Correction of Capsular Contracture After Augmentation Mammaplasty By Conversion to the Subpectoral or “Dual-Plane” Position
Scott L. Spear
Michael Cohen
Introduction
As the surgical options for correcting capsular contracture and implant malposition have continued to evolve over the last decade, today’s surgeon has an increased armamentarium when faced with a patient with this problem (1,2,3,4). If the problem is one of capsular contracture, the surgeon may perform a capsulotomy or may attempt to remove as much of the capsule as is necessary. Similarly, if there is implant malposition, capsule may be excised and the implant pocket adjusted in an attempt to reposition the implant (5). All of these techniques, however, are limited by the original choice of implant location. Implants that are placed completely submuscularly will tend to migrate superiorly, whereas implants that are placed completely subglandularly will lose their superior fullness and tend to contract in a more inferior position with rounder shape. Often the solution to these problems is to relocate the implant to a new position entirely.
The dual-plane pocket offers a valuable alternative. Conversion to dual-plane positioning involves creating a subglandular space in the inferior one third of the breast and a confluent subpectoral space in the superior two thirds. This allows the implant to sit in a more appropriate position on the breast while enabling the breast tissue to redrape more naturally.
The purpose of this chapter is to describe a method developed over the last two decades of dealing with established capsular contracture. The method evolved from several years of experience with other procedures, which were not as reliable or consistently successful. By relocating implants to a subpectoral, or dual-plane, position, a more natural breast shape can be obtained with a low risk of capsular contracture or other complications.
Technique
To convert a patient from a subglandular or submuscular position to the dual plane, two things must be done. The new dual-plane pocket must be created, and the old pocket must be obliterated. This can be performed through the patient’s prior augmentation incision, whether periareolar or inframammary.
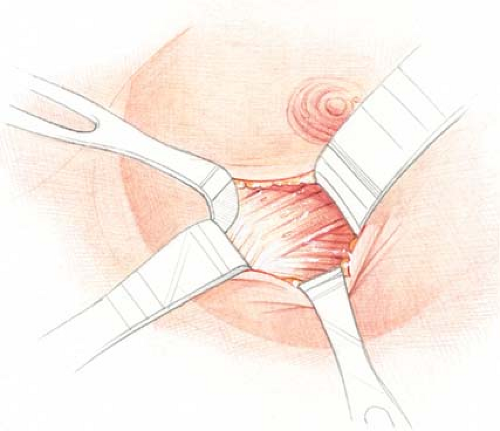
For those patients whose original implants were subglandular, a total or near-total capsulectomy is initially performed. The technique of leaving the capsule intact anteriorly to the pectoralis major is not recommended because it restricts the ability of the pectoralis major muscle to redrape over the implant. After removing as much capsule as technically and safely possible, the edge of the pectoralis major muscle is identified (Fig. 129.1) and a pocket dissected beneath the pectoralis major muscle using primarily sharp dissection with fiberoptic lighting and electrocautery and a minimum of blunt dissection (Fig. 129.2). The pectoralis major muscle is released entirely across its inferior origin, and the subpectoral pocket is dissected as far medially as necessary to achieve the desired pocket shape and medial breast border. The initial capsulectomy typically recreates a reasonable approximation of a desirable subglandular breast pocket. The subsequent release of the pectoralis major muscle along its lower border should extend as far medially as the space created by the capsulectomy, unless it is apparent that to do so the breast pocket would extend too far toward the midline. Progressive release of the pectoralis major muscle from inferiorly to superiorly along the sternal border should be done very judiciously if at all. Excessive medial release of the pectoralis major muscle along the sternum risks the creation of symmastia, window shading, or an unnatural medial breast fullness.
Laterally, the pectoralis major should be separated from the pectoralis minor and serratus anterior muscles with the dissection ultimately joining the subpectoral pocket with the space created by the capsulectomy. Any apparent excess space medially, inferiorly, or laterally is closed preferably with internal sutures. The new implant is then placed within the pocket such that the superior two thirds or so is in a subpectoral plane, leaving the inferior one third in the subglandular space (Fig. 129.3). Three to five one-half mattress stabilizing “marionette sutures” are placed between the skin and pectoralis major muscle to stabilize the inferior muscle edge at or near the level of the areola (Fig. 129.4). These marionette sutures are critical in closing off the upper portion of the previous subglandular space to prevent the new implant from dislodging back into the previous purely subglandular pocket.
For those patients whose original implants were primarily or entirely submuscular, the operation is quite different, and in particular capsulectomy is typically more selective. With use of the previous inframammary or periareolar incision, the operation begins by creating the subglandular portion of the new dual-plane, partly subpectoral pocket in a virginal space. Before entering the previous submuscular pocket, dissection thus proceeds in the subglandular plane from the level of the inframammary fold vertically up to the level of the inferior border of the areola. For patients with more soft tissue or ptosis, the dissection may go as far superior as the upper border of the areola. In patients with significant ptosis, a mastopexy may be required. This dissection creates the lowermost portion of a standard subglandular pocket and always exposes the inferior edge of the pectoralis major muscle. After creating this new
partial subglandular pocket, one identifies the inferior or lowermost border of the pectoralis major muscle. Dissection is begun along the lower border of the pectoralis major, which exposes the capsule of the existing submuscular implant.
partial subglandular pocket, one identifies the inferior or lowermost border of the pectoralis major muscle. Dissection is begun along the lower border of the pectoralis major, which exposes the capsule of the existing submuscular implant.
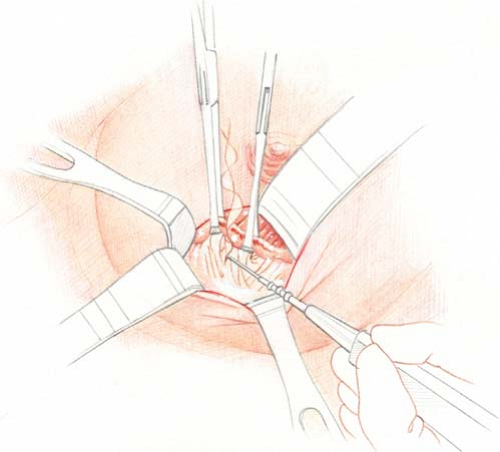 Figure 129.2. Elevation of a submuscular plane beneath the pectoralis major.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|