Cosmetic Applications of Nonablative Lasers and Other Light Devices: Introduction
|
Over the last 40 years, the explosive advancement of laser technology has revolutionized the treatment of numerous skin conditions. The principle of selective photothermolysis set forth in 1983 by Anderson and Parrish1 has formed the basis for the development of lasers that selectively target and destroy tissues containing water, hemoglobin, and pigment. Lasers exhibiting such selective action were first applied to improve various potentially disfiguring medical conditions such as port-wine stains, hemangiomas, and pigmented birthmarks. More recently, these same principles have been implemented in an effort to improve the cosmetic appearance of normal and aging skin. The principle of fractional photothermolysis (FP) set fort by Manstein and Anderson2 has further revolutionized nonablative and ablative resurfacing by improving safety and shortening patient recovery times. Because laser treatments target all aspects of photoaging, from ameliorating the appearance of fine and deep rhytides to softening skin texture and improving pigmentation and skin laxity, they are becoming an indispensable tool in the armamentarium of the cosmetic dermatologist. A thorough understanding of the benefits and limitations of each laser technique and the expectations and lifestyle of the individual patient allow the practitioner to achieve the most satisfying cosmetic results.
Nonablative Skin Rejuvenation
Skin rejuvenation by laser was originally performed with devices that resulted in the destruction or ablation of the epidermis and elements of the dermis. The demand for less invasive procedures with shorter recovery times than those of traditional ablative laser resurfacing has led to the development of nonablative laser surgery. Many of these systems emit light in the infrared portion of the electromagnetic spectrum (1,000–1,500 nm), which is absorbed by water in deeper tissues while leaving the epidermis intact. This type of dermal wounding stimulates new collagen and elastin formation, which can improve the appearance of skin with mild-to-moderate photodamage. In general, the results are not comparable to those achieved with ablative lasers, but many patients are willing to accept more modest clinical improvements in exchange for fewer side effects and shorter recovery times. The advent of fractional nonablative laser technology has enabled the delivery of higher energy fluences to treat a fraction of the skin surface. This technology generally allows more effective and safer treatments for photoaging compared to traditional nonablative lasers.
Proper patient selection is the key to successful nonablative laser resurfacing (see Chapter 251 for ablative laser procedures). Patients with realistic expectations who have mildly to moderately photodamaged skin are the best candidates for nonablative procedures. Results from nonablative laser treatments are generally gradual and progressive, with textural irregularities and pigment irregularities improving more than rhytides. Patients who seek immediate dramatic results are likely to be disappointed with the overall clinical outcome. The practitioner must distinguish and educate patients on the difference between static and dynamic rhytides. Static rhytides in general respond more favorably and completely to laser therapy whereas dynamic rhytides are best addressed with appropriate injection of available botulinum toxin preparations.
As with ablative laser resurfacing, the heat produced by nonablative systems can reactivate prior herpes simplex infections (Table 252-1). Patients with a strong history of herpes labialis should receive prophylactic oral antiviral medication before treatment. Although nonablative laser procedures have an extremely low risk of scarring, these risks are increased in patients who have received isotretinoin in the previous year. Therefore, these patients should not undergo nonablative resurfacing. Patients with darker skin phototypes may develop a temporary postinflammatory hyperpigmentation after nonablative laser treatment. In order to ensure a safe treatment and to minimize the risk of adverse reactions, practitioners must use appropriate energy settings and correct treatment techniques to avoid bulk heating (heat accumulation) and injury to the treatment area.
Nonablative laser resurfacing can be performed in the physician’s office, with both the patient and clinical personnel wearing proper eye protection.
Several visible-light lasers have been developed to target discrete chromophores to stimulate dermal remodeling (Table 252-2). One of the first approaches to photorejuvenation used pulsed dye lasers (PDL) emitting light at wavelengths of either 585 nm or 595 nm. The ability of PDL treatment to improve the appearance of hypertrophic scars, striae distensae, and acne scars suggests that PDL treatment stimulates new collagen formation. A small clinical study confirmed that a single treatment with a PDL (585 nm, 450 ms) induced clinical improvement in 75%–90% of mild-to-moderate rhytides and 40% of moderate-to-severe rhytides.3 Longer-wavelength lasers such as the 1,064-nm Q-switched neodymium:yttrium-aluminum-garnet (Nd:YAG) laser, the 1,320-nm Nd:YAG laser, the 1,450-nm diode laser, and 1,540-nm erbium:glass laser have also been shown to induce dermal remodeling. Multiple treatments are necessary at 2- to 4-week intervals. The effects are often gradual due to ongoing collagen formation, which may occur up to 6 months after the last treatment.
|
Treatment with intense pulsed light (IPL) devices, which emit a broad, continuous spectrum of light from 515 nm to 1,200 nm, has been shown to successfully rejuvenate photodamaged skin. Filters can be placed over the beam to eliminate the shorter wavelengths, which target hemoglobin and melanin, depending on the clinical application. Studies have shown that IPL treatment produces substantial clinical improvement in the dyspigmentation and telangiectasias that are associated with photoaging but only mild improvement in rhytides.4
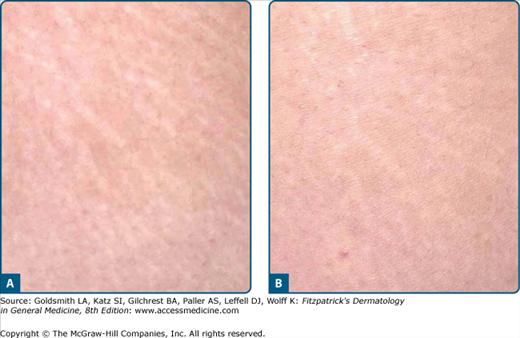
In contrast to visible-light lasers creating large sheets of thermal damage, the lasers used for fractional photothermolysis are mid-infrared (1,440 nm, 1,540 nm, 1,550 nm, 1,927 nm) devices that create columns of thermal injury to various depths into the dermis, similar to pixels in a digital photograph.5 The epidermis rapidly heals around these columns of thermal damage, which stimulate progressive collagen remodeling. Treatments are generally scheduled at 3- to 4-week intervals for a total of 3 to 6 sessions. Photodamage of the face, neck, chest, and hands; acne scars (Fig. 252-1); striae distensae (Fig. 252-2); and melasma have all been shown to respond to fractional photothermolysis.
Several nonablative devices that deliver energy deep into the dermis have been shown to cause skin tightening. The direct application of infrared light, with pretreatment and post-treatment contact cooling of the skin, has been shown to heat deep collagen to the point of contraction. In appropriate patients, this contraction results in a visible tightening of redundant skin. Skin tightening can also be achieved by the use of monopolar and bipolar radiofrequency devices generating electric current, which produces heat through resistance in the dermis. Periorbital rhytides and middle and lower face laxity generally require 1 to 3 treatments at 4-week intervals, with tightening noted 1–3 months after the last treatment6 (Fig. 252-3). A new infrared device that emits light at 1,100–1,800 nm in multisecond cycles has also been shown to induce skin contraction. Focused ultrasound has recently been incorporated into a device designed to generate dermal and subcutaneous heating with subsequent neocollagenesis in treated skin. Selective cryolipolysis is utilized by a novel noninvasive device to cool and selectively treat localized subcutaneous fat deposits.
Nonablative laser procedures are generally more easily tolerated than ablative procedures. The degree and type of anesthesia required depends on the patient’s pain tolerance and the amount of heat energy generated by the device. A topical anesthetic such as lidocaine or a eutectic mixture of lidocaine and prilocaine applied 1 hour before the procedure is usually sufficient. Forced-air cooling can also make the procedure more tolerable. Higher-energy procedures such as fractional photothermolysis occasionally require nerve blocks, oral or intramuscular analgesics, and anxiolytics.
Nonablative visible-light laser systems require different treatment parameters depending on the skin type and condition to be treated. To protect the epidermis, all of these devices are used in conjunction with a contact cooling handpiece or cryogen spray delivered several milliseconds before the laser pulse. IPL devices are used with various filters and at different energy levels depending on the desired treatment effect. A transparent water-based gel is used to protect the epidermis. Fractional photothermolysis is performed in the presence of forced-air cooling. Various density and energy settings are used depending on the indication and clinical endpoint desired.
Finally, tightening procedures are performed by holding the handpiece in firm contact with the treated skin. Several investigators have shown that multiple passes using radiofrequency at relatively low-to-medium energies are effective and more tolerable for patients than high-energy treatments.
Because nonablative laser treatments stimulate collagen remodeling over several months, objective clinical improvements after a series of treatments may take weeks or months to be achieved. Reassurance by the physician as well as the use of pretreatment photographs may help patients to better appreciate their progress. Setting realistic goals and targeting the aspects of photoaging that are important to the patient will also yield a more favorable outcome and enhance patient satisfaction.
Nonablative laser surgery is not without risks, but side effects are much milder than with ablative laser treatment. Depending on the treatment, patients may have erythema and edema, which resolves in hours to days. Rarely are treatments associated with blistering, transient hyperpigmentation, or scarring. In some cases, post-treatment hyperpigmentation has been caused by excessive use of cryogen spray but has resolved with topical bleaching agents. IPL treatment of tanned skin or darker skin phototypes should be used cautiously due to the increased risk of adverse events including blistering, hypopigmentation, and scarring. To avoid reactivation of latent herpes simplex virus (HSV) infections with fractional resurfacing, appropriate oral antiviral prophylaxis should be considered for all patients regardless of reported HSV status.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree