Deep Inferior Epigastric Artery Perforator Flap Breast Reconstruction
Mark W. Clemens
Maurice Y. Nahabedian
Background
The search to find the ideal type of reconstruction following breast cancer has led to an evolution in techniques that attempt to restore the “normal breast.” Theoretically the ideal reconstruction would restore “like with like,” giving the breast a natural texture and feel. The cost to the patient in donor site would be minimal or potentially even beneficial. Pedicled or free musculocutaneous flaps have traditionally been used for autogenous breast reconstruction with inherent sacrifices to donor sites (1,2). The recent development of perforator flaps has made possible the reliable transfer of skin and fat with minimal donor-site morbidity (3). For the reconstruction of mastectomy defects, the abdominal perforator flap has become a mainstay among reconstructive microsurgeons. The deep inferior epigastric artery perforator (DIEP) flap as introduced in 1989 and popularized in 1994 can produce a soft, natural-appearing breast with an improved abdominal contour and without muscle or fascia sacrifice (4,5). This has led to a decreased incidence in abdominal bulge, hernia, and weakness (6).
Anatomy
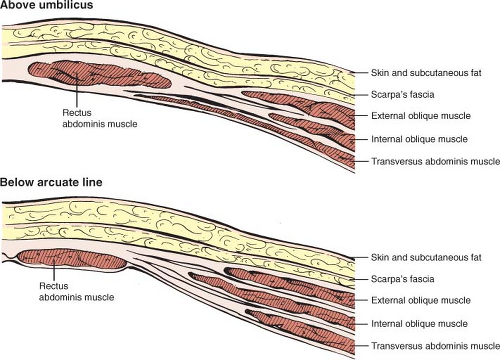
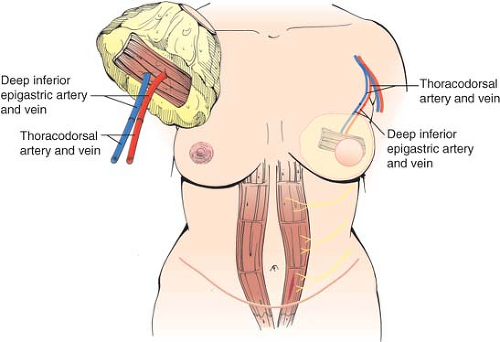
The DIEP flap is an adipocutaneous flap that is derived from the lower abdomen. The anatomic layers of the anterior abdominal wall include the skin, subcutaneous fat, superficial fascia layer (Camper’s), a deeper membranous fascia layer (Scarpa’s), anterior rectus sheath, abdominal musculature with aponeuroses and fascial sheaths, posterior rectus sheath and preperitoneal fat, transversalis fascia, and the peritoneum. The paired muscles of the anterior abdominal wall are the external oblique, internal oblique, transverse abdominis, and the rectus abdominis muscles (Fig. 65.1). The rectus abdominis muscle is enveloped by a fascial sheath composed anteriorly by the aponeurosis of the external oblique and half of the internal oblique and posteriorly by the aponeurosis of the other half of the internal oblique and the transverse abdominis muscles (Fig. 65.2). The arcuate line (linea semicircularis) runs horizontally across the lower one fourth of the rectus abdominis muscle and represents the lower border of the rectus sheath. The rectus sheath does not have a posterior component below this line.
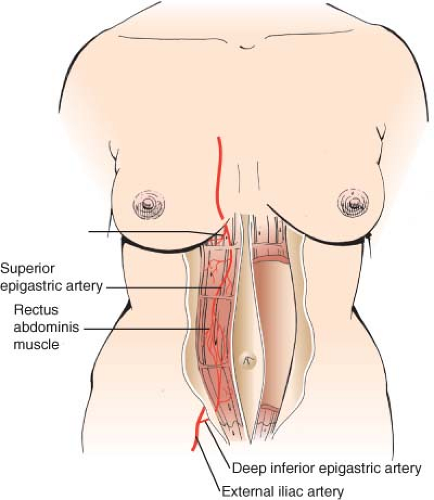
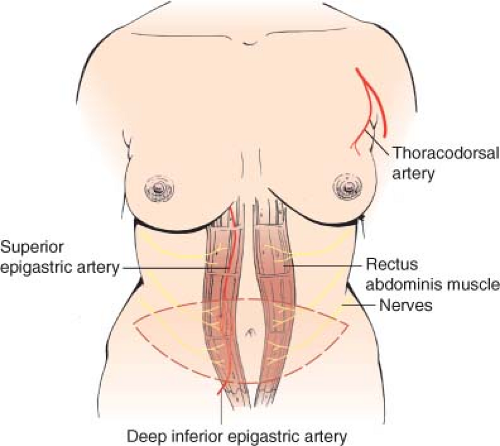
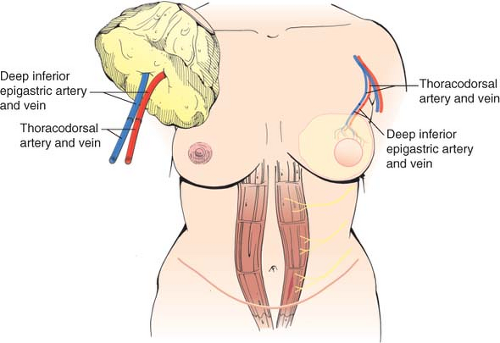
The vascularity of the DIEP flap is derived from the deep inferior epigastric vessels, which are a branch of the external iliac artery and vein (Fig. 65.3). The deep system has multiple perforators that supply the anterior abdominal wall (Fig. 65.4). The DIEP flap is usually designed to incorporate one to three of these perforators. The deep inferior epigastric artery courses along the posterior surface of the rectus abdominis and enters either the lower (17%), middle (78%), or upper (5%) one third of the muscle (7). The flap is raised by following these perforators to a single pedicle with preservation of the rectus muscle and rectus sheath (Fig. 65.5). Two venae comitantes usually accompany the artery.
The harvest of an abdominal free flap can be thought of as on a continuum between a transverse rectus abdominis myocutaneous (TRAM) flap and a perforating flap (DIEP). DIEP and free TRAM flaps have identical blood supplies and similar harvesting techniques (8). The defining feature of these two flaps includes the presence or absence of the rectus abdominis muscle and the number of perforating vessels perfusing the flap. The amount of rectus abdominis muscle incorporated into a free TRAM flap is significantly variable and can range from an entire width of the muscle to a small 2 cm × 2 cm segment of muscle (Fig. 65.6). The latter type of free TRAM flap incorporates a small segment of anterior rectus sheath and is known as a muscle-sparing free TRAM flap. The rectus muscle incorporated into the free TRAM may be full width (MS-0) or partial length. Partial width flaps will preserve the lateral segment (MS-1) or the lateral and medial segments (MS-2) (9). The free TRAM flap is usually designed to include a variable number of perforators (generally three to six). In contrast, the DIEP flap (MS-3) incorporates no muscle or anterior rectus sheath, and the number of perforators with a caliber greater than 1.5 mm generally ranges from one to three. One review of 88 DIEP flaps that examined the number of perforators included with the flaps demonstrated that one perforator was included in 76%, two perforators were included in 22%, and three perforators were included in 2% (10). The DIEA may have a dominant medial (18%), central (28%), or lateral (54%) branch pattern. Lateral perforators tend to course more perpendicularly, which may ease dissection. The majority of perforators are located within 8 cm of the umbilicus, 2 cm above and 6 cm below the umbilicus. Doppler imaging has determined the average mean diameter of the deep inferior epigastric artery to be 3.6 mm (range, 2.8 to 5 mm) (11,12). Average pedicle length is 10.3 cm but may be quite variable. Several segmental nerves enter the rectus abdominis at the junction of the lateral and central segments. Small, type 1 nerves demonstrate overlapping innervation from adjacent nerves and may be sacrificed without functional detriment. Single large, type 2 nerves at the level of the arcuate line innervate the entire width of rectus muscle and may contribute to donor-site morbidity and abdominal bulge if sacrificed (13).
Indications
The use of the DIEP flap in breast reconstruction for breast cancer defects after mastectomy allows for excellent shape and
contour of the breast mound while minimizing donor-site morbidities related to abdominal strength and contour.
contour of the breast mound while minimizing donor-site morbidities related to abdominal strength and contour.
For patients who present with excess skin and fat overlying the abdomen, an abdominal perforator flap is an ideal tissue source for breast reconstruction (Fig. 65.7). Morbidly obese women with a large abdominal pannus are discouraged from perforator flap reconstruction (Fig. 65.8). There are a number of preoperative and intraoperative factors used to decide between performing a TRAM flap versus a DIEP flap (14,15,16). Important preoperative factors include breast size, breast volume, body habitus, quantity and quality of abdominal skin and fat, and tobacco use.
Size and volume of the natural breast are major determinants that influence flap choice. This is usually achieved by visual assessment; however, a more accurate assessment can be calculated using three-dimensional imaging techniques (17). In our practice, women with a breast volume less than 1,000 cc are potential candidates for DIEP or free TRAM flap reconstruction, whereas women with a breast volume greater than 1,000 cc are better candidates for the free TRAM flap (9) Large-volume (>1,000 cc) breast reconstruction may be at an increased risk for complications related to inadequate vascular perfusion. Preoperative assessment of abdominal perforators has been demonstrated to be useful in predicting the presence
and course of these abdominal wall perforators. This can be achieved using duplex ultrasound or computed tomography angiography (18). Preoperative imaging may aid in preoperative determination of perforator location and the possibility of performing a superficial inferior epigastric artery flap.
and course of these abdominal wall perforators. This can be achieved using duplex ultrasound or computed tomography angiography (18). Preoperative imaging may aid in preoperative determination of perforator location and the possibility of performing a superficial inferior epigastric artery flap.
Contraindications
Contraindication to DIEP flap reconstruction can include previous abdominal incisions when they are located such that they would compromise the amount of available tissue (Fig. 65.9). Previous Pfannenstiel incisions usually do not compromise the integrity of the deep inferior epigastric artery or vein, although this has been observed on occasion. Although previous abdominal incisions, such as a subcostal incision, are not absolute deterrents, care must be exercised to minimize the degree of undermining and maintain adequate blood supply to the anterior abdominal tissues.
 Figure 65.7. An ideal candidate for a deep interior epigastric perforator flap in which there is an adequate volume of lower abdominal tissue to reconstruct a breast. |
The clinical status of the patient depends on a variety of factors that also may affect the free flap. These include advanced age, nutritional status, tobacco use, and presence of underlying
comorbidities (e.g., diabetes mellitus, cardiopulmonary disease, peripheral vascular disease). Although advanced age and tobacco use are not contraindications to free-flap operations, poor nutritional status can impede wound healing and recovery. Morbidly obese women with a large abdominal pannus are discouraged from proceeding with abdominal flap reconstruction (15). Women with a history of tobacco use may be better candidates for free TRAM reconstruction to include more perforators and minimize the morbidity related to tobacco use (14). Patients with poorly controlled diabetes mellitus and peripheral vascular disease require adequate glucose control and may require revascularization procedures prior to free tissue transfer. Surgical clearance by a medical physician is recommended for patients with multiple medical problems.
comorbidities (e.g., diabetes mellitus, cardiopulmonary disease, peripheral vascular disease). Although advanced age and tobacco use are not contraindications to free-flap operations, poor nutritional status can impede wound healing and recovery. Morbidly obese women with a large abdominal pannus are discouraged from proceeding with abdominal flap reconstruction (15). Women with a history of tobacco use may be better candidates for free TRAM reconstruction to include more perforators and minimize the morbidity related to tobacco use (14). Patients with poorly controlled diabetes mellitus and peripheral vascular disease require adequate glucose control and may require revascularization procedures prior to free tissue transfer. Surgical clearance by a medical physician is recommended for patients with multiple medical problems.
 Figure 65.8. A less-than-ideal candidate for a deep interior epigastric perforator (DIEP) flap based on increased body weight, body mass index, and body habitus. There is excessive lower abdominal lipodystrophy that might preclude one from safely and effectively performing a DIEP flap.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|