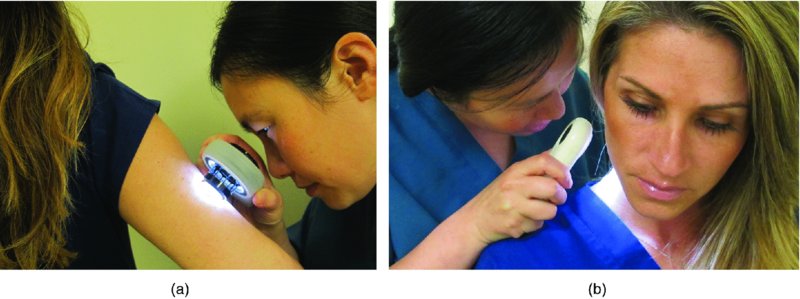
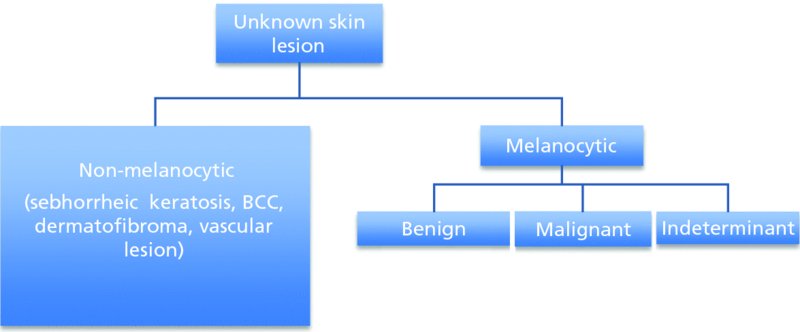
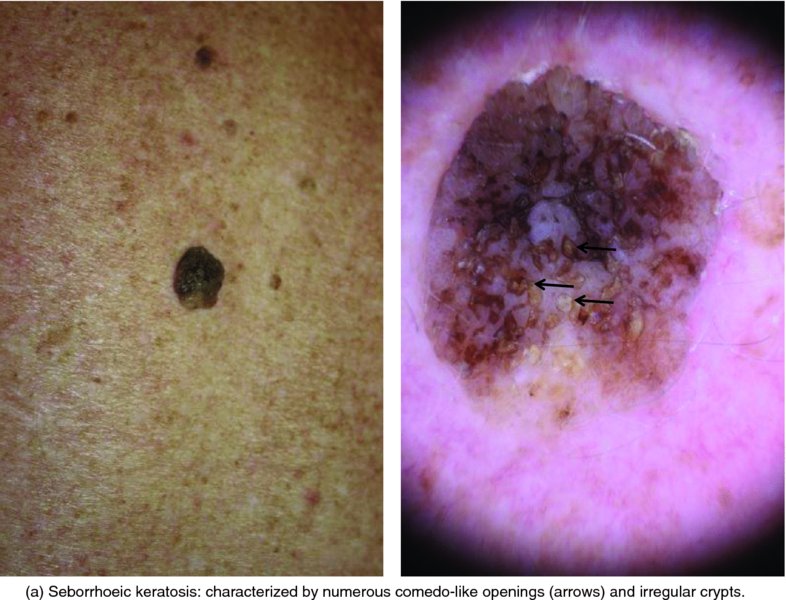
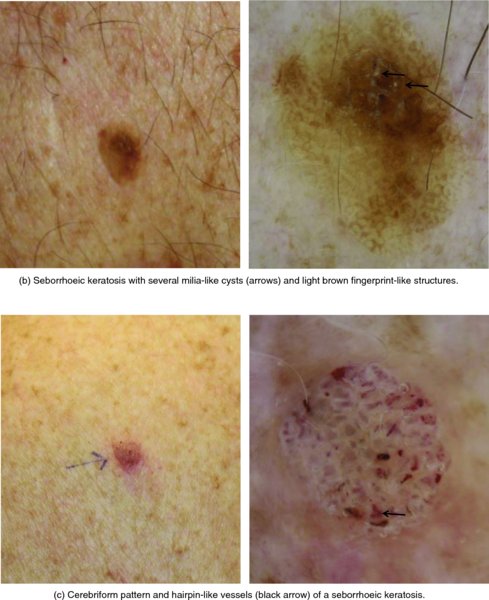
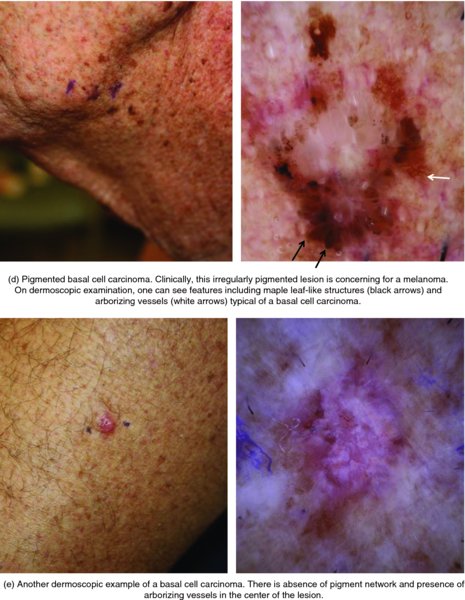
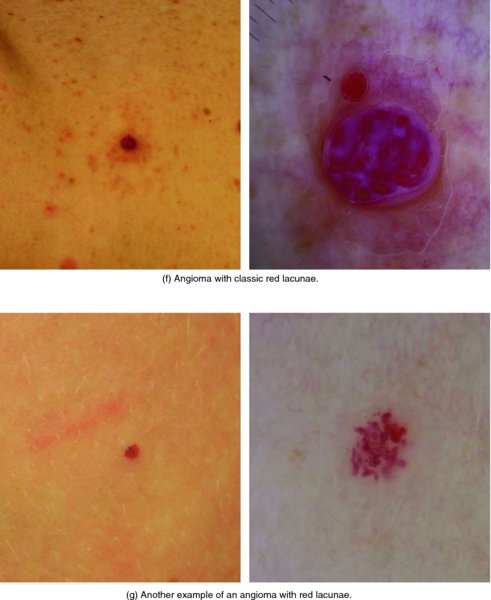
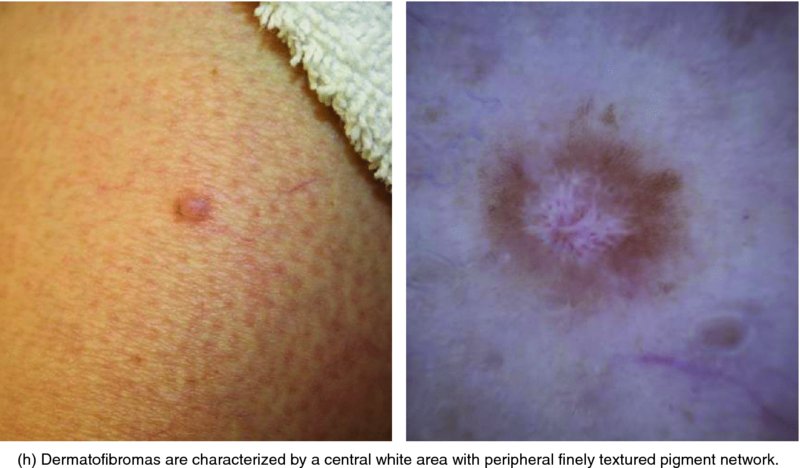
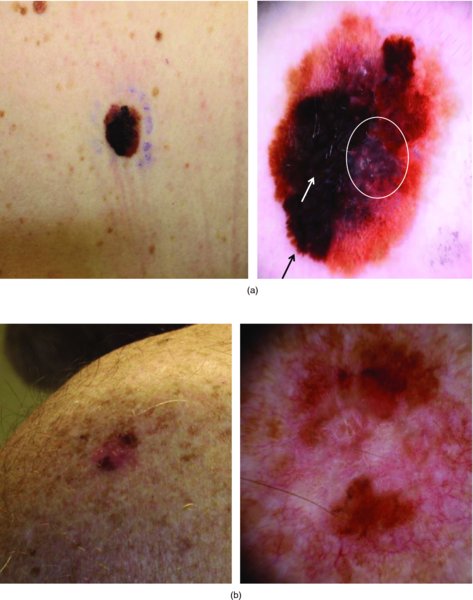
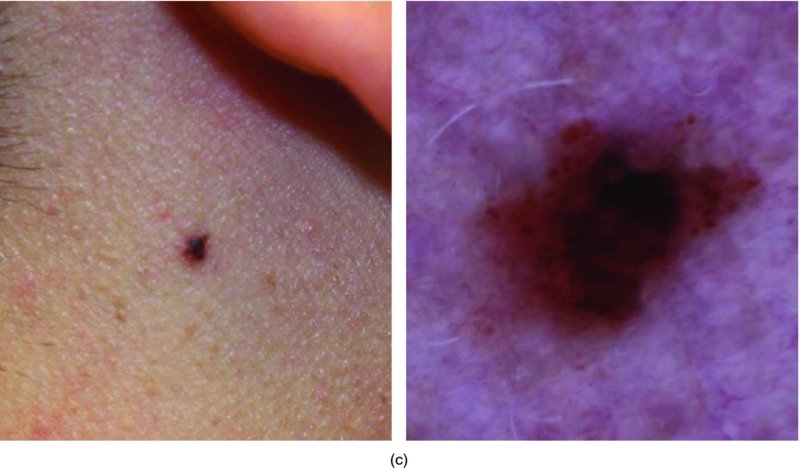
28 Dermoscopy, also termed epiluminescence microscopy or skin surface microscopy, has been used since the 1900s by dermatologists as a non-invasive in vivo diagnostic technique to aid in early diagnosis of melanoma. Dermoscopy helps to differentiate melanomas from benign naevi and from mimickers such as pigmented basal cell carcinoma, seborrhoeic keratoses or haemorrhages under the skin. A meta-analysis published in 2008 showed that, among dermatologists, dermoscopy increased diagnostic accuracy in pigmented skin lesions (90% diagnosed melanoma correctly versus 74% without dermoscopy), without any difference in specificity. One randomized trial of dermatologists trained in dermoscopy demonstrated a 42% reduction in unnecessary biopsy compared with those using naked eye examination alone. Dermoscopy has also been shown to be increasingly useful in the diagnosis of a variety of other dermatological conditions. It can aid in finding burrows in scabies, locating a splinter, evaluating alopecia and evaluating nail fold capillaries in systemic sclerosis. A dermascope consists of a hand-held device with magnification (usually 10- to 20-fold) and a light source (Figure 28.1). A digital imaging system can be attached for photographic documentation. A dermascope renders the stratum corneum translucent to allow for the examination of the subsurface morphological details of the skin. It enhances the microstructures in the epidermis, dermo-epidermal junction and papillary dermis, allowing clinicians to identify specific features that correspond to benign and malignant pigmented skin lesions (Table 28.1). Two methods are commonly used to accomplish this: cross-polarized light and contact immersion system. With contact immersion dermoscopy, the dermoscope is placed directly on the skin along with an immersion fluid (mineral oil, ultrasonic gel, alcohol or water) to reduce reflection and refraction of light from the stratum corneum. Alternatively, the use of cross-polarized light eliminates the use of immersion fluid and the need for direct contact with the skin which reducing the risk of cross-contamination between patients. Newer hybrid devices allow for both polarized and contact immersion examination (Figure 28.2). Table 28.1 Typical dermoscopic features of skin lesions. Figure 28.1 Hand-held dermascopes. Figure 28.2 Physician examining a pigmented lesion using a contact immersion system (a) and cross-polarized light which does not require direct contact (b). Dermoscopic evaluation is a two-step process (Figure 28.3). The first step in dermoscopic evaluation is to determine whether a lesion is of melanocytic origin. Melanocytic lesions, basal cell carcinomas, seborrhoeic keratoses, dermatofibromas and vascular lesions have unique dermoscopic features (see Table 28.1; Figure 28.4). In general, melanocytic lesions have pigment network with dots, globules or streaks, and blue–grey pigmentation. If the lesion does not have any of these melanocytic features and does not have any features of non-melanocytic lesions listed in Table 28.1, it is considered melanocytic by default. Of note, lesions present on facial, acral and mucosal sites may demonstrate site-specific dermoscopic features; a full discussion of these more complex sites may be found in a dedicated advanced dermoscopy text. Figure 28.3 Two-step dermoscopic evaluation. BCC, basal cell carcinoma. Figure 28.4 Typical dermascopic appearance of non-melanocytic lesions. Figures courtesy of Dr. Kelly Nelson, Department of Dermatology, Vanderbilt University, Nashville, Tennessee, USA.
Dermoscopy
Melanocytic lesion
Pigment network
Dots and globules
Streaks
Parallel pattern of pigment (on acral skin)
Blue–grey pigmentation
Lack of any specific dermoscopic features
Seborrhoeic keratosis
Milia-like cysts
Comedo-like openings
Light-brown fingerprint-like structures
Fissures/ridges/irregular crypts
Basal cell carcinoma
Absent pigment network
Arborizing vessels
Maple leaf-like areas
Blue–grey ovoid nests/globules
Spoke wheel areas
Superficial ulceration
Vascular lesion
Red–blue lacunas
Red–blue to red–black homogenous areas
Dermatofibroma
Peripheral finely textured pigment network
Central white area
Dermoscopic evaluation

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








