■ Perforators to the lower abdominal skin and adipose tissue come off the pedicle at multiple levels and are referred to as medial or lateral rows of perforators, indicating their relative position within the rectus/entry point into the flap.
■ Most perforators are found within a 10-cm radius from the umbilicus.
■ Zones of perfusion based on fluorescent perfusion studies9 are illustrated in FIG 2—illustration with zones transposed onto rectus/pedicle.
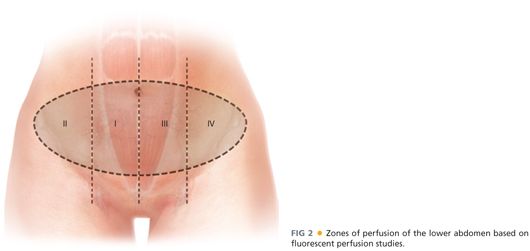
■ In general, perfusion of the hemiabdominal flap ipsilateral to the perforators (zones I and II) is stronger than it is to the contralateral abdominal flap across the midline (zones III and IV).
■ Medial row perforators have a greater likelihood of perfusing tissue across the midline than do lateral row perforators.
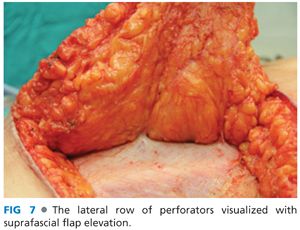
■ In contrast, lateral row perforators have a greater likelihood of perfusing the most lateral extent of the ipsilateral hemiabdominal flap than do medial row perforators.
■ Medial and lateral rows of perforators communicate via a subdermal plexus.
■ There is also communication between DIEA and DIEV system and the superficial inferior epigastric artery (SIEA) and superficial inferior epigastric vein (SIEV) system.
■ The SIEV is the dominant outflow vessel for the lower abdomen in many patients.
PATIENT HISTORY AND PHYSICAL FINDINGS
■ A thorough history and physical examination are critical in preparing for reconstruction.
■ Pertinent aspects of the history include previous abdominal or chest wall operations and medical conditions that would preclude patients from a lengthy operation under general anesthesia.
■ A focused abdominal examination evaluating the amount of lower abdominal adipose tissue and the location of surgical scars if present
■ A team-based approach involving surgeons, anesthesiologists, primary care physicians, and other specialists such as cardiologists, as needed, ensures that patients are evaluated as a whole and all key concerns are addressed.
IMAGING AND OTHER DIAGNOSTIC STUDIES
■ Preoperative computed tomography (CT) angiography of the donor site has been advocated in recent years. The preoperative scans provide a road map for flap perforators, with information on perforator location, size, and distribution (FIG 3).
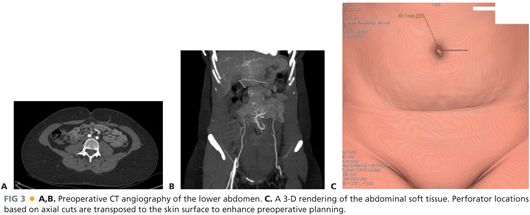
■ In patients with long low transverse abdominal incisions, the scans also allow for the assessment of continuity of the flap pedicle beyond the incision.
■ Information gathered from scans has been shown to decrease operative times.10 CT scans, however, are not an absolute requirement for preoperative planning.
SURGICAL MANAGEMENT
■ In consulting with patients, decisions about the timing of reconstruction (immediately after mastectomy or delayed) and the type of reconstruction are made, taking patient factors and tumor characteristics into consideration.
■ Patient factors of significance include the following:
■ Patient preference
■ Body habitus or the availability of abdominal donor tissue
■ Body mass index
■ Smoking history
■ History of previous abdominal operations that compromise the vascular pedicle or donor site
■ Medical comorbidities that would preclude patients from undergoing a lengthy operation
■ Tumor characteristics as they relate to the following:
■ The need for postmastectomy radiation therapy or
■ The need for close postmastectomy surveillance prior to reconstruction
■ In general, patients known to require postmastectomy radiation therapy are reconstructed in a delayed fashion to avoid the detrimental effects of radiation on flaps. A history of radiation therapy also serves as a relative indication for use of an autologous form of reconstruction, as implant reconstructions in the setting of radiation are prone to higher rates of complications and failure.
Preoperative Planning
■ In addition to basic labs, patients should be type and screened, particularly in cases of bilateral reconstructions.
■ All anticoagulant and antiplatelet medications should be stopped a week prior to the operation. Warfarin can be bridged with enoxaparin also a week prior.
■ Smokers are required to quit for a minimum of 4 weeks prior.
■ Patients receive preoperative antibiotics with intraoperative redosing.
■ Patients receive deep vein thrombosis (DVT) prophylaxis with use of a pneumatic compression device and subcutaneous heparin at the beginning of the case.
Positioning
Marking/positioning
■ Preoperative markings of the breast and abdomen are performed with the patient in the upright position.
■ Key landmarks for the breast marked are the chest midline, inframammary fold, and a periareolar marking in the case of a skin-sparing mastectomy. The breast base width is also measured (FIG 4A).
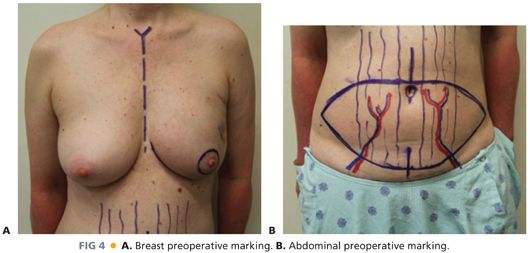
■ The upper marking for the abdominal flap is made at or just above the umbilicus with the location of perforators on preoperative imaging, providing some guidance. The breast base width is used to mark the potential vertical height/distance from the upper marking to the lower marking. The lower marking is then made to complete the elliptical pattern (FIG 4B).
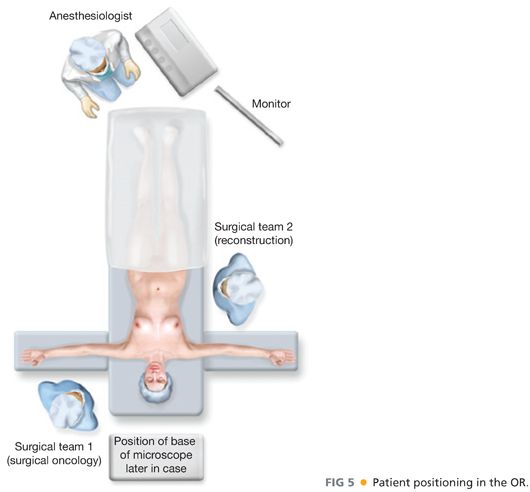
■ Patient positioning in the operating room (OR) is supine and the table is turned 180 degrees from the anesthesiologist, providing better access for two surgical teams (FIG 5).
TECHNIQUES
FLAP HARVEST
■ Skin preparation with clipping is performed as needed.
■ The breasts and abdomen are prepped and draped in a sterile fashion.
■ The upper abdominal incision is made with a scalpel, and dissection through the adipose tissue down to anterior abdominal wall fascia is performed with electrocautery.
■ An adipocutaneous flap is elevated cephalad with the electrocautery, ending at the xiphoid centrally and at the costal margins laterally. Less elevation may be needed in patients with ample skin laxity.
■ The OR table is reflexed and the raised upper abdominal flap is transposed downward to assess the ability of this skin edge to meet the lower abdominal markings for closure. The lower abdominal markings are at this time adjusted as needed and the table returned to its original position.
■ The lower abdominal incision is made superficially with a scalpel and careful dissection through the adipose tissue is performed, anticipating the presence of the SIEA and SIEV, typically above Scarpa’s fascia (FIG 6).
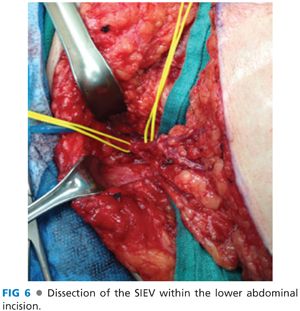
■ Once the superficial vessels are visualized, a Weitlaner retractor is introduced to provide further exposure and the vessels are dissected out toward the femoral vessels with use of tenotomy scissors and bipolar electrocautery. In patients who are not good candidates for the SIEA flap (SIEA) based on the absence of adequate-sized vessels, the vein is dissected to a length greater than or equal to 5 cm prior to ligating it with hemoclips and dividing it.
■ Dissection down to the anterior abdominal wall fascia is then completed with electrocautery.
■ Flap elevation is performed in the suprafascial plane from lateral to medial with electrocautery until the lateral row of perforators are encountered just medial to the edge of the rectus fascia (FIG 7).
■ An incision is made around the umbilicus and along the midline of the flap in bilateral reconstruction cases or in cases with hemiabdominal flaps large enough for a unilateral reconstruction.
■ The umbilical stalk is dissected out with blunt-tipped scissors and division of the flap down the midline is completed with electrocautery.
■ In unilateral reconstructions that require use of portions of the flap that cross the midline, the umbilicus is dissected out without splitting the flap.
■ Suprafascial elevation of the flap from its medial edge is performed with electrocautery until the medial row of perforators are encountered.
■ Dissection around the perforators is performed with a low-energy electrocautery, and at this time, all perforators are assessed for their size and location within the flap.
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








