Cutaneous Manifestations of Drug Abuse: Introduction
|
Introduction
Drug abuse and addiction can be suspected or diagnosed on the basis of mucosal and cutaneous findings. The administration of drugs may cause cutaneous stigmata and eruptions predominantly through local or systemic, toxic or hypersensitivity-induced effects as a result of the drug itself, adulterants, infectious agents, or the mode of drug delivery.
Definitions
Illicit drug use is a maladaptive pattern involving self-administration of prescribed or recreational drugs. Chipping is a lay term used to describe a pattern of drug use in which the user is not physically dependent, but rather sustains “controlled use” of a drug. A certain percentage of users will progress to drug dependence, a physical and/or psychological need for the effects of a chemical in order to avoid withdrawal symptoms associated with abstinence (Box 105-1). Drug dependence often leads to drug abuse, an intense desire to recurrently obtain increasing amounts of one or more chemical substances to the exclusion of all other activities, resulting in clinically significant physical, emotional or social distress (Box 105-2). Tolerance defines a physiologic state in which progressive increases in the dose of a drug are needed to achieve the effects previously experienced at smaller doses. Some drugs chiefly induce physical dependence, while cause predominantly psychological dependence.1
The presence of three or more of the following, occurring any time in the same 12-month period:
|
Adapted from American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders IV-TR, 4th edition. Washington DC, American Psychiatric Press, 2000. |
The presence of one or more of the following, occurring within a 12-month period:
|
Adapted from American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders IV-TR, 4th edition. Washington DC, American Psychiatric Press, 2000. |
The National Institute of Drug Abuse (NIDA) (http://www.drugabuse.gov/)2 considers the following agents to be drugs of abuse in the United States:
- Alcohol
- Club drugs
- Cocaine
- Heroin
- Inhalants
- Lysergic acid diethylamide (LSD)
- Marijuana
- 3,4-Methylenedioxymethamphetamine (MDMA, Ecstasy)
- Methamphetamine
- Phencyclidine (PCP)
- Prescription medications
- Steroids (anabolic)
- Tobacco
Epidemiology
In 2004, the United Nations’ World Drug Report estimated that between 3% and 5% of the global population used illicit drugs.3 In 2008, the National Survey on Drug Use and Health in the United States estimated that:
- 20.1 million Americans aged 12 or older (8% of that population) were currently using illicit drugs including marijuana/hashish, cocaine, crack, heroin, hallucinogens, inhalants or prescription-type psychotherapeutics.
- Marijuana was the most commonly used illicit drug (15.2 million past month users).
- The most commonly injected drugs were heroin and cocaine.
- Almost 2 million current cocaine users, comprising 0.7% of the population, were estimated.4
- The actual number of individuals who use heroin is difficult to determine because there has been a growing tendency to sniff, snort or smoke rather than to inject heroin intravenously or subcutaneously.
- An estimated 70.9 million Americans (28.4%) aged 12 or older were current users of tobacco in any form.
- Of Americans aged 12 and older, 51.6% had consumed alcohol at least once in the 30 days prior to being surveyed; 23.3% reported drinking heavily (>5 drinks on >5 occasions).
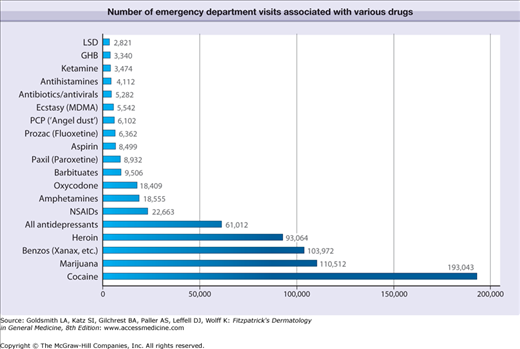
The drugs most commonly associated with emergency department visits in 2001 included cocaine, marijuana, benzodiazepines and heroin, in that order (Fig. 105-1).
Figure 105-1
Number of emergency department visits associated with various drugs. Cocaine, marijuana and benzodiazepines were the most common drugs associated with emergency department visits in 2001. Data from the United States Substance Abuse and Mental Health Services Administration, 2001, http://thedea.org/statistics.html.158
Pathogenesis
Studies in concordant twins have shown a strong influence of genetic inheritance on the susceptibility to drug use.5 The potential of a drug to cause addiction varies. The processes by which genes regulate physical reactions to addictive drugs have not been clearly elucidated. Repeated exposure to cocaine causes a change at the level of gene expression that leads to altered levels of the specific brain protein called cyclin-dependent kinase-5. This protein regulates the action of dopamine, which potentiates the euphoric effects of cocaine and other drugs.6 Narcotics disable the neurons that normally inhibit the release of dopamine while amphetamines and cocaine increase dopamine signaling, either by directly stimulating its release, or by blocking its absorption. Environmental factors such as history of sexual abuse during childhood, severe family dysfunction with drug abusing, detached or mentally ill parents, poor social skills, and drug-using peers are also clearly important.
The mechanisms of addiction, tolerance and dependence are complex. Addictive drugs flood the synapses of the mesolimbic system, especially the nucleus accumbens, with excessive amounts of dopamine, augmenting the hedonic tone and producing a euphoric state. The subsequent pleasurable reactions of the frontal cortex, amygdala, and hippocampus are exaggerated. The association of drug use and euphoria in these brain areas is reinforced with each exposure until the user no longer controls behavior, at which point addiction has resulted.7 Chronic users have sustained activation of the cAMP response element-binding (CREB) protein, a trigger for the production of dynorphin and other proteins that shut off dopamine release, preventing the individual from finding pleasure in usually enjoyable activities and requiring subsequent fixes with higher doses of drug to overcome the effects of tolerance. Addictive drugs also inhibit or excite neuronal activity in various areas of the nervous system. To compensate for these alterations, neuroadaptation develops with either formation of new neuroreceptor sites or diminished synthesis and sensitivity of neurotransmitters and neuroreceptor sites. Discontinuation of the drug reverses the neuroadaptation process and results in an exaggerated neural response that produces withdrawal symptoms.
Clinical Findings Associated with Commonly Used Drugs
Ethyl alcohol, or ethanol, is the intoxicating ingredient found in alcoholic beverages. It is a central nervous system depressant that impairs brain function and motor skills and is rapidly absorbed from the stomach and small intestine into the bloodstream. Heavy use can increase the risk of liver disease, stroke and certain cancers.
Direct liver toxicity of alcohol can cause hepatomegaly, jaundice, shrunken liver in the setting of cirrhosis, and hypoalbuminemia leading to Muehrcke lines and Terry nails (see Chapter 89). Hyperestrogenemia can lead to gynecomastia, palmar erythema, spider angiomata, and testicular atrophy. Portal hypertension secondary to alcohol-induced liver cirrhosis can lead to an enlarged spleen, ascites, variceal bleeding, hemorrhoidal bleeding and caput medusae. Dupuytren contractures due to fibroblastic proliferation and disorderly collagen deposition may be seen in 66% of alcohol abusers. Asterixis and confusion are seen in patients with hepatic encephalopathy. Alcohol withdrawal delirium, also known as delirium tremens, is characterized by tachycardia, hypertension, body temperature elevation and delirium. Ataxia, confusion and lateral gaze palsy are indications of Wernicke encephalopathy. Wernicke encephalopathy followed by anterograde and retrograde amnesia along with confabulation characterize Korsakoff syndrome.
Club drugs include γ-hydroxybutyric acid (GHB, date rape drug), flunitrazepam (Rohypnol®, roofies), ketamine, MDMA, and LSD (Table 105-1). These drugs tend to be used by teenagers and young adults in social settings. In 2008, NIDA showed that among 12th graders, 1.3% had abused flunitrazepam, 1.2% had abused GHB and 1.5% had abused ketamine at least once in the year prior to their being surveyed.8 GHB is sedating and can cause coma and seizures. It is being used increasingly by bodybuilders, who believe that it helps to metabolize fat and build muscle. Flunitrazepam is also sedating and can incapacitate users and cause amnesia; when combined with alcohol, this drug can be lethal. Ketamine distorts perception and produces feelings of detachment from the environment and self.
Drug | Street Namesa | Route of Administration |
|---|---|---|
Alcohol | Booze Brew Juice | Ingestion |
Anabolic steroids | Gym candy Juice Pumpers Stackers | Ingestion Injection |
Betel | Bunga (Tagalog) Cau (Vietnamese) Jambe (Javanese) Kunya (Burmese) Paan (Sanskrit) Supadi (Nepali) Shupari (Bengali) | Chewed |
Tobacco | Bogie, cancer stick, cigs (cigarettes) Chaw, snuff, chew (smokeless tobacco) | Chewed Smoke inhalation |
Club Drugs | ||
GHB | Fantasy G Georgia Home Boy Liquid ecstasy Soap | Ingestion |
Flunitrazepam | Roofies | Ingestion |
Ketamine | Jet Special K Vitamin K | Ingestion |
Cocaine | Blow Coke Crack Flake Snow | Nasal inhalation Injection Transdermal application |
Heroin | H Junk Ska Smack | Injection Smoke inhalation |
Inhalants | Poppers Snappers Whippets | Inhalation |
LSD | Acid Blotter Dots | Ingestion |
Marijuana | Ganga Grass Mary Jane Pot Reefer Weed 420 | Smoke inhalation Ingestion |
MDMA | Adam E Ecstasy Love X XTC | Ingestion |
Methamphetamine | Chalk Crystal Glass Ice Meth Speed | Ingestion Injection Nasal inhalation Smoke inhalation |
Phencyclidine | Angel dust Fuel Ozone PCP Rocket Wack | Ingestion Nasal inhalation Smoke inhalation |
Prescription medications: Opioids, CNS depressants, stimulants | Dust, dillies (dilaudid) Emsel, God’s drug (morphine) Oxy, cotton (oxycontin) Rids, vitamin R (Ritalin) | Ingestion |
Cocaine (benzoylmethylecgonine) is an alkaloid extracted from the leaves of the coca plant Erythroxylon coca.9–15 It is a powerful sympathomimetic, vasoconstrictor, local anesthetic, and stimulant. Cocaine hydrochloride is a powder that can be can be nasally inhaled or injected intravenously or subcutaneously, also known as “skin popping” (Fig. 105-2). Crack cocaine or “crack,” the freebase rock crystal form of cocaine hydrochloride, is smoked (Table 105-1). Freebase refers to the pure basic form of an amine, as opposed to its salt form. The amine is usually a natural alkaloid product.
Cocaine can produce intense vasoconstrictive effects by directly stimulating the central nervous system and increasing peripheral catecholamines. The vasospastic action of cocaine is greatest at one hour after use and can be associated with ischemia, infarction and hemorrhagic injuries of most organ systems including the skin.16–18 The ischemic effects of cocaine in the skin can lead to acute multifocal skin necrosis,19 chronic skin ulcers,20 cutaneous fibrosis,21 blackened hyperkeratotic “crack hands”22 and claw-like “parrot beak” curvature of the nails. These changes are commonly found in association with pernio and some atrophy of the distal portions of the digital pulp secondary to ischemia. At skin-popping sites, there may be central pallor surrounded by ecchymosis due to the vasoconstrictive properties of cocaine acting locally at the injection site with hemorrhage occurring in the surrounding tissue. Skin popping is a method of drug administration whereby a substance is injected subcutaneously or intradermally, but not intravenously and not typically intramuscularly. Individuals with vasomotor instability are more susceptible to these types of reactions.23
Inadvertent or deliberate direct intraarterial injection of cocaine can cause severe tissue ischemia and necrosis via direct vasoconstriction. Individuals experience an initial intense burning pain, followed by cyanosis and marked edema. Compartment syndrome may also result. In the most severe cases necrosis leads to amputation.24,25 Skin popping also puts one at risk for developing secondary amyloidosis.
Cocaine-induced vasospasm may cause major internal organ injury including acute myocardial ischemia, cerebrovascular accidents, renal infarction26 and splenic infarction.18,27 Vasoconstriction of mesenteric vessels and the direct toxic effect of cocaine on gastrointestinal mucosa can result in acute abdominal crises (known as crack belly) secondary to perforations, intestinal ischemia and infarction.28,29
Various vasculitic and vasculopathic processes have been associated with cocaine use including pseudovasculitis,30 urticarial vasculitis,31 Churg–Strauss vasculitis,32 Raynaud phenomenon,33,34 Henoch–Schonlein purpura, necrotizing vasculitis35,36 and Buerger disease (see Chapters 163, 164, and 173).37,38
The local anesthetic properties of cocaine make it difficult for individuals to feel traumatic injury. This leaves users prone to repetitive trauma from the irritant properties of the drug itself and implements of drug delivery, thus exposing them to an increased risk of infection.39 Missing a vein and injecting into the surrounding tissue creates a niche environment in which bacteria can thrive.40 Repeated needlesticks increase the likelihood of cutaneous infection and transmission of blood-borne viruses.41
Mucosal manifestations of ischemia secondary to cocaine inhalation or smoking include dental caries,42 gingival recession,43 oral blisters44 and nasal and palatal perforation.45 Insufflating (snorting) cocaine may lead to recurrent epistaxis, intranasal crusting, rhinitis and chronic sinusitis.42,46 Inhalation utensils themselves can act as vectors for viruses and may induce “snorter’s warts.” Nasal septum perforation reduces nasal support and results in a broad, flat nose or “saddle nose deformity.”46–49 Nasal septum perforation typically occurs prior to development of palatal perforation. Cocaine burns of the upper airway are associated with hoarseness, dysphonia, odynophagia, dysphagia and stridor.23,26,50–53 Crack cocaine smoke has a direct toxic effect on the corneal epithelium of the eye. Repeated exposure to the alkaloid smoke may cause an irritant effect leading to excessive eye rubbing and subsequent infectious complications, and chemical burns.51
Drug reactions including acute generalized exanthematous pustulosis54 and Stevens–Johnson syndrome 55 have also been reported.
The stimulant properties of cocaine are associated with increased metabolism and dramatic weight loss.56 Psychiatric conditions, most commonly delusions of parasitosis and subsequent formication are experienced approximately 20% of the time in cocaine users (also known as coke bugs)57 (see Chapter 104). Recent reports have emerged of febrile agranulocytosis and often vasculitis with prominent involvement of the ear lobes secondary to cocaine adulterated with levamisole, an anthelmintic medication used in veterinary medicine to control parasites in livestock.58,59
Natural and semisynthetic derivatives of the opium poppy are known as opiates. Biologically natural opiates include morphine and codeine, while semisynthetic opiates such as heroin and hydromorphone are derived from biologically active opiates. Diacetylmorphine, or heroin, crosses the blood–brain barrier and binds opioid receptors in the brain, resulting in its euphoric, analgesic and anxiolytic effects. Heroin is the most common parenterally injected illicit drug, either by intravenous or subcutaneous (skin popping) administration. Heroin may also be inhaled. With a peak “rush” at 7–8 seconds, it is the fastest-acting and via smoking most potent opiate, accounting for up to 90% of opiate use in the United States.
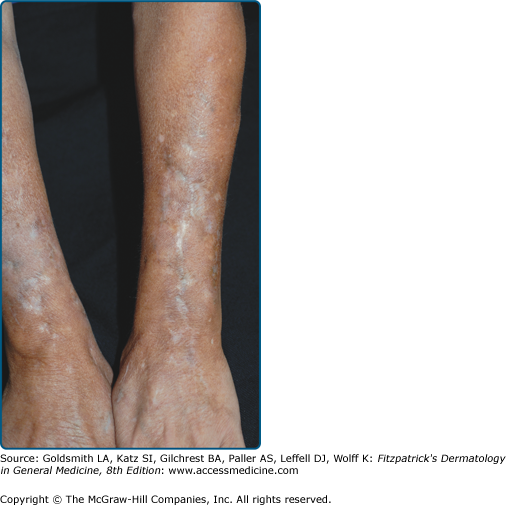
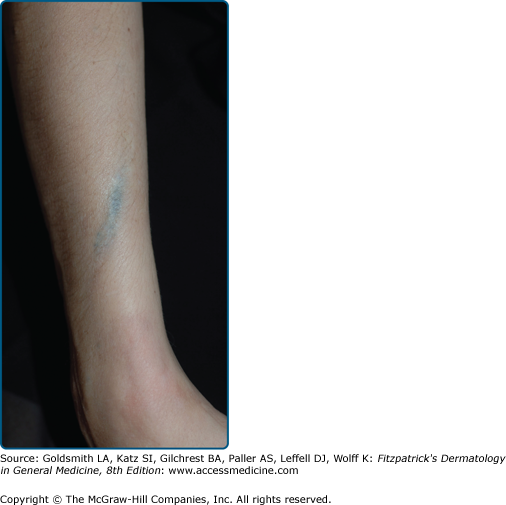
Scarring is the primary cutaneous stigma of injection drug use. The antecubital fossa is the usual starting point of intravenous drug use, followed sequentially by the upper arms, hands, neck, feet, legs, groin and digits.60 Linear cord-like scars along a vascular distribution (track-marks), are formed after repeated injections along a superficial vein, resulting in venous thrombosis and subsequent fibrosis.61 (Fig. 105-3) Skin popping scars are irregular round hypopigmented or hyperpigmented, atrophic or hypertrophic scars or keloids.62 (see Fig. 105-2) Soot tattoos or shooting tattoos result from soot deposition or the introduction of foreign materials in the dermis after “cooking” of the drug and/or flaming of needles (Fig. 105-4).63
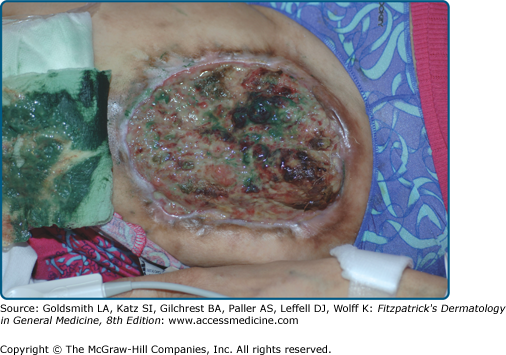
Diluting or “cutting” heroin to retail “street strength” is a common practice. Common diluents for white powder heroin include quinine, lactose, lidocaine, caffeine, lemon juice, inositol, dextrose, sucrose, procaine, starch, magnesium silicate and mannitol.64 Diluents may cause lymphatic destruction, foreign body granulomas, cutaneous nodules, ulcerations, panniculitis and dermal sclerosis secondary to irritation and dermal inflammatory processes (Fig. 105-5).65–67 The subsequent vascularized granulation tissue in and around chronic ulcers may be used as a site for drug injection.20 (see eFig. 105-5.1) Black tar heroin is a dark, gummy form of heroin that is less refined and cheaper than the white powder variant. It is mixed with a variety of diluents including dextrose, burnt cornstarch, instant coffee and dirt.68 The mixture may also contain dust and pathogens introduced during the process of manufacturing or storage.64,66 Irritant substances can also cause sterile chemical cellulites and abscesses.
eFigure 105-5.1
Chronic ulcer at site of repeated cocaine injection. Repeated cocaine injection and subsequent chronic vasoconstriction at this site contributed to the formation and persistence of this significant ulcer. The highly vascularized overlying granulation tissue provides an excellent site for efficient injection drug use. The wound is dressed with Panafil® ointment, a compound containing papain, urea and chlorophyllin copper complex which was used at one time for its debriding properties.
Cutaneous infections are common in injection drug users (Table 105-1). Skin popping and black tar heroin use are associated with cutaneous necrosis and necrotizing ulcers.69–72 An increase in Clostridial infections including wound botulism due to Clostridium botulinum, tetanus due to Clostridium tetani, and rapidly progressive myonecrosis with a fulminant shock syndrome due to Clostridium sordellii have been observed with the use of black tar heroin in California.73–76
Fungi have been cultured from confiscated heroin specimens.77 Systemic candidosis characterized by painful nodules and pustules on the scalp and hair-bearing areas, chorioretinitis or uveitis, and costochondritis has been described in individuals injecting brown heroin diluted with lemon juice.78
Inhaling smoke and then exhaling it into another individual’s mouth (known as shotgunning) is associated with efficient transmission of respiratory pathogens. 79
Opiates induce histamine release that results in subsequent pruritus that starts almost immediately after heroin injection and can last 10 minutes to 24 hours.80 Urticaria, severe angioedema and bronchospasm have also been reported with heroin use.80
Rare morbilliform eruptions, fixed drug eruptions and a case of toxic epidermal necrolysis have also been reported.62,64,81 Adulterants are thought to be responsible for most of these reactions.
Secondary systemic amyloidosis is an important cause of renal disease in heroin users. Its pathogenesis is thought to be associated with chronic antigenic stimulation and prolonged inflammation secondary to cutaneous infections. Patients were observed to progress to end stage renal disease over several months to 3 years.82
3,4-methylenedioxymethamphetamine (MDMA, ecstasy), along with lysergic acid diethylamide (LSD) and hallucinogenic mushrooms, is one of the most commonly used illicit hallucinogens (Table 105-1). More than 7 million persons have tried MDMA at least once in their lifetime. MDMA is a synthetic stimulant with psychoactive properties that acts both by causing a massive synaptic release of serotonin, and to a lesser extent dopamine and norepinephrine, as well as inhibiting the reuptake transporters within the synapse. Its short-term effects include inducing euphoria, a sense of enhanced intimacy with others, and diminished anxiety and depression. Adverse health effects can include nausea, chills, sweating, teeth clenching, muscle cramping, and blurred vision. MDMA is usually ingested, but may be injected or inhaled with effects lasting for 3–6 hours. It is frequently used in combination with alcohol, cannabis, amphetamine or cocaine, resulting in unpredictable effects.83
MDMA is associated with xerostomia and is therefore often coupled with soft drinks, which may lead to dental caries. The neurotransmitter release associated with MDMA induces bruxism, trismus and teeth grinding that can wear down tooth enamel. Direct application of MDMA to the gums may cause necrotizing gingivitis and widespread perioral and intraoral swelling. MDMA can also interfere with systemic temperature regulation that can, rarely, be lethal.
Methamphetamine is a very addictive synthetic stimulant that affects the brain and central nervous system through the release of dopamine, norepinephrine, and serotonin. By concurrently blocking reuptake of these neurotransmitters, sensations of euphoria, lowered inhibitions, feelings of invincibility, and hyperactivity are produced.84 Metamphetamine a white, odorless, bitter-tasting powder that can be ingested orally, snorted or injected. It may also be smoked in its rock “crystal” form.85 Short-term effects include feelings of euphoria, decreased fatigue associated with difficult life situations, headache, difficulty concentrating, diminished appetite, abdominal pain, vomiting, diarrhea, disordered sleep, paranoid or aggressive behavior, and psychosis. Long-term use of methamphetamine use is associated with anorexia, neurotoxicity, neurodegeneration, and clinical depression that may lead to homicidal and suicidal ideation and action.85
An increased rate of skin and soft tissue infections have been reported in methamphetamine users, including increased rates of methicillin-resistant Staphylococcus aureus (MRSA) infections in noninjection drug users. Methamphetamine use is associated with formication that can lead to subsequent skin picking, skin breakdown, and portals of infection (see eFig. 105-5.2). Use of methamphetamine and other sexually stimulating drugs can also increase direct skin-to-skin sexual contact and transmission of MRSA86 (Table 105-1).
Methamphetamine users are at risk for developing meth mouth, or oral decay characterized by poor oral hygiene, xerostomia and rampant caries typically on the smooth surfaces of teeth, and excessive tooth wear.87 Methamphetamine use has also been associated with psychosis and subsequent self-injurious behavior including genital mutilation.88