Cytotoxic and Antimetabolic Agents: Introduction
|
Cytotoxic and antimetabolic agents may be used to treat severe or refractory skin disease. The toxicities of such agents are significant and must be balanced against therapeutic advantage. In treating skin disease, most of these agents are utilized at immunomodulatory rather than cytotoxic dosages.
Cytotoxic and antimetabolic drugs modulate the behavior of inflammatory and other cells through inhibition of cell growth and development. The cell cycle represents a conceptual schema for the sequence of growth experienced by essentially all cells (see Chapter 46). The cycle begins with the G1 phase, which is directed toward preparing the cellular apparatus for DNA synthesis. The S phase follows G1 and is devoted to DNA synthesis. At the end of DNA synthesis, the G2 phase occurs. The G2 phase is followed by the M phase, or actual cell division. Some cells may also enter a resting state of indeterminate length, termed G0. Specific cytotoxic drugs may be effective at different stages of the cell cycle.
The cytotoxic drugs commonly used in dermatology fall into two classes: (1) antimetabolites and (2) alkylating agents. Antimetabolites mimic natural molecules and are most active while DNA is being synthesized (S phase). Alkylating agents exert effect through physicochemical interactions with DNA, such as alkylation, cross-linking, and carbamylation. The effects of alkylating agents are generally independent of the cell cycle.
The immunosuppressive properties of cytotoxic agents (see also Chapter 233) provide benefit in immunologically mediated disease, yet these agents may predispose to infection as well. Potentially lethal infections may arise quickly in an immunosuppressed patient. Those placed on cytotoxic agents should be queried at each visit for symptoms of infection, such as fever, chills, sweating, shortness of breath, cough, headache, dysuria, and arthritis. Prompt reporting of symptoms should be encouraged.
Antimetabolic Agents
Methotrexate remains one of the most frequently employed antimetabolic agents in dermatology. With appropriate monitoring, an impressive record of safety with methotrexate has accumulated. Concerns regarding use of methotrexate are best addressed through increased drug awareness, rational patient selection, appropriate laboratory monitoring, and, most recently, folate supplementation.
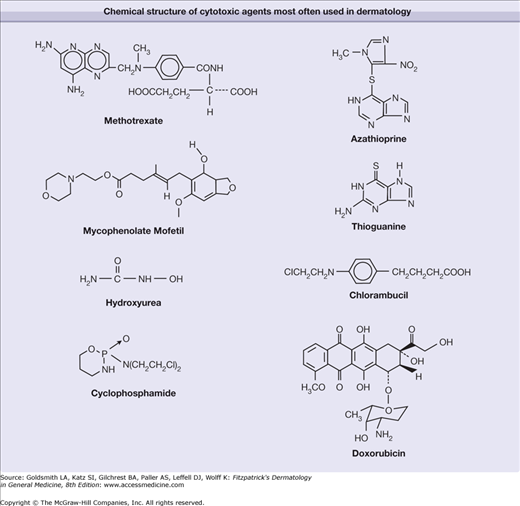
Methotrexate (Fig. 227-1) is an analog of folate that competitively and irreversibly inhibits dihydrofolate reductase (Fig. 227-1). Methotrexate also partially inhibits thymidylate synthetase. Through inhibition of these enzymes, methotrexate decreases the availability of reduced folate and thymidylate necessary for RNA and DNA synthesis. Other inhibitors of folate metabolism, such as trimethoprim-sulfamethoxazole, may potentiate the toxicity of methotrexate (see Section “Drug Interactions”).
Like folate itself, the activity of methotrexate is enhanced by glutamylation. Glutamylation also yields additional anti-inflammatory properties.1 First, by inhibiting aminoimidazole carboxamide ribonucleoside transformylase, methotrexate-polyglutamate increases the local tissue concentration of adenosine, which has potent anti-inflammatory action. Second, by decreasing available tetrahydrofolate, methotrexate decreases the production of S-adenyl methionine, which also results in decreased inflammation.
Oral methotrexate is absorbed rapidly through the gastrointestinal tract. In children, absorption is decreased by concurrent ingestion of food and milk, but this has not been observed in adults. In adults, the mean bioavailability is 67% of the administered dose. Peak plasma levels occur 1–3 hours after administration. The half-life of the drug is 4–5 hours. For doses higher than 25 mg/week, gastrointestinal absorption is more erratic, and some experts recommend intramuscular dosing above this level.2
Methotrexate is eliminated chiefly by the kidneys, with 60%–95% excreted unchanged. Decreases in glomerular filtration or tubular secretion may lead to methotrexate toxicity. Approximately 50% of methotrexate within the blood is protein bound. Weak organic acids, such as aspirin or many other nonsteroidal anti-inflammatory agents, may displace methotrexate, altering blood levels and renal excretion (see Section “Drug Interactions”).
Methotrexate is used for many purposes in dermatology, but its chief indication is for treatment of severe psoriasis. The effects of methotrexate in psoriasis were first recognized in the late 1950s and 1960s,3 and by the late 1980s, more than one-half of dermatologists reported using methotrexate to treat severe psoriasis.4 The impact of an increasing number of systemic treatments for psoriasis (the “biologics”; see Chapter 234) on the use of methotrexate has not been fully studied, but recent analysis has confirmed that methotrexate represents the most affordable and a very effective systemic treatment for psoriasis.5 Methotrexate has also been used in a variety of other autoimmune and connective tissue diseases, vasculitides, inflammatory dermatoses, and papulosquamous conditions (Box 227-1).
|
Typical oncologic doses of methotrexate (100–250 mg/m2/week) are cytotoxic; however, lower doses (7.5–25.0 mg/week) are immunomodulatory. In dermatology, methotrexate doses are typically less than 30 mg/week, and are often less than 17.5 mg/week. Cumulative dose should be tracked and recorded, as this may impact monitoring with continued use (see Section “Monitoring Therapy”).
Methotrexate is available in 2.5-mg tablets. For those with economic limitations, methotrexate liquid (25 mg/mL) may be more affordable for peroral use.6 Either a single weekly dose or a weekly dose divided into three portions separated by 12 hours is used. These dosing regimens are equally efficacious, but split dosing may lessen gastrointestinal upset.
Evaluation before methotrexate use includes a careful history and physical examination, and assessment of concomitant conditions or medications that may limit methotrexate use. Exclusion of patients inappropriate for methotrexate therapy is an important first step in management. Relative contraindications to methotrexate use include abnormalities in renal or liver function (including viral hepatitis), cirrhosis, excessive alcohol consumption, concomitant use of hepatotoxic drugs, active infection, immunosuppression, recent vaccination (particularly live vaccines), obesity (body mass index >30), diabetes mellitus, poor reliability, and an active desire to conceive (men and women).7 In general, the elderly are often less amenable to methotrexate therapy due to declining renal function. Administration of methotrexate to pregnant women or nursing mothers is strictly contraindicated. While use of methotrexate is often avoided in the setting of HIV, it may be appropriate in select circumstances; caution is advised.8
Baseline laboratory studies (Table 227-1) include a complete blood cell count (CBC); platelet count; liver function testing; serologic assessment for hepatitis A, B, and C antibodies (if indicated or preferred by the clinician); renal function assessment; and pregnancy and HIV screening (where indicated).7 While a baseline screen for tuberculosis using purified protein derivative (PPD) is not expressly mandated, the Centers of Disease Control and Prevention recommends consideration of such testing for any patient placed on immunosuppressive medication.9 Similarly, screening for strongyloides infection may be appropriate in some populations.10
Initial Evaluation | Ongoing Laboratory Monitoring |
|---|---|
|
|
|
|
|
|
|
|
|
|
Initiation of methotrexate therapy typically involves use of a single 5- to 10-mg test dose. Repeat laboratory studies, a skin examination, and a review of systems are conducted 1 week later. Performance of repeat laboratory studies sooner than 5–6 days after dosing yields only expected elevated liver transaminases and may confound interpretation.
If the test dose is tolerated and laboratory studies are satisfactory, weekly therapy may commence using a typical starting dose of 7.5–10 mg/week, depending on the severity of disease, overall health, and ideal body weight of the patient. Some authorities may begin with a dose as high as 15 mg/week in certain settings. The dose may be increased by 2.5–5.0 mg every 4–8 weeks until adequate control is achieved or toxicity ensues.7 When improvement has stabilized, the dose may be tapered in 2.5-mg decrements to a point at which disease activity increases slightly. The goal is to allow for mild- or low-grade psoriasis to avoid an unacceptably high dose. It is important to discuss this expectation with the patient to prevent confusion regarding the endpoint. Concomitant topical therapy may also lower the methotrexate dose needed for satisfactory control.
If a patient does not demonstrate satisfactory improvement on a dose of 20–25 mg/week, consideration of alternative agents is indicated. Occasional patients with refractory disease may respond better to parenteral methotrexate, typically intramuscular dosing. In refractory cases, methotrexate may be combined with ultraviolet B (UVB) phototherapy, psoralen and UVA light (PUVA), cyclosporine, oral retinoids, or biologics to enhance efficacy.7
Ongoing laboratory evaluation during methotrexate therapy (Table 227-1) should include a CBC with manual differential and platelet count and liver function tests weekly for 2–4 weeks for the first few months, then every 1–3 months.7 Repeat testing with any dose escalation or intercurrent illness. Liver function testing should not be performed earlier than 5 days after dosing to avoid confounded results. Renal function tests should be performed every 2 to 3 months,7 or with any suspicion of altered renal function.
Recent developments have altered recommendations regarding liver biopsy in the setting of methotrexate use for psoriasis. For patients without risk factors for liver injury (Table 227-2), current recommendations for liver biopsy are similar to those issued by the American College of Rheumatology with regard to use of methotrexate in rheumatoid arthritis. However, for patients with risk factors for methotrexate-induced liver injury, a delayed baseline liver biopsy should be considered (usually after 2–6 months of use, when it is apparent the medication is efficacious, well tolerated, and likely to be continued), and again at a cumulative dose of 1.0–1.5 g. Monitoring via measurement of the aminoterminal peptide of procollagen III (PIIINP) is popular in some European countries, but the test is not approved for use in the United States.7
Risk Factors for Hepatic Toxicity | Recommendations for Low-Risk Patients |
|---|---|
|
Recommendations for High-Risk Patients
|
Absolute and relative contraindications and common adverse effects of methotrexate are summarized in Box 227-2.
|
Adverse reactions to methotrexate range from the trivial to life threatening.
Nausea and vomiting with oral administration is common and dose related. Such effects may be seen with parenteral dosing as well. Indeed, 10%–30% of all patients placed on methotrexate may experience some gastrointestinal upset. Symptoms may even occur before dosing or 24–36 hours afterward, suggesting a psychosomatic or anticipatory basis in select cases. Supplementation with folate (1–5 mg/day) reduces gastrointestinal symptoms without compromising efficacy.11–14 A recent study on folate supplementation (5 mg daily) suggested a slight decrease in methotrexate efficacy,15 but others questioned the methodology,16 and most authorities continue to advocate strongly for supplementation.7
Induction of liver fibrosis is a major concern with methotrexate use. Methotrexate is hepatotoxic, and some elevation in liver transaminases is expected with use. These elevations occur near to administration and are not strictly predictive of those predisposed to fibrosis. Dose reduction or discontinuance is indicated if transaminases exceed two- to threefold normal values when measured at least 5–6 days after the last dose.
The gold standard for assessing methotrexate-induced liver fibrosis is percutaneous needle biopsy. The procedure is not without risk; minor bleeding occurs in 1 in 1,000 patients, and the risk of death is estimated at 1 in 10,000.17 Liver specimens are assessed for lobular architecture, inflammation and fibrosis, and fat infiltration. A grading scheme using a scale of I to IV is widely employed (Table 227-3). Patients with grades I and II histology may continue methotrexate, those with grade IIIA histology may continue with a repeat liver biopsy in 6 months, and those with grades IIIB and IV histology should discontinue methotrexate.7
Biopsy Grade | Histopathologic Findings | Recommended Action |
|---|---|---|
I | Normal; fatty infiltration (mild), portal inflammation (mild) | Continue methotrexate |
II | Fatty infiltration (moderate to severe), portal inflammation (moderate/severe) | Continue methotrexate |
IIIA | Fibrosis (mild) | Continue methotrexate; repeat biopsy in 6 mon |
IIIB | Fibrosis (moderate to severe) | Discontinue methotrexate |
IV | Frank cirrhosis | Discontinue methotrexate |
A noninvasive test for liver fibrosis would be ideal. Ultrasound alone has demonstrated conflicting results.18,19 Radionuclide scans and the aminopyrine breath test have proven inadequate for independent detection of methotrexate-induced fibrosis.20,21 Serum assay of the PIIINP may suggest fibrosis; however, specificity is limited. PIIINP is simply a marker of fibrogenesis, and it may be elevated during fibrosis of any organ system.22 It is unreliable in patients with psoriatic arthritis. A compelling argument has been made to use an amalgam of tests, such as ultrasound, dynamic radionuclide scanning, and PIIINP assay, to reduce the number of required liver biopsies. Nevertheless, at present, percutaneous liver biopsy remains the gold standard for evaluation when methotrexate-induced liver disease is suspected.23
The most important acute adverse effect of methotrexate is myelosuppression. Anemia, neutropenia, and thrombocytopenia may result from methotrexate use. Risk factors for bone marrow toxicity include advanced age, poor renal function, and concurrent administration of conflicting medications (see Section “Drug Interactions”).
Oral ulcerations or stomatitis may be noted with methotrexate use. Skin ulceration, particularly of the lower legs, may herald bone marrow suppression. In patients treated with methotrexate for psoriasis, rapid ulceration of psoriatic plaques may also suggest toxicity.24 Laboratory studies and dose reduction or complete discontinuance is indicated when mucocutaneous ulcerations or skin ulcerations develop, respectively. Methotrexate may also engender a cutaneous “recall reaction” in areas of prior irradiation or recent sunburn.25 Mild alopecia has been described with methotrexate use. Other cutaneous manifestations include acral erythema, epidermal necrosis, and vasculitis.
Low-dose methotrexate use has not been definitively associated with carcinogenesis, but a recent study examining patients using methotrexate for rheumatoid arthritis demonstrated a 50% increased risk of malignancy relative to the general population, with a threefold increased risk in melanoma, a fivefold increased risk in non-Hodgkin lymphoma, and a nearly threefold increase in lung cancer.26 Conversely, in a cohort study from the United Kingdom, a slight increase in lymphoma was observed among psoriatic patients, but use of methotrexate was not discriminatory.27
Methotrexate is a Category X agent during pregnancy, and administration is absolutely contraindicated (see Box 227-2). Pregnancies that occur after the discontinuation of methotrexate appear unaffected, but it is generally advocated that men wait 3 months after discontinuance before attempting conception; women should wait one complete menstrual cycle. Reliable contraception is requisite while taking methotrexate.7
Acute pneumonitis and pulmonary fibrosis have been reported with methotrexate use in psoriasis, although such reactions are more common in rheumatoid arthritis patients.28 Pulmonary toxicity likely represents an idiosyncratic reaction. Chest radiographs and pulmonary function testing are not useful in the detection or prevention of pulmonary fibrosis.29 A chest X-ray should be performed in those with symptoms of pneumonitis. Discontinuance is recommended if examination findings are concerning.
Opportunistic infections (e.g., Pneumocystis pneumonia, cryptococcosis, and histoplasmosis) have been reported in otherwise healthy individuals receiving low-dose methotrexate.10,30–33 Admittedly, such patients were often using other immunosuppressive medications as well; often prednisone.
Systemic anaphylaxis with low-dose methotrexate has been reported.34 Many patients suffering from anaphylaxis had received methotrexate before, at comparable doses, without untoward effects.
Daily supplementation with 1–5 mg of folate has reduced nausea, vomiting, stomatitis and oral ulceration, elevated transaminases, and mild myelosuppression without compromising the efficacy of methotrexate.11–14 Pneumonitis, and moderate-to-severe myelosuppression are not mitigated by folate supplementation. Elevated homocysteine levels, common with methotrexate use and an independent risk factor for coronary artery disease, are decreased with folate supplementation.35
Folinic acid may also be used as supplementation, but it should not be given concurrently with methotrexate dosing. Instead, it is dosed at 5 mg by mouth every 12 hours for 3 doses, beginning 12 hours after the last weekly methotrexate dose. Unlike folinic acid, folate does not compete with methotrexate for cellular uptake, and it can be taken daily. Both are available as generic medications. One drawback to folate supplementation is the potential masking of vitamin B12 deficiency. Use of folate supplementation with methotrexate therapy is well established.7
Methotrexate overdose is more likely in patients with declining renal function, in those who misunderstand dosing directions, or in those concomitantly exposed to a second folate antagonist, such as trimethoprim-sulfamethoxazole. Overdose should be treated promptly with folinic acid (leucovorin). Folinic acid is metabolized in vivo to tetrahydrofolate in the absence of dihydrofolate reductase, providing an alternative supply of DNA and RNA precursors.
Folinic acid should be given early, preferably within the first 24–36 hours after overdose. Folinic acid itself has very little toxicity. Therefore, an oral dose of 10 mg/m2 should be given on first suspicion of methotrexate overdose without delay for a serum assay.7 Peroral or parenteral doses may be continued every 6 hours until the serum concentration of methotrexate falls to less than 10−8 M. Practically speaking, or when a serum assay is unavailable, this recommendation is often equivalent to 15–25 mg of folinic acid by mouth every 6 hours for six to ten doses.
Although any drug that may enhance methotrexate toxicity should be avoided during therapy, there are several near-absolute contraindications (Box 227-3), including aspirin, many nonsteroidal anti-inflammatory agents, probenecid, and trimethoprim-sulfamethoxazole.36 Conversely, many cyclooxygenase-2 selective inhibitors, like celecoxib, do not impact the pharmacokinetics of methotrexate.7
Azathioprine is a synthetic analog of natural purine bases used in RNA and DNA synthesis (see Fig. 227-1). Although many thiopurine derivatives exist, azathioprine is the agent most often used in dermatology.
Azathioprine is a prodrug that is metabolized in the body to 6-mercaptopurine (6-MP). 6-MP is further anabolized via hypoxanthine-guanine phosphoribosyl transferase (HGPRT), ultimately to a purine analog, 6-thioguanine (6-TG), that inhibits RNA and DNA synthesis and repair, yielding immunosuppression. HGPRT activation is critical. Yet patients with Lesch-Nyhan syndrome (HGPRT deficiency) experience no immunosuppression or untoward effects while taking azathioprine.37
Azathioprine and its metabolite, 6-MP, are equally potent when administered parenterally, but azathioprine enjoys improved bioavailability, with 88% of the oral dose being absorbed through the gastrointestinal tract. After absorption, azathioprine is converted to 6-MP, mostly within erythrocytes. The fate of 6-MP is determined by one of three competing metabolic pathways: (1) it may be anabolized to an ultimate active form (6-TG) via HGPRT, (2) it may be catabolized to an inactive form via xanthine oxidase (XO), or (3) it may be catabolized to an inactive form by thiopurine methyltransferase (TPMT).38
Elucidation of the TPMT-dependent catabolic pathway has revolutionized the clinical use of azathioprine. In humans, expression of TPMT is variable due to genetic polymorphisms. Patients may be categorized into three subgroups: (1) a large majority possesses high levels of TPMT expression (∼90%), (2) intermediate expression is demonstrated in ∼10%, and (3) less than 1% demonstrate very low TPMT activity (about 1 in 300 persons).39 Commercial assays for TPMT activity allow for graduated azathioprine dosing, with improved efficacy and a lesser incidence of unforeseen side effects (see Section “Dosing Regimen”).40,41
XO is another enzyme involved in the catabolism of 6-MP. Allopurinol, used in the treatment of gout, is a potent inhibitor of XO; toxicity may result in those taking both medications.42 Unlike TPMT, there is very little genetic variation in XO expression, and it is unnecessary to assess innate XO expression before azathioprine dosing. A careful medication history, however, is critical (see Section “Drug Interactions”).
In dermatology, azathioprine is used “off-label” chiefly as a steroid-sparing agent for immunobullous disorders, including pemphigus, cicatricial pemphigoid, and severe or recalcitrant bullous pemphigoid (Box 227-4).43 In a prospective, long-term study of pemphigus vulgaris patients treated with glucocorticoids and azathioprine, 45% achieved remission.44 The steroid-sparing effect of azathioprine in pemphigus has been challenged in literary review, but not in a clinical trial; it remains a common regimen among practicing dermatologists.45
|
Azathioprine is supplied as 50-mg tablets and also as an injectable. Traditionally, a dose of 1–2 mg/kg/day of azathioprine was used, often concurrent with high-dose prednisone. Increasingly, the appropriate dosage is now based on a patient’s own TPMT expression (Table 227-4).40 Impaired renal function may be associated with greater toxicity, and the dosage may still be adjusted for this reason.
TPMT Erythrocyte Assay | Maximum Azathioprine Dose |
|---|---|
>19.0 U (high expression) | 2.5 mg/kg/day |
13.7–19.0 U (intermediate expression) | 1.5 mg/kg/day |
5.0–13.7 U (low expression) | 0.5 mg/kg/day |
<5.0 U (very low expression) | Do not use |
Before therapy, the patient should receive a complete history and physical examination. Exclusion of patients with severe comorbidities, active infections, or the possibility of reactivation of an infection (tuberculosis) is recommended. All women of childbearing age should receive a pregnancy test. Patients with a history of exposure to alkylating agents should likely not receive azathioprine unless unavoidable, as an increased risk of lymphoproliferative disease exists when used in succession.
Baseline laboratory tests include a CBC with manual differential and platelet count, renal and liver function testing, and an erythrocyte TPMT activity assay should be performed. There are reports of mycobacterial infection in those taking azathioprine, and tuberculin screening should be considered. In steroid-responsive bullous disorders and in connective tissue disease, experienced practitioners often initiate azathioprine concurrently with high-dose steroids.
During therapy, a CBC with manual differentiation and platelet count should be obtained biweekly for the first 2 months, monthly for the next 2 months, and every 2 months thereafter; liver function testing should occur every month for 3 months and then bimonthly thereafter.46 Additional laboratory testing is necessary with dosage increases or if an initial TPMT level cannot be determined. Biannual physical examinations should pay particular attention to evidence of possible lymphoreticular disease and skin cancer, particularly squamous cell carcinoma (SCC). Safety guidelines used during azathioprine therapy are summarized in Box 227-5.
|
Recently, optimal erythrocyte levels of 6-TG necessary for disease remission in patients with immunobullous disease treated with azathioprine were determined.47 Optimal levels of 6-TG in erythrocytes for disease remission were 150–300 pmol/8 × 108 erythrocytes. Lower levels were observed in lesser disease states. High levels of the inactive metabolite 6-methylmercaptopurine and induction of TPMT were associated with recalcitrant disease.
In fact, TPMT induction (>10 U from baseline) explains why some patients fail to respond to high azathioprine doses (at least 2.5 mg/kg/d), even when baseline measurement suggested an intermediate level of enzyme activity within erythrocytes. Experts were quick to recognize the clinical value of this observation; this type of nonresponder should be switched to an alternative agent.48 Similarly, measurement of TPMT activity (at baseline and during use) and 6-TG levels within erythrocytes allows for an algorithmic approach to discriminate among the underdosed, noncompliant, and those experiencing TPMT-induction (Table 227-5).47,48 Furthermore, TPMT genotype determination may be used when RBC enzyme activity is near the cutoff between high activity and intermediate activity, to allow for more aggressive azathioprine dosing.47
Test/Value | Optimal Responder | Underdosed | Noncompliant | TPMT Induction |
|---|---|---|---|---|
TPMT (erythrocyte) | Near baseline | Near baseline | Near baseline | Elevated above baseline (>10 U) |
6-Thioguanine (active metabolite) | Optimal | Low | Low | Low |
6-Methylmercaptopurine (inactive metabolite) | Elevated | Low | Low | Elevated significantly |
Azathioprine dose | Adequate | Inadequate, potentially will respond to increasea | Presumed adequatea | May respond to increaseb |
Absolute and relative contraindications and common adverse effects of azathioprine are summarized in Box 227-6.
|
With careful monitoring, azathioprine is generally safe. Adverse effects tend to occur in those patients with lower TPMT activity levels, higher doses of azathioprine, or concomitant use of allopurinol.
Myelosuppression is a major side effect of azathioprine use. Generalized depression of all blood cell lines is most common,49 but depression of any single lineage may be observed. Thrombocytopenia is a common initial presentation of bone marrow toxicity. Bone marrow suppression tends to occur at higher doses,50 and in those with lower TPMT expression. Discontinuance usually results in complete marrow recovery.
Most patients treated with azathioprine also receive large doses of glucocorticoids. Therefore, it is often difficult to quantify the independent role of azathioprine in any predisposition toward infection. Herpes virus infections, human papilloma infection, and scabies infestation have been reported in those taking azathioprine.50
Patients receiving high doses of azathioprine may experience nausea, vomiting, and diarrhea. Such symptoms are not usually treatment limiting and may be reduced by administration with food.
Toxic hepatitis has developed in approximately 1% of patients treated with azathioprine for rheumatoid arthritis, and it is usually reversible.51 Other adverse effects include hepatic veno-occlusive disease and associated pancreatitis. Discontinuance is warranted with evidence of liver toxicity.
Azathioprine-induced shock and hypersensitivity reactions have been reported in patients with cutaneous disease. In most cases, hypotensive collapse occurred within hours of the initial dose. Drug fever has also been reported with azathioprine (see Chapter 41).
An increased risk of lymphoproliferative disease has been documented in renal transplant recipients, rheumatoid arthritis patients, and, most recently, inflammatory bowel disease patients treated with chronic azathioprine.52–54 In one study, the relative risk was increased roughly 10- to 13-fold, or one lymphoma per 1,000 patient-years of azathioprine treatment. Dermatologic doses of azathioprine are often lower and the duration of treatment shorter, leading to speculation that the risk of lymphoma is probably lower in those treated for cutaneous disease. However, the most recent meta-analysis of patients treated with azathioprine for inflammatory bowel disease who developed lymphoma included those on “low-dose” regimens.54 In light of this information, it seems prudent to inform patients that the exact magnitude of any increased risk for lymphoma with “low-dose” azathioprine is largely unknown. Patients with a prior exposure to alkylating agents may have a prohibitive risk of lymphoma if treated subsequently with azathioprine; great caution is suggested in this population.
Aggressive behavior of SCC has been described in patients taking azathioprine for eczema, atopic dermatitis, and chronic actinic dermatitis.55 It was recently suggested that azathioprine used in solid organ transplant recipients may sensitize DNA to UVA radiation, leading to the increased incidence of SCC in this population.56 Admittedly, confounding risk factors exist, but a later small series confirmed a reduced minimal erythema dose to UVA irradiation with coadministration of azathioprine.57 Dermatologists should be aware of this emerging research, as only broad spectrum sun-screens mitigate UVA exposure, and such rays are not blocked by glass.
Azathioprine is a Category D agent during pregnancy. The prodrug and the active metabolites readily cross the placenta. The rate of congenital malformation appears to be low (4.3%), but myelosuppression and immunosuppression are significant occurrences in neonates and breastfed infants. Fertility of men or women appears unaffected by azathioprine.58
A major drug interaction occurs between azathioprine and allopurinol. When allopurinol must be used concurrently, the azathioprine dose must be decreased by 75%. There is evidence that aminosalicylates may inhibit TPMT activity, and it may be prudent to minimize or avoid such medications in patients using azathioprine.
Thioguanine (see Fig. 227-1) is a less utilized member of the thiopurine family of drugs. It has a metabolism and mechanism of action similar to that of azathioprine.
Thioguanine is a prodrug that produces nucleoside analogues through the action of purine nucleoside phosphorylases present in tissues. These guanine analogues undergo enzymatic conversion to nucleotides and ultimately yield cytotoxic activity via incorporation into cellular DNA. Apoptosis is induced preferentially against activated T lymphocytes. The clinical response to thioguanine has been correlated to decreased T lymphocyte counts in psoriatic skin lesions, irrespective of systemic lymphocyte counts.59
Thioguanine is administered orally, but it has incomplete and unpredictable absorption. Peak plasma concentrations may vary tenfold and occur 2–4 hours after ingestion.60
In dermatology, thioguanine is used chiefly for the treatment of psoriasis, particularly in those with recalcitrant disease or with contraindications to other systemic therapies (Box 227-7). In a recent retrospective study of patients with recalcitrant psoriasis, 14 of 18 patients experienced greater than 90% improvement with thioguanine, including patients with psoriatic arthritis, palmoplantar disease, or scalp involvement.61 Thioguanine has been used effectively, although infrequently, to treat lupus and atopic dermatitis.
Thioguanine is supplied as 40-mg tablets. Classically, treatment was initiated with a 40 mg/day dose, with close monitoring for myelosuppression. After 1 month, if the clinical response was inadequate, the dose was increased to 80–120 mg/day. A pulsed regimen of 100 mg to 120 mg twice weekly, increasing up to 160 mg three times per week, has been reported effective.62 The most recent guidelines suggest an amalgam of these strategies, beginning with a dose of 80 mg twice weekly with possible advancement by 20 mg every 2 to 4 weeks, to a maximum dose of 160 mg three times weekly.46
Similar to azathioprine, use of commercial assays for TPMT activity improve thioguanine dosing. The latest review of thioguanine use in severe psoriasis recommends an assessment of TPMT levels before treatment so as to guide the selection of an adequate starting dose.61 Patients with high levels of TPMT expression can likely tolerate higher initial doses.
All patients should undergo a thorough history and physical examination before initiation of treatment. Patients with severe comorbidities, particularly hematologic disturbances, or active infection should be excluded. Women of childbearing age should receive a pregnancy test. Recommended baseline laboratory studies include a CBC with manual differential and platelet count, liver function studies, and a TPMT activity assay.
Repeat blood counts and liver function tests should be followed weekly at first, transitioning to biweekly as the dose stabilizes, then monthly for 3 months, and quarterly thereafter. Always perform complete and broad laboratory testing when a dose is escalated or there is a change in the patient’s health status. Safety guidelines used during thioguanine therapy are summarized in Box 227-8.
|
Absolute and relative contraindications and common adverse effects of thioguanine are summarized in Box 227-9.
|
Common adverse effects of thioguanine include myelosuppression and gastrointestinal disturbances. In the largest series of patients using thioguanine for psoriasis, just less than one-half experienced myelosuppression, yet only 20% required complete discontinuance.63 In one series, thrombocytopenia was the earliest indicator of myelosuppression.61 Pulsed dosing of thioguanine has been associated with a lower rate of myelosuppression, but, admittedly, TPMT testing was not performed in this study.62
Gastrointestinal disturbances include nausea, excessive flatulence, taste changes, esophageal reflux, and diarrhea, symptoms that are often tolerated without discontinuance. In a single study, elevated liver transaminases occurred in 25% of patients, yet many had been taking methotrexate before the study.63 Generally, thioguanine is not considered particularly hepatotoxic; liver biopsy is not indicated during treatment. Rare cases of toxic hepatic veno-occlusive disease have been described in patients using thioguanine for psoriasis.64 Low-dose thioguanine use in pregnant women has been reported with inflammatory bowel disease; however, use during pregnancy is generally avoided.65
Thioguanine metabolism is not dependent on XO; it may be administered concurrently with allopurinol without dose reduction. Aminosalicylates may inhibit TPMT activity, and it may be prudent to minimize or avoid such medications in patients taking thioguanine.
Hydroxyurea was first synthesized in 1869, and through the years it has been used to treat a variety of conditions, including hematologic malignancies, sickle cell anemia, and psoriasis.
Hydroxyurea impairs DNA synthesis through inhibition of ribonucleotide diphosphate reductase, an enzyme that reduces nucleotides to deoxynucleotides. This inhibition limits the supply of DNA bases available for synthesis. Strand breakage and cell death result. Hydroxyurea also prevents cells from repairing damage from UV or ionizing radiation, acting as a radiosensitizer. Finally, hydroxyurea yields hypomethylation of genes, altering expression,66 and this may contribute to normalization of psoriatic skin through improved keratinocyte differentiation. Hydroxyurea is most active in cells with a high proliferative index. It is preferentially concentrated within leukocytes.
Hydroxyurea is a small molecule that is well absorbed after oral administration. Serum levels peak within 2 hours of dosing. Hydroxyurea has a rapid onset of action, with tissue effects noted within 5 hours. The actual metabolism of hydroxyurea is incompletely understood, but at least 80% is excreted by the kidney. Within 24 hours of dosing, negligible amounts of hydroxyurea remain in the body.
In dermatology, hydroxyurea is used chiefly for treatment of psoriasis (Box 227-10). Efficacy has been demonstrated in plaque, pustular, and erythrodermic forms. Still others believe hydroxyurea is only moderately effective and prefer to reserve use as a maintenance therapy once initial clearance has been achieved via other modalities.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree