and from region to region. Smith3 and others reported 19.6% incidence among burn patients in the USA, in Israel Haik4 and colleagues found as few as 1.5%, while Luo5 and others found 8.01% in China. Regional differences are to be expected as a result of differences in local customs, building materials, and other factors.
The presence of inhalation injury is clinically significant for a variety of reasons, as listed in Table 19.1. Inhalation injury has been found to be an independent risk factor for mortality.6,7 It is also associated with hemodynamic instability, as volume requirements for resuscitation may be increased by as much as 50% when cutaneous burns are accompanied by inhalation injury.8 Parenchymal injury can lead to impaired gas exchange, pneumonia, and ARDS. When severe, these changes increase the risk of multiorgan failure and mortality. After recovery from inhalation injury pulmonary function disorders may persist due to pulmonary fibrosis or bronchiectasis. Improvements in the survival of patients with inhalation injury have been attributed to better overall burn outcomes, improved ventilatory management, and improved management of pneumonias.5
Table 19.1 Clinical significance of inhalation injuries
Diagnosis
As stated above, inhalation injury is a non-specific term used to describe injury to the airways and/or lungs due to the inhalation of gases that are either hot or contain chemical irritants, or both. There is no consensus on the diagnostic criteria for inhalation injury. In the clinical setting the diagnosis is a relatively subjective judgment based on history and physical examinationination, and often confirmed by additional diagnostic procedures such as bronchoscopy. One of the reasons for the lack of consensus is that impaired pulmonary function due to inhalation injury often results from an inflammatory response to the initial injury, and manifestations may be delayed for a day or two. In addition, it is our clinical impression that progressive respiratory failure is not necessarily proportional to the intensity of smoke exposure.9 It is also possible for thermally injured patients to experience acute lung injury from the systemic effects of the inflammatory response to severe cutaneous burns.10 Thus, it is not uncommon to see acute lung injury in patients with large scald burns.11 This makes it difficult to determine what component of respiratory failure is due to inhalation injury in patients with large burns.
On initial presentation, patients with inhalation injury may have relatively normal gas exchange as evaluated by arterial blood gas analysis, and the chest radiograph is usually normal.12 In the absence of evidence of respiratory distress it is important to recognize features from the history and physical examination that reveal risk factors for inhalation injury. Early diagnosis is important to recognize the potential for airway compromise, manage fluid resuscitation, and to recognize systemic toxicity that may lead to permanent neurological deficits if not promptly treated.
History of the mechanism of injury is especially important in the case of scalds due to ingestion of hot liquids. Although patients may appear asymptomatic initially, oropharyngeal scalds have led to fatal airway occlusion. Intraoral scalds can present in a manner similar to epiglottitis.13 The larynx should be examined for evidence of compromise in all patients who present with significant risk of intraoral scald.
The physical examination reveals additional risk factors for inhalation injury. We guard our face vigorously, and the presence of burns to the face or singed eyebrows or nasal hair implies a very intense exposure. When gases hot enough to burn tissue are near the airway it suggests that oropharyngeal or nasopharyngeal structures may also suffer thermal injury. Soot deposits on the face and carbonaceous sputum suggests intense exposure to and inhalation of smoke. Physical examination may reveal signs and symptoms such as stridor, hoarseness, drooling, and dysphagia that are considered classic evidence of inhalation injury. These findings, however, do not always indicate that tracheal intubation is necessary.14 However, as described below, when patients are considered at risk for upper airway thermal injury and occlusion, a priority is to evaluate the upper airway for impending occlusion that may be prevented by early tracheal intubation.
The chest radiograph is also considered an insensitive indicator of parenchymal injury after smoke inhalation. Although an admission chest radiograph should be obtained in all patients suspected of inhalation injury, it has been recognized that a normal study does not rule out the possibility of significant pulmonary injury.12
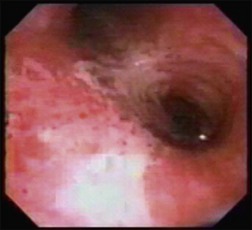
Flexible fiberoptic bronchoscopy was early recognized as a powerful tool in the diagnosis of inhalation injury.15 Fiberoptic bronchoscopy allows direct visualization of tissue damage to the upper airway and bronchi by heat and chemical irritants. This procedure can quickly and reliably identify patients with upper airway compromise who will benefit from intubation.16 Bronchoscopic evidence of inhalation injury includes soot deposits, erythema, edema (as indistinct tracheal rings or blunting of the carina), mucosal blisters and erosions, hemorrhages, and bronchorrhea (Fig. 19.1).
Flexible fiberoptic bronchoscopy has been considered the ‘gold standard’ and is often used to confirm the diagnosis of inhalation injury.17 However, Hunt noted that in some cases bronchoscopy performed soon after injury may not show mucosal injury.15 In addition, because acute lung injury and tracheobronchitis can be a result of systemic inflammation due to cutaneous burns,10,11 endoscopic changes after 36–48 hours may be caused by mechanisms other than inhalation of chemical irritants. Moreover, although fiberoptic bronchoscopy can definitively identify tissue damage from inhalation injury, it has been recognized that the observed changes are relatively proximal and may be more severe than more peripheral, parenchymal injuries.18 As a result, a bronchoscopic diagnosis of inhalation does not always identify which patients will experience progressive respiratory dysfunction.
Radionuclide studies have been used to provide evidence of pulmonary injury distal to the more proximal views permitted by flexible bronchoscopy. Intravenously administered xenon-133 is excreted by the lungs and exhaled. Delayed clearance of xenon-133 is a sensitive indicator of inhalation injury.19 More recently, lung scintigraphy using technetium-99 aerosol inhalation has been used to identify areas of pulmonary dysfunction in patients with respiratory dysfunction after smoke inhalation. Delayed clearance and inhomogeneous lung distribution of radioactivity are evidence of injury.20 These studies are sensitive indicators of inhalation injury, but interpretation can be confounded by pre-existing lung disease and it may be difficult to perform these studies in critically ill burn patients.
Pathophysiology of pulmonary insufficiency with inhalation injury
As stated above, except in special cases such as inhalation of steam, injury to airways below the larynx and pulmonary parenchyma nearly always results from chemical irritation. A number of reviews are available to describe the pathophysiology of pulmonary failure associated with smoke inhalation.2,21 Chemicals inhaled with smoke as well as carbon particles coated with irritants are deposited in the airways. Aqueous secretions of the mucosa dissolve these irritants and the respiratory mucosa is bathed in relatively concentrated caustic solutions. The initial response to this insult is injury to the respiratory epithelium, resulting in hyperemia, edema, increased mucous secretions, impaired ciliary clearance, and bronchoconstriction. Work in experimental animals has also demonstrated an early separation of ciliated respiratory epithelial cells from the basement membrane. This results in denuded areas of the airways and explains the copious formation of protein-rich exudate. Fibrin casts tenaciously adherent to the airway surfaces are formed from this exudate.
Airways become blocked by edema, bronchoconstriction, fibrin casts, necrotic debris, and inflammatory infiltrate (Fig. 19.2). Degraded surfactant causes alveolar instability and collapse. These changes result in impaired hypoxic pulmonary vasoconstriction and areas of atelectasis, and postobstructive sequestration of material that provide a medium for bacterial growth and risk of pneumonia. Impaired function of alveolar macrophages slows the removal of these materials and facilitates the development of infection. Pulmonary compliance is reduced, which can greatly increase the work of breathing.
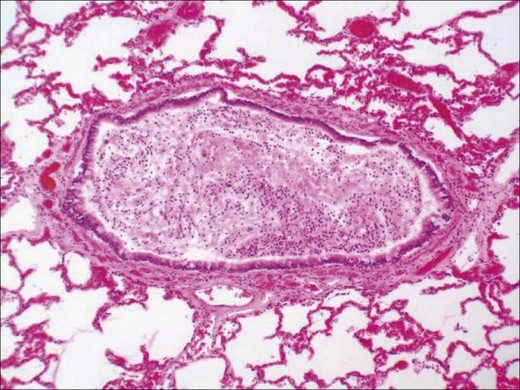
Figure 19.2 Small airway occluded by inflammatory exudate in a patient who had a smoke inhalation injury.
As a result of these changes pulmonary gas exchange is impaired. Atelectasis due to airway obstruction increases dead space and shunt to an extent, but the impaired gas exchange due to smoke inhalation appears to be primarily a ventilation–perfusion imbalance.22 It has been suggested that this mechanism of pulmonary dysfunction is fundamentally different from other types of ARDS.17,23 Other etiologies of ARDS, such as sepsis, involve disruption of the pulmonary capillary membrane and alveolar flooding, resulting primarily in true shunt. This distinction can influence the ventilator strategies employed. Patients with respiratory failure due to smoke inhalation injury have small airway obstruction, and care should focus on pulmonary toilet together with recruiting and stabilizing alveoli, which tend to collapse, whereas in ARDS due to other etiologies the strategy is to concentrate on avoiding ventilator-induced lung injury. In some burn centers this is a rationale for the use of high-frequency percussive ventilation.17
Just as the bronchi are the focus of the diagnosis of inhalation injury, it is also the focus of its pathology.24 The hyperemia and edema that are seen in the airway and which are so important for the diagnosis of inhalation injury are the result of an almost 20-fold increase in bronchial blood flow.25,26 Following the airway injury, there are changes in the lung parenchyma. There is a release of the chemokine interleukin (IL)-8 and an influx of neutrophils into the airway and alveoli. Reactive oxygen (ROS) and nitrogen species (RNS) are formed.27 One of the latter, peroxynitrite, damages DNA. DNA damage results in activation of poly-(ADP ribose) polymerase.28 Poly-(ADP ribose) protects the damaged DNA but also activates the nuclear factor NF-κB.29 This causes the formation of the inducible form of nitric oxide synthase and additional release of IL-8, attracting and activating additional neutrophils and forming more reactive nitrogen and oxygen species.30 The oxidation, nitration, and nitrosation of lung tissues results in membrane damage, edema formation and impaired oxygen diffusion.31,32 Alveoli that are not ventilated are not perfused with blood because alveolar hypoxia causes pulmonary vasoconstriction. NO released by nitric oxide synthase causes a loss of hypoxic pulmonary vasoconstriction, leading to perfusion of unventilated alveoli and thus a fall in arterial oxygen saturation.33
Ablation of the bronchial blood flow will prevent most of the pathophysiology involved in inhalation injury to the pulmonary parenchyma.24,34,35 These changes in bronchial blood flow are not associated with heat. They can be produced in experimental animals by smoke that has been cooled to body temperature.36 As mentioned above, the blood flow to the airway is so effective in cooling or heating inhaled air that it is almost impossible for hot gases to reach the bronchi.36,37 These changes in blood flow also appear to be independent of the chemical composition of smoke, as they are mediated by a neuroinflammation. We have recently reported that following insufflation of smoke into deeply anesthetized sheep, the airway blood flow increased 10-fold, but after administration of an inhibitor of the neuropeptide calcitonin gene-related peptide (CGRP) the smoke-induced hyperemia was markedly reduced.38 Neuropeptides (peptides released from nerves within the lung tissue) induce vasodilatation by causing activation of nitric oxide synthase, leading to the formation of NO. It has also been reported that an inhibitor of the neuro isoform of nitric oxide synthase would block the hyperemia and much of the pathophysiology mentioned above, including the loss of hypoxic pulmonary vasoconstriction.39,40 These findings have led us to the following hypothesis: the chemicals in smoke activate sensory nerves to release neuropeptides that activate NOS1 to release NO and superoxide to form peroxynitrite, which damages DNA, activating PARP, that stimulates NF-κB which in turn will upregulate the inducible form of nitric oxide synthetase, leading to massive formation of ROS and RNS, tissue damage and hypoxia and dyspnea. Some of the activated polymorphonuclear cells that escape from the pulmonary and bronchial circulation into the systemic circulation are carried to systemic organs, promoting multiorgan system damage.
Treatment
Initially, special attention must be given to the airway evaluation. There are many potential indications for early and even prophylactic intubation in victims of serious burn injury (Table 19.2). Early hypoxemia due to impaired gas exchange after inhalation injury is an ominous sign, and those with respiratory distress not corrected by supplemental oxygen may require intubation. Patients unable to protect their airway owing to diminished mental status due to injury or intoxication should be intubated to prevent aspiration. It is recommended that, even in the absence of inhalation injury, those with large burns covering 40% or more of their total body surface area (TBSA) should be intubated because of the risk of associated hemodynamic instability.17
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree