Debridement of Soft Tissue Infections of the Foot and Ankle
Hunter S. Oliver-Allen
Michael C. Holland
Scott L. Hansen
DEFINITION
Soft tissue infections of the lower leg and foot include a spectrum of severity from superficial cellulitis to rapidly progressive necrotizing fasciitis.
Soft tissue infections of the foot and ankle can involve skin, subcutaneous tissue, fascia, muscle, ligaments, tendons, joints, and around the nails.
Secondary infections can be due to peripheral vascular disease (PVD), diabetes, metabolic conditions, and immunocompromised patients.
Infections of the foot and ankle are often categorized into three groups: soft tissue infections, bone infections, and diabetic infections.
Infections can be further characterized into nonpurulent (cellulitis and erysipelas), purulent (abscess), necrotizing soft tissue infections (NSTI) (including necrotizing cellulitis, myositis, and fasciitis) as well as tendonitis and septic arthritis.
Immediate goal is to treat and control the infection.
Long-term goal is for limb salvage, preserve limb function, and decrease risk for amputation.
Infections are most commonly caused by bacteria, however can also be due to viral, fungal, or mycobacteria.
Some may respond to treatment with topical, oral, or intravenous antibiotics alone, while others will require surgical debridement of devitalized tissue.
Typically present as painful lesions with skin changes invariably present, with or without involvement of deeper tissues.
ANATOMY
The lower leg, ankle, and foot comprise 28 bones.
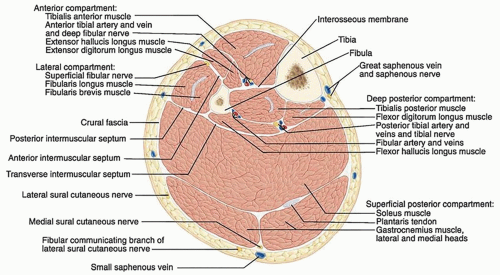
Soft tissues include muscles that are divided into anatomically distinct compartments in both the lower leg and the foot (FIG 1).
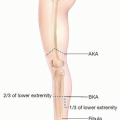
The four compartments of the lower leg include the anterior, lateral, superficial posterior, and deep posterior divided by fascia.
The nine compartments of the foot include the calcaneal —communicating with the deep posterior compartment of the leg, superficial, medial, lateral, adductor, and four interosseous.
The primary neurovascular structures include the anterior tibial, peroneal, and posterior tibial arteries and paired veins; superficial peroneal, deep peroneal, tibial, saphenous, and sural nerves; and greater and lesser saphenous veins in the superficial tissues.
Plantar surface is composed of thick glabrous epidermis and dermis, and a subcutaneous layer with vertical fibrous septae, densely adhering it to the plantar fascia and periosteum.
PATHOGENESIS
Infections result from breakdown of natural defenses in skin such as with trauma or open wound and invasion of resident skin flora or environmental pathogens.1
Patients with neuropathy and vascular disease and are immunocompromised have increased risk of infection.1
Group A beta-hemolytic streptococcus is the most common and second most common is Staphylococcus aureus.
Infections are also commonly polymicrobial, especially in diabetic patients.
NSTI result from bacterial invasion and subsequent angiothrombosis decreasing blood supply causing tissue necrosis They are classified into two groups:2
Type I is a polymicrobial infection consisting of anaerobic bacteria and aerobic bacteria.
Type II is monomicrobial infections typically of group A streptococcus or other beta-hemolytic streptococcus alone or with other pathogens.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree