Cosmetics and Skin Care in Dermatology: Introduction
|
According to recent data, the US sales of skin-care cosmeceuticals (cosmetics with attributed biologic effects) range between $3.5 and $6.4 billion, with forecasts of steady continued growth despite the global recession.1–3 A plethora of skin-care products are currently available to account for this substantial sales volume. The range of products and their associated claims is so extensive and complex that physicians and consumers are often confused about their indications and effectiveness. One approach to understanding these many options is to consider how the products are used to treat specific skin types.
For the purposes of choosing the most appropriate cosmetics and other skin-care products, facial skin can be grouped into four main categories that in practice represent up to 16 skin types: dry (D) or oily (O), sensitive (S) or resistant (R), pigmented (P) or nonpigmented (N), and wrinkled (W) or unwrinkled [or “tight” (T)]. These “skin types” are not static and can be affected by a range of intrinsic and extrinsic factors such as environment, aging, and disease. The key to proper skin-care recommendations is to take all four parameters into consideration. The various permutations of the four skin-type parameters yield 16 possible skin types. For example, a person may have dry, sensitive, pigmented, wrinkled skin, and her needs would significantly differ from someone with oily, sensitive, pigmented, and wrinkled skin.
This chapter discusses the basic science and defining characteristics of the four parameters. Certain extrinsic or intrinsic factors, such as a move to a different climate, a change in stress levels, pregnancy, menopause, and other stressors, can result in a skin type change. The Baumann Skin Type Indicator, a questionnaire developed to determine skin type, is helpful in assessing skin type initially and again after major life events.4
Skin Hydration
Xerosis or “dry skin” describes skin that is characterized by dull color (usually gray white), rough texture, and an elevated number of ridges.5 The etiology of this common condition is multifactorial. The most significant factor in the development of xerosis is the role of the stratum corneum (SC) and its capacity to maintain skin hydration. Rawlings et al showed that patients with dry skin have a perturbation in the lipid bilayer of the SC, which is associated with increased fatty acid and decreased ceramide levels.6 Defects or deficiencies in this barrier layer of the skin cause a spike in water evaporation, known as transepidermal water loss (TEWL). This leads to abnormal desquamation of corneocytes7 because desmosomes remain intact at higher levels of the SC, and desmoglein I levels remain elevated in the superficial SC of individuals with dry skin as compared to controls. This occurs because the enzymes necessary for desmosome digestion are impaired when the water level is insufficient, which leads to abnormal desquamation resulting in visible “clumps” of keratinocytes that cause the skin to appear rough and dry.8 Recent studies suggest that both the initial cohesion and the ultimate desquamation of corneocytes from the SC surface may be orchestrated by localized changes in pH, which selectively activate different classes of extracellular proteases in a pH-dependent fashion.9 Impairment of the lipid bilayer of the SC can be caused by various exogenous factors such as ultraviolet (UV) radiation, detergents, acetone, chlorine and prolonged water immersion.
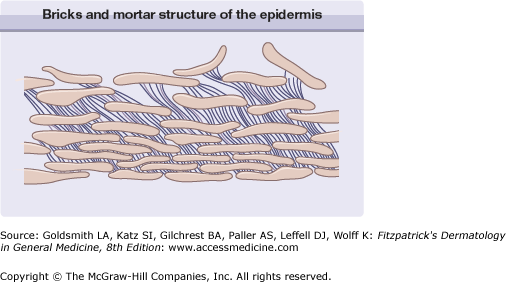
The SC is composed of three primary groups of compounds: (1) ceramides, (2) fatty acids, and (3) cholesterol. When present in the proper amount and balance, these components help protect the skin and keep it watertight (see Fig. 250-1). When the barrier is impaired, however, the skin is rendered dry, because of the inability to retain water, and sensitive, because of increased vulnerability to extrinsic elements. Several other factors play a causative role in dry skin.
Natural moisturizing factor (NMF), derived from the breakdown of the protein filaggrin, is integral in maintaining water within skin cells. Filaggrin provides structural support and strength in the lower layers of the SC. It is broken down in higher levels (stratum compactum) of the SC by a still-uncharacterized, cytosolic protease into free amino acids, including histidine, glutamine (glutamic acid), and arginine.10 These osmotically active amino acids remain inside the keratinocyte and avidly bind to water. The pace at which filaggrin is broken down into NMF is thought to be regulated by aspartate protease (cathepsin), which initiates this cascade and determines the amount of NMF that is present.11 Interestingly, this putative aspartate protease (cathepsin) is regulated by changes in external humidity. In other words, in low-humidity environments, the pace of NMF production increases. This acclimation process typically occurs over the course of several days12 and cannot yet be regulated artificially via products or procedures.
Hyaluronic acid (HA), which can bind 1,000 times its weight in water, is another substance found in the skin that may help it retain and maintain water. HA is produced mainly by fibroblasts and keratinocytes in the skin, and has an estimated turnover rate of 2–4.5 days in mammalians.13 HA is localized not only in the dermis but also in the epidermal intercellular spaces, especially the middle spinous layer, but not in the SC or stratum granulosum.14 Aged skin, which is less plump than youthful skin, is characterized by decreased levels of HA. The role of HA in skin hydration is not clear, and HA does not penetrate the skin upon topical application15; however, this has not stopped many companies from putting HA in topical skin-care products and claiming efficacy.
Aquaporin-3 (AQP3) is a member of a family of homologous aquaporin water channels that facilitate fluid transport. Other aquaporins in this family are well known to contribute to water transport in kidney and lung epithelia. AQP3 is a member of a subclass of aquaporins called aquaglyceroporins, which transport not only water but also glycerol and possibly other small solutes. AQP3 was recently found to be expressed at the plasma membrane of epidermal keratinocytes in human skin16 (eFig. 250-1.1). There is evidence for a high concentration of solutes (Na+, K+, and Cl−) and a low concentration of water (13%–35%)17 in the superficial SC, producing in the steady-state gradients of both solutes and water from the skin surface to the viable epidermal keratinocytes.18,19 Although transepithelial fluid transporting properties have been studied extensively in kidney and lung epithelia, the molecular mechanisms of fluid transport across epidermal keratinocyte layers remain poorly understood, as is the relationship between keratinocyte fluid transport and SC hydration. It has been proposed that AQP316 might facilitate transepidermal water permeability to protect the SC against desiccation by evaporative water loss from the skin surface and/or dissipate water gradients in the epidermal keratinocyte cell layer. Water permeability of human epidermal keratinocytes was inhibited by mercurials and low pH, consistent with the involvement of AQP3.16 A study20 looking at skin phenotype in transgenic mice lacking AQP3 showed significantly reduced water and glycerol permeability in AQP3 null mice proving that AQP3 is functional as a plasma membrane water/glycerol transporter in the epidermis. Conductance measurements showed remarkably reduced SC water content in AQP3 null mice in most areas of the skin. However, epidermal cell water permeability is probably not a major determinant of SC hydration because water movement across AQP3 is very slow compared with other tissues.21 Pharmacologic manipulation of AQP3 may be used in the future to treat skin disorders of excess and decreased hydration. At this time, only Ajuga turkestanica extract has been shown to play a role in regulating AQP3.22 Ajuga turkestanica is found as an ingredient in a high-end line of skin-care products.
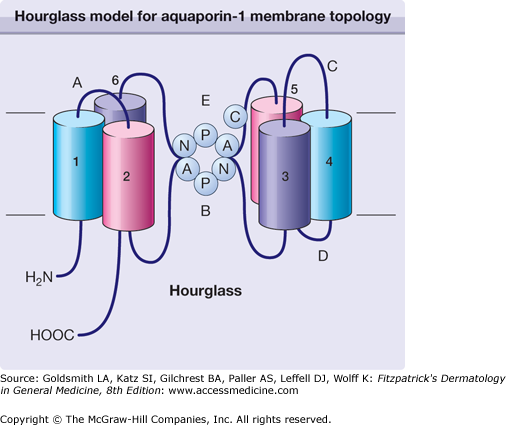
eFigure 250-1.1
Hourglass model for aquaporin-1 membrane topology. Each aquaporin-1 subunit contains six bilayer-spanning domains composed of two obversely symmetric structures (TM1–3, hemipore 1; and TM4–6, hemipore 2). When NPA [formed by amino acids asparagine (N), proline (P), and alanine (A)] motifs in loops B and E are juxtaposed, they form a single aqueous channel spanning the bilayer (the “hourglass”) flanked by the mercury-sensitive residue (C189). (Redrawn with permission from the Annual Review of Biochemistry, Volume 68©, 1999 by Annual Reviews, .)
Sebum production may also be a factor in the pathogenesis of xerosis. The oily secretion of the sebaceous glands contains wax esters, sterol esters, cholesterol, di- and triglycerides, and squalene,23 and is thought to confer protection to the skin from environmental influences and, when production is decreased, play a part in dry skin.24 Because sebaceous-gland-impoverished skin, such as that in prepubertal children, exhibits normal basal barrier function,25 it has been assumed that sebum does not influence epidermal permeability barrier function. Furthermore, when sebaceous glands are involuted pharmacologically with supraphysiologic doses of isotretinoin,26,27 both barrier function and SC lamellar membranes remain unaltered.28 Although sebum levels may not influence barrier function, sebum may still play a role in dry skin types, especially dry, resistant types that exhibit dry skin but not increased skin sensitivity. Lipids from modified sebaceous glands in the eye, called meibomian glands, help prevent dry eyes by preventing tear evaporation29,30; therefore, it makes intuitive sense that sebum-derived fats form a lipid film over the skin surface, preventing TEWL. Credence is given to this theory by a study that examined permeability barrier homeostasis and SC hydration in asebia J1 mice that demonstrate sebaceous gland hypoplasia.31 Normal barrier function was found in these sebum-deficient mice and can be explained by the unaltered levels of the three key barrier lipids, ceramides, free sterols, and free fatty acids, as well as the persistence of normal SC extracellular membranes. However, the mice were found to have decreased SC hydration. These results show that an intact intercellular membrane bilayer system, although sufficient for permeability barrier homeostasis, does not always suffice for normal SC hydration. Interestingly, the researchers found that topically applied glycerol returned the SC to normal hydration levels. In normal skin, sebaceous gland-derived triglycerides are hydrolyzed to glycerol prior to delivery to the skin surface. Replacing this glycerol in sebum-deficient skin may be a way to decrease skin dryness in sebum-deficient individuals. Glycerol has also been shown to be effective in accelerating barrier recovery.32
Patients rarely complain about decreased sebum production. However, it seems certain that sebum production plays a role in dry skin. For example, prepubertal children (>2 years and <9 years) commonly display eczematous patches (pityriasis alba) on the face and trunk that disappear coincidentally with the onset of sebaceous gland activation. Conversely, increased sebum production, which results in oily skin that can lead to acne, is a common complaint. It is well understood that an age-related change is seen in sebaceous gland activity, with levels typically low during childhood, rising in the mid-to-late teens, and generally remaining stable for decades until trailing off in the seventh and eighth decades as endogenous androgen production declines.33 The level of sebum production is also influenced by diet, stress, hormone production, and, to a degree, by genetics. In a study of 20 pairs each of identical and nonidentical like-sex twins, the identical twins exhibited essentially the same sebum excretion rates, with significantly divergent acne severity, whereas the nonidentical twins differed significantly according to both parameters, implying both the genetic influence of sebum and the mediation of exogenous factors in lesion development.34
In the context of the oily–dry parameter, ideal skin is typically characterized by an intact SC with an intact barrier, sufficient NMF levels, normal levels of HA, normal expression of AQP3, and balanced sebum secretion. In skin that falls on the oily side of the spectrum, increased sebum secretion is usually the culprit. This may or may not be accompanied by acne. If acne is a concern, then the patient would also fall into the sensitive skin category and would be labeled as an oily-sensitive skin type. The skin-care treatments would focus on decreasing sebum with retinoids, decreasing skin bacteria with antibiotics, benzoyl peroxide or other antimicrobials, and adding anti-inflammatory ingredients. If acne is absent, the individual would be labeled as an oily-resistant skin type. Skin care would focus only on decreasing sebum production unless other parameters such as dyspigmentation and wrinkling are also factors. Oral ketoconazole35 and oral retinoids36 have been shown to decrease sebum secretion, but this has not been shown with topical agents. Sebum-absorbing polymers and talcs are also useful for camouflaging unwanted sebum in people with oily-resistant skin.
In skin that falls on the dry side of the continuum, one must decide which factors are contributing to the dry skin. Clues can be derived by looking at the other skin parameters. If a patient has dry and sensitive skin, it is likely that the skin barrier is impaired and care should be taken to use products that repair the skin barrier, such as those that contain fatty acids, cholesterol, ceramides and glycerol. If the skin is photodamaged and wrinkled as a result, decreased HA likely plays a role. Topically applied HA is not absorbed, so using skin-care products with HA is not helpful; however, studies have suggested that glucosamine supplements may contribute to an increase in HA levels.37 One small single-blind study showed improvement of wrinkles but no change in skin hydration so the role of glucosamine is unclear.38 Dry skin that endures ongoing sun exposure likely suffers from an impaired skin barrier and decreased levels of NMF. At this time, there are no products that increase NMF, so skin care should focus on repairing the skin barrier and providing adequate sun protection.
All patients with dry skin are advised to avoid harsh foaming detergents that remove hydrating lipids and NMF from the skin. These detergents are found in laundry and dish cleansers in addition to body and facial cleansers. All dry skin patients should also abstain from taking protracted baths, particularly in hot or chlorinated water. In addition, people with very dry skin are advised to use humidifiers in low-humidity environments and apply moisturizers two to three times a day and after bathing.
In addition to targeting the causes of dry skin, there are many moisturizers on the market that help hydrate the skin in a more basic or generic manner. These products can be categorized as occlusives, humectants, or emollients (Table 250-1).
Barrier repair
|
Occlusives
|
Humectants
|
Occlusives
Occlusives coat the SC to retard TEWL. An occlusive provides an emollient effect as well as decreases TEWL. The best occlusive ingredients currently available are petrolatum and mineral oil. Petrolatum, for example, has a water vapor loss resistance 170 times that of olive oil.39 However, petrolatum has a greasy feeling that may make agents containing it cosmetically unacceptable to many patients. Other commonly used occlusive ingredients include paraffin, squalene, dimethicone, soybean oil, grapeseed oil, propylene glycol, lanolin, and beeswax.40 These agents are only effective while present on the skin; once removed, the TEWL returns to the previous level. Interestingly, it is not desirable to decrease TEWL by more than 40% because maceration with increased levels of bacteria can result.41 Therefore, occlusives are usually combined with humectant ingredients.
Humectants
Humectants are water-soluble materials with high water absorption capabilities. They are able to attract water from the atmosphere (if atmospheric humidity is greater than 80%) and from the underlying epidermis. Although humectants may draw water from the environment to help hydrate the skin, in low-humidity conditions they may absorb water from the deeper epidermis and dermis resulting in increased skin dryness.42 For this reason, they are more effective when combined with occlusives. Humectants are also popular additives to cosmetic moisturizers because they prevent product evaporation and thickening, which increases the shelf-life of products. Some humectants have bacteriostatic activity as well.43 Humectants draw water into the skin, causing a slight swelling of the SC that gives the perception of smoother skin with fewer wrinkles. Examples of commonly used humectants include glycerin, sorbitol, sodium hyaluronate, urea, propylene glycol, alpha hydroxy acids, and sugars.
Emollients
These are substances added to cosmetics to soften and smooth the skin. They function by filling the spaces between desquamating corneocytes to create a smooth surface.44 Emollients provide increased cohesion causing a flattening of the curled edges of the individual corneocytes.45 This leads to a smoother surface with less friction and greater light refraction. Many emollients function as humectants and occlusive moisturizers as well. Lanolin, mineral oil, and petrolatum are examples of occlusive ingredients that also confer an emollient effect.
Skin Sensitivity and Cosmetic Intolerance Syndrome
Sensitive skin is much more challenging to describe than resistant skin. The latter is characterized by a strong SC that confers potent cutaneous protection, shielding the skin from allergens and irritating substances. As the term implies, resistant skin rarely exhibits erythema (unless overexposed to the sun) or acne (unless it is so affected due to stress or hormonal fluctuations). People with resistant skin can use most skin-care products without fear of developing an adverse reaction such as a rash, acne, or a stinging sensation. The disadvantages of such skin include an inability to detect different effects among cosmetic products and, more important, having too high a threshold for penetration, so that few products are likely to cross the SC and impart beneficial changes.
The concept and presentation of sensitive skin is much more complex. Data from the early 1990s suggested that more than 40% of people presenting to a dermatologist reported having sensitive skin.46 In fact, in a recent epidemiological study of 1,039 people not selected based on sensitive skin-related criteria, questionnaire results indicated that 68.4% of the study population stated that their skin was sensitive to some degree, 77.3% claimed sensitive facial skin, 60.7% claimed sensitive body skin, and 56.3% claimed sensitive genital skin.47 Healthy women of child-bearing age comprise the majority of people that complain about this type of skin. With increasing age, the incidence of sensitive skin appears to decline. There are numerous cosmetic products available that are marketed for sensitive skin. However, sensitive skin itself is a relatively complex dermatologic phenomenon.
Cosmetic intolerance syndrome is not a single entity but rather a symptom complex of multiple exogenous and endogenous factors and represents an extreme of the continuum of patients who complain of sensitive skin. The syndrome is an uncommon clinical phenomenon in which patients complain bitterly of facial burning and discomfort associated with application of most skin-care products. Their skin may show overt inflammatory changes, or symptoms may be subjective only. These patients seriously challenge the diagnostic skills and even empathy of practitioners because the severity of symptoms does not match objective signs of disease. Many patients affected with this syndrome have tried numerous cosmetics and topical medications.
Fisher48 coined the term status cosmeticus for the condition in which patients no longer tolerate the use of any facial cosmetic product. Some of these patients initially experience subjective or objective irritation in response to use of cosmetics and become intolerant to many other topical agents during the evolution of this disorder. Other patients have occult allergic contact dermatitis, allergic photocontact dermatitis, contact urticarial reaction, or a combination of these conditions. In such patients, causal agents can be documented by careful clinical review and patch testing.
Strictly observing a prolonged program of eliminating cosmetics is an important therapeutic intervention. Some patients are able to return gradually to using other cosmetics after 6–12 months. Subsequent additions to the skin-care regimen can be made one at a time every 2 weeks. For the final regimen, the number of cosmetics and frequency of their use should remain limited.
Other patients experience facial burning continuously, without showing objective signs. Cotterill49 described these patients as having “dermatologic nondisease.” Many of these patients have a disturbed body image or body dysmorphic disorder—that is, they complain of physical defects that lack objective evidence. Many are depressed and need psychiatric help, which they frequently reject.
Sensitive skin covers the same range of pathophysiology as cosmetic intolerance syndrome, but it is generally less severe. Most of these consumers manifest sensory skin irritation.
Indeed, there are four very distinct variations of sensitive skin: (1) acne type (prone to developing acne, black heads, or white heads); (2) rosacea type (featuring a tendency toward recurrent flushing, facial redness, and experiencing hot sensations); (3) stinging type (predilection to stinging or burning sensations); and (4) allergic type (more likely to exhibit erythema, pruritus, and skin flaking).
Each of these subtypes of sensitive skin presents a unique challenge to the practitioner regarding appropriate treatment and recommendations regarding over-the-counter cosmetic skin-care products. The common process among these four subtypes is inflammation. Therefore, treatments for any kind of sensitive skin should focus on reducing and eliminating inflammation. Treatment can be further complicated when a patient displays a proclivity toward more than one sensitive skin subtype.
Definitive data on the prevalence of acne in the United States or worldwide are challenging to collect, but acne is generally considered the most pervasive skin condition in the United States. An overwhelming majority of these patients, roughly 70%–80%, are adolescents and young adults between 11 and 25 years old.50 (Fig. 250-2.) Adult women manifesting a hormonal component to their acne comprise most of the remainder of acne sufferers. There are three primary factors in the pathogenesis of acne: (1) elevated sebum production (which falls into the oily skin type); (2) clogged pores, characterized by dead skin cells inside the hair follicles adhering more than in those without acne (increased sebum production may also play a role in causing these skin cells to clump); and (3) the presence of the bacteria Propionibacterium acnes. Although acne can be a dynamic condition with various causal pathways or contributing factors, the essential pathognomonic feature is that increased amounts of sebum cause dead skin cells in the hair follicles to adhere, thereby clogging the follicle and creating a papule or pustule. P. acnes then migrate into the hair follicle, attacking the collected sebum and dead skin cells. This stimulates the release of cytokines and other inflammatory factors that engender the inflammatory response with the clinical correlates of redness and pus.
Some skin and hair care cosmetics cause acneiform eruptions. Acnegenicity encompasses both comedogenicity, which refers to follicular keratin impaction,51 and papulopustular formation. The time course for the appearance of facial papulopustules and comedones is different: papulopustules may appear in just a few days, whereas the appearance of comedones is delayed. Considerable confusion derives from the testing techniques: for example, isopropyl myristate in concentrations as low as 10% in petrolatum rapidly induces comedones in the rabbit ear but yields papulopustules in humans. Even common emulsifiers such as sodium lauryl sulfate produce pustules in a dose-related manner. The mechanisms appear to be related in spite of varied morphology. The European Union’s ban on animal testing of final products, which took effect in March 2009, will result in stronger reliance on human testing, whether this takes the form of use tests or application of a cosmetic under occlusion to the back for 4 weeks and subsequent cyanoacrylate or cationic polymer biopsies (to identify microcomedones), or both.
In 1996, the clinical significance of cosmetics in precipitating postadolescent acne in women was called into question by one of the authors of the original paper on “acne cosmetica.”52,53 Consequently, it is best to advise female acne patients to keep their cosmetic regimen simple and gentle, using products from manufacturers who test for acnegenicity.
Typically afflicting adults between 25 and 60 years of age, rosacea affects tens of millions of Americans. Like acne, this condition is characterized by facial redness, flushing, and papules, but is also distinguished by the formation of prominent telangiectasias (see Fig. 250-3). Topical skin care for rosacea is primarily geared toward preventing exacerbation of the condition, and using anti-inflammatory ingredients to decrease inflammation. Ingredients with anti-inflammatory activity include feverfew, sulfur, zinc, sulfacetamide, quadrinone, niacinamide, licorice extract, cucumber extract, aloe vera, colloidal oatmeal, and chamomile (Table 250-2).
|
Burning, stinging, or itching caused by application of a cosmetic or topical medicament without detectable visible or microscopic change is termed sensory irritation. The afferent limb of this reaction is carried by C nerve fibers that are present throughout the dermis and viable epidermis. The stinging occurs on the face within an hour of application in susceptible individuals. In a segment of the population, this sensory response is caused by many ingredients at dosages that do not produce clinical objective irritation. Nonallergic stinging is a phenomenon that a discrete subset of people experience in response to certain triggers. Some patients may indeed be more sensitive than others and are referred to as “stingers” by dermatologists. Stingers do not have a higher incidence of atopy or dry skin, but do report frequent adverse reactions to cosmetics. Strontium nitrate and chloride inhibit sensory irritation caused by α-hydroxy acids, ascorbic acid, and aluminum salts.54 These blockers are incorporated into skin-care products such as those containing α-hydroxy acids.
Several tests have been devised to identify stingers or the stinging propensity. The lactic acid stinging test is a widely accepted standard method for evaluating individuals who report invisible and subjective cutaneous irritation. In an early study, Frosch and Kligman applied 5% lactic acid to subjects’ nasolabial folds during profuse sweating, which resulted in 20% of participants reporting an unpleasant sensation.55 In a similar study in which lactic acid (10%) was applied to nasolabial folds, Seidenari et al observed that individuals with “sensitive skin” experienced a much stronger stinging sensation than those in the healthy control group.56 The stinging sensation is not necessarily associated with erythema as many patients feel stinging without experiencing redness or irritation.57 However, patients with rosacea distinguished by facial flushing are more susceptible to stinging from lactic acid exposure. It is recommended that patients with the stinging subtype of sensitive skin avoid products that contain the following ingredients: α-hydroxy acids (particularly glycolic acid), benzoic acid, bronopol, cinnamic acid compounds, Dowicel 200, formaldehyde, lactic acid, propylene glycol, quaternary ammonium compounds, sodium lauryl sulfate, sorbic acid, urea, or vitamin C.