Facial trauma is a significant cause of morbidity in the United States. Despite the large volume of trauma surgeries at most academic institutions, there is still controversy regarding management of many traumatic injuries. The literature lacks clear-cut best practices for most fractures. In orbital trauma, there is debate about the optimal timing of repair, preferred biomaterial to be used, and the utility of evaluation afterward with intraoperative computed tomographic scan. In repair of mandible fractures, there is debate regarding open versus closed reduction of subcondylar fractures, or alternatively, endoscopic repair.
Key points
- •
There is debate about the optimal timing of repair, as well as material chosen to repair orbital floor fractures. There is a trend toward early repair in patients with large, displaced fractures and observation of smaller ones. When choosing a material to repair the fracture, the critical issue is the magnitude of the fracture, with large fractures requiring a stronger, supportive material.
- •
Intraoperative computed tomographic scan and intraoperative navigation are expensive technologies, but may reduce costs overall by decreasing the number of revision surgeries needed.
- •
There is still much debate about open versus closed repair of subcondylar fractures. Several studies have shown improvements in facial and ramus heights on the side of the open repair as well as improved occlusion with the open technique. Closed technique carries less risk for facial nerve injury and scar formation.
- •
Endoscopic-assisted subcondylar repair may be a compromise, allowing the benefits of open repair with lower risks. However, this technique is difficult and has a steep learning curve.
- •
Maxillomandibular fixation has been used for decades to achieve optimal occlusion during and after mandible repair, but there are new data suggesting this may not always be necessary.
Introduction
Facial trauma is a significant cause of morbidity in the United States. In one analysis, there were 407,167 Emergency Room (ER) visits for facial fractures with a cost approaching $1 billion. Despite the large volume of trauma surgeries at most academic institutions, there is controversy regarding management of certain traumatic injuries. The literature lacks clear-cut best practices with many fractures. In orbital trauma, there is debate about the optimal timing of repair, preferred biomaterial to be used, and the utility of intraoperative computed tomographic (CT) scans. In mandible fractures, there is debate regarding open versus closed versus endoscopic repair of the condyle. Maxillomandibular fixation (MMF) has been used for decades to achieve optimal occlusion during and after mandible repair, but there are new data suggesting this may not always be necessary. The purpose of this article is to review the salient points of each side of the debate and cite literature that exists to support each position.
Introduction
Facial trauma is a significant cause of morbidity in the United States. In one analysis, there were 407,167 Emergency Room (ER) visits for facial fractures with a cost approaching $1 billion. Despite the large volume of trauma surgeries at most academic institutions, there is controversy regarding management of certain traumatic injuries. The literature lacks clear-cut best practices with many fractures. In orbital trauma, there is debate about the optimal timing of repair, preferred biomaterial to be used, and the utility of intraoperative computed tomographic (CT) scans. In mandible fractures, there is debate regarding open versus closed versus endoscopic repair of the condyle. Maxillomandibular fixation (MMF) has been used for decades to achieve optimal occlusion during and after mandible repair, but there are new data suggesting this may not always be necessary. The purpose of this article is to review the salient points of each side of the debate and cite literature that exists to support each position.
Repair of orbital fractures
Timing
Yadav and colleagues noted that the rate of CT use in the US ERs quadrupled from 1996 to 2007. Patients totaling 4.1 million presented to an ER with, and were treated for, injuries of the eye and face. Of those, 20% (820,252 patients) underwent CT imaging, with 102,999 patients (12.5%) diagnosed with an orbital fracture. Another study reported that although the number of facial traumas has gone up between 1991 and 2007, the number of facial fracture repairs has decreased. Although this may in part be attributed to changing causes of fractures, it is likely that these trends are related to increasing use of CT imaging, resulting in decreasing severity of facial injuries being diagnosed. With an increase in the diagnosis of facial fractures, the question about which fractures should be repaired and which should be observed has grown more complex. For those that are repaired, what is the ideal timing of repair?
The 3 generally accepted categories of repair are immediate (within 24 hours), early (less than 2 weeks), and late (greater than 2 weeks). There is consensus on criteria that necessitate immediate repair. The first is activation of the oculocardiac reflex, with CT evidence of an entrapped muscle or periorbital tissue causing bradycardia, heart block, nausea, vomiting, or syncope. The second is entrapment of the perimuscular tissue with marked limitation of extra ocular movements on upward gaze. There is also a trend toward early repair in patients with large, displaced orbital fracture with increased orbital volume. Several investigators have demonstrated improved postoperative results, with decreased diplopia and enophthalmos by performing early intervention. It has been suggested that greater intrinsic damage leads to subsequent fibrosis, which results in poorer motility outcomes despite complete release of soft tissues. There is a suggestion that earlier intervention for such injuries might improve outcomes.
The real question then is, which patients need early orbital reconstruction and which patients are candidates for delayed repair? This uncertainty applies to patients with orbital fractures that have good ocular motility and only slight displacement of the orbital contents. The indication for surgery in solitary medial wall fractures is also controversial. Indications for surgery in these patients who do not have diplopia is usually the development of enophthalmos. However, enophthalmos rarely becomes significant (more than 2 mm) in the first 2 weeks after trauma. Although there is the Jaquiery classification, which describes the extent of the orbital fracture, and Hertel exopthamometry, the literature lacks a 3-dimensional volume-based classification to assist in clinical decision-making. At this time, there is not a clear definition of degree of injury that will or will not necessitate repair. For the patient who does undergo repair, there is some evidence for early repair, but this has not been proven conclusively. A review of the literature by Dubois found 4 studies that indicated some advantageous effects for surgery performed at less than 2 weeks for adults, although 5 studies found no significant differences. In pediatric patients, one study showed a correlation between earlier repair and diplopia and motility disorders, whereas 5 studies were inconclusive. In patients with small fractures, a watchful waiting approach may be appropriate, and surgery may be avoided in some cases.
Materials
The choice of reconstructive material presents another major decision in the care of a patient with an orbital fracture. A perfect biomaterial would be chemically inert, biofriendly, nonallergenic, and noncarcinogenic. It should also be cost-effective to place, readily available and able to be sterilized, and easy to handle, yet have the ability to be stable and retain its shape once manipulated. Preferably, it should be radiopaque to enable radiographic evaluation but without producing artifacts that may mask important features on subsequent radiologic examination. Unfortunately, this ideal graft material does not exist at this time. There are dozens of materials from which to choose.
Materials for repair can be placed into 5 main categories: autogenous, allogenic, alloplastic absorbable, alloplastic nonabsorbable, and xenograft. Autogenous grafts are usually bone, cartilage, or temporalis fascia. Bone grafts may be taken from iliac crest, calvarium, nasal septal bone, rib, maxillary, and mandibular bone. Bone grafts are a popular option because of the strength and rigidity of bone as well as the ability of the body to vascularize and incorporate the tissue with minimal immune reactivity. The major disadvantage of bone is that the rigidity does not allow contouring without fracture. When deciding on a harvest site, the following should be taken into account: iliac crest and rib bone show significant and unpredictable resorption, up to 80%, because of their endochondral origin ; calvarial bone remains a popular choice because of its accessibility and proximity to the surgical field, various sizes of grafts that can be harvested, and a hidden scar with minimal pain. One study illustrated the use of nasal septal bone, which restored orbital volume and alleviated symptomatic nasal passages.
Cartilage can be harvested from the nasal septum or the concha, with studies showing some preference toward septal cartilage. The advantages of cartilage compared with bone are that cartilage is easier to harvest and is more malleable, and the relative avascularity of this tissue allows for minimal oxygen perfusion and less resorption. The major limitation of this method is the limited size of the tissue harvested. Thus, cartilage is usually preferred for smaller defects. The use of temporalis fascia has been well described. This harvest site also offers minimal morbidity with a well-hidden scar. However, the lack of rigidity makes this material unsuitable for a large defect, and it is best for defects of the orbital floor measuring 2 cm 2 or less.
The use of allografts and xenografts has fallen out of favor because of risk of disease transmission and unpredictable absorption. Xenografts, such as collagen membranes of porcine origin, have a risk of disease transmission and an unpredictable rate of absorption and may not be sufficient for defects larger than 1 cm 2 . Allografts that have been historically used are demineralized bone, lyophilized dura, homologous fascia lata, and irradiated rib cartilage. Lyophilized dura was popular because of its strength, absence of donor morbidity, and lack of tissue reaction. Unfortunately, a patient was diagnosed with Creutzfeldt-Jakob prion disease, likely from a dura graft she got 6 years previously. There is also a theoretic risk of other disease transmission such as human immunodeficiency virus and hepatitis C. Furthermore, allografts have a rate of absorption higher than that of autogenous tissue.
Alloplastic materials can be divided into absorbable and nonabsorbable. Popular nonabsorbable materials include titanium, porous polyethylene, silicone, and polytetrafluoroethylene. These implants are popular because they are rigid, can cover a wide defect, and can be molded to fit the defect. Using computer assistance, titanium mesh can be custom designed for patient-specific defects. Absorbable materials include copolymers of polylactic acid and polyglycolic acid, and polydioxanone foil. Absorbable materials also have a high level of customizability and control, providing temporary support, leaving fibrous granulation tissue during their degradation. The risk that goes with all foreign body implantation is infection, foreign body reaction, or extrusion.
Several reviews have been done to evaluate the data on biomaterials. The results do not show a clear advantage of one material. Most studies are retrospective, and populations were ill defined, making it difficult to control for the variety of trauma patients in regards to age, mechanism of injury, and comorbidities that may affect healing. In addition, different surgical approaches to the orbit may affect healing, and there is a lack of long-term follow-up. Nonetheless, using the evidence available, investigators were able to produce some guidelines. The critical factor in choosing the right implant material is the magnitude of the defect, determined by the size of the fracture and the orbital volume change. In the case of small defects or linear fractures, the placement of a membrane may be suitable, whereas in larger defects affecting one wall or multiple walls, a stronger, supportive material may be necessary. For small defects, the choice of material is more dependent on biocompatibility. In larger defects, mechanical properties and the contour or form factor needs special consideration as well as biocompatibility.
Intraoperative Computed Tomographic Scans
Even with the ideal reconstructive material, the complex anatomy of the bony orbit makes precise reconstruction of orbital fractures and zygomatico-orbital fractures challenging. Inadequate repair of these injuries often results in excess orbital volume with postoperative diplopia and globe malposition. Intraoperative imaging plays a crucial role in orthopedic surgery during the repair of long bone fractures, giving immediate feedback and allowing for further reduction and corrections to be made while still in the operating room. Given the complexity of the facial skeleton, a transfer of this technology to maxillofacial trauma repair seems logical.
Use of intraoperative CT scanning has been reviewed by several investigators. Several investigators suggest using intraoperative CT in all cases of orbital or orbital zygomatic trauma, whereas others propose reserving the use of intraoperative cone-beam CT to aid in the reduction of complex or secondary zygomaticomaxillary (ZMC) repositioning after a failure of conventional techniques.
Those who argue in opposition of the use of intraoperative CT state cost, exposure to radiation, and additional time spent in the operating room. In regards to radiation exposure, the amount of radiation dosed with new technologies such as cone-beam CT is minimal. Daily background radiation is 8 mSv every 24 hours; cone-beam CT is 40 to 80 mSv, and FAN beam CT is 600 to 800 mSv (a 2-view chest radiograph is 100 mSv for reference). Furthermore, many surgeons will obtain postoperative imaging to evaluate reduction. Intraoperative CT obviates this.
A study by Shaye and colleagues investigated the amount of time used for intraoperative CT scan and found it to be a mean of 14.5 minutes. More importantly, the results of the CT scan led to revisions in 24% of patients, with 8 of 9 of them being classified as “complex” cases. This finding is consistent with the average of 18% revisions, which was calculated based on a meta-analysis. There is no way to determine how many of these cases would have required secondary revision at a later date had they not undergone revision in the operating room. This calculation is difficult to determine, because the threshold to perform revision is much higher once out of the operating room, and discrepancies seen on CT may not have contributed to a postoperative problem that would compel revision surgery. Nevertheless, given the high cost of revision surgery, it would take just a few secondary revisions to justify the cost of intraoperative CT.
A review by van Hout and colleagues set out to assess the value of intraoperative imaging on fracture repair and found that intraoperative imaging does have consequences on the surgical management of ZMC fractures. However, they did not find significant data regarding facial symmetry or fracture reduction. Although it is reasonable to assume that performing intraoperative revisions improves the quality of outcomes, the positive consequences of these revisions are merely implied and yet to be proven.
Use of Navigation Technology
A technique that has been described by several investigators is to “mirror” the normal anatomy of the uninjured orbit to the contralateral injured side and use this as a template for surgical repair. This mirror technique has been used in combination with surgical navigation. Surgical navigation shows promise and is particularly useful when one side of the face is unaffected. A CT scan represents the most appropriate imaging modality for cases of bone abnormality, which is generally the image modality of choice used in the ERs to diagnose these fractures on intake. Relying on symmetry of the face, the patient’s CT scan can be imported into the navigation system, and the unaffected side then undergoes an axial flip and is virtually mirrored onto the pathologic side. The navigation probe can be placed along the repair throughout the reconstruction to ensure accurate placement of the implant and/or bony pieces.
The advantage of this method is that the accuracy of the construct can then be assessed at any stage and again at the end of the process. Intraoperative CT remains less dynamic than navigation-assisted techniques, consequently delaying surgery and adding radiation exposure. In a facility that already uses a navigation system for neurosurgery or otolaryngology, using the system for maxillofacial trauma may be an easy and affordable addition. However, in a facility that is not familiar with the navigation system, there may be financial and technical difficulties initially. Another disadvantage of this technique is that there is, on average, 1 mm of error in registration in the periorbital area regardless of the method of registration. In addition, it requires a normal contralateral side, which is not often the case in panfacial trauma. A larger clinical series with long-term follow-up will be needed to determine reproducibility and cost-effectiveness.
Repair of mandible fractures
Open Versus Closed Treatment of Subcondylar Fractures
Mandible fractures are the most common facial fractures after the nasal bone. A large percentage of them require repair. Repair of mandible fractures has evolved significantly throughout the years. Techniques ranging from wire osteosynthesis, lag screw, compression, and noncompression plates have been used. Techniques of repair continue to evolve as new evidence becomes available. However, in some areas, the data show mixed results, and there is controversy among surgeons over best practice.
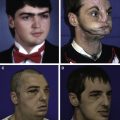
The anatomic distribution of fractures includes the angle, symphysis, condyle and subcondyle, and body. The area of mandible repair that sparks the most controversy is repair of the condylar fracture. Complications of condylar fracture include pain, restricted mandibular movement, deviation of the mandible, malocclusion, pathologic changes to the temporomandibular joint, osteonecrosis, facial asymmetry, and ankylosis. For many years, closed management and MMF were used to treat these fractures. It should be noted that closed management does not actually reduce these fractures and the term closed reduction is a misnomer. Closed management of these fractures includes stabilizing the fracture and re-establishing occlusion with MMF. This method was preferred treatment for many years. In recent years, open treatment of these fractures has become more common, likely because of advancements in the technology of plate and screw fixation devices and use of the endoscope. There is some evidence that this leads to better outcomes.
Most surgeons agree there are several absolute indications for open treatment. These indications were described in an article by Zide and Kent and include dislocation into the middle cranial fossa or external auditory canal, lateral extracapsular displacement, inability to obtain adequate occlusion, and open joint wound with foreign body or gross contamination. In addition, many investigators agree that other indications for open treatment include bilateral fractures and polytrauma, where there are fractures of other areas of the face that compromise occlusion and for which rigid fixation will be used. Similarly, most investigators agree that for mild or moderately displaced condylar fractures, conservative treatment with rigid or elastic MMF is generally adequate. The controversy comes when caring for the patient with a considerably displaced fracture. In 2003, the American Association of Oral and Maxillofacial Surgeons special committee on parameters of care developed indications for open reduction and added the following: physical evidence of a fracture, imaging evidence of a fracture, malocclusion, mandibular dysfunction, abnormal relationship of the jaw, hemotympanum, cerebral spinal fluid otorrhea, effusion, and hemarthrosis.
Several studies have attempted to answer the question of open versus closed reduction and to clarify the variables that help determine which approach may be most appropriate for each patient. Haug and Assael compared 10 patients who underwent open reduction internal fixation (ORIF) to 10 patients who underwent closed treatment with maxillomandibular fixation (CRMMF) and found that ORIF was associated with visible scars and CRMMF was associated with chronic pain. Ellis and Throckmorton compared vertical measure of facial morphology in patients with condyle fractures who had undergone either closed or open repair. They found that the patients treated with closed methods had significantly shorter posterior facial and ramus heights on the side of the injury compared with those treated with open reduction. The same group evaluated occlusal relationships of patients treated with closed or open techniques and found that those treated by closed techniques had a significantly greater percentage of malocclusion.
Villarreal and colleagues reviewed a series of 104 condyle fractures to determine what factors most influenced the clinical variables and postoperative result. They found that the principal factors that determined the treatment decision were the level of the fracture and the degree of displacement. The functional improvement obtained by open methods was greater than that obtained by closed treatment. However, open treatment increased the incidence of postoperative condylar deformities and mandibular asymmetry. Ellis and colleagues did another study and followed 61 patients who underwent ORIF for unilateral condyle fracture and found that despite being in good reduction after the initial repair, 10% to 20% of condylar processes had postsurgical changes of more than 10°, likely from a loss of fixation. Eckelt and colleagues performed a large randomized, prospective controlled trial of open versus closed treatment in 79 fractures. They examined clinical parameters such as mouth opening and protrusion; radiographic parameters, such as deviation of the fragment, shortening of the ascending ramus; and subjective functional impairment including pain and discomfort. They found that both treatment options for condylar fractures of the mandible yielded acceptable results. However, operative (open) treatment, irrespective of the method of internal fixation used, was superior in all objective and subjective functional parameters. Furthermore, they examined the data for each location of fracture (condylar base, condylar neck, condylar head). They found that although patients had less discomfort overall with ascending level of fracture, for all fracture types, open surgical treatment in connection with anatomically correct reduction and fixation of fragments resulted in significantly better outcomes on a uniformly high level.
Many surgeons recommend closed management because of problems with surgical approach, infection, injury to nerves and blood vessels, and scar formation. Marker and colleagues examined 348 patients who all underwent closed management to see if there were any variables predictive of complications. They found 3% had pain and 2% had malocclusion. Based on this, they determined closed management is safe and reliable in all but a few cases. Santler and colleagues examined 150 patients who were treated with either open or closed management and were examined at 2.5 years follow-up, they found that surgically treated patients showed significantly more weather sensitivity and pain on maximum mouth opening.
A review done by Nussbaum and colleagues was unable to provide definitive answers. They found numerous problems with the information presented in the various articles. These problems included lack of patient randomization, failure to classify the type of condylar fracture, variability within the surgical protocols, and inconsistencies in choice of variables and how they were reported. It is suggested that treatment type should be selected considering patient’s age, fracture type, patient’s systemic status, other facture, teeth, possibility of occlusal restoration by intermaxillary fixation, and existence of foreign materials. In the final determination of treatment plan, the advantage, disadvantage, risk of each treatment, and risk of complications should be sufficiently discussed with patients.
Endoscopic-Assisted Repair of Subcondylar Fractures
The above arguments illustrate the dilemma faced by the facial plastic surgeon. Many are dissatisfied with the potential complications of open reduction, such as facial scars and injury to the facial nerve, but there is also dissatisfaction with the results of closed management. Endoscopic approach to the subcondylar fracture offers the advantages of both techniques. In several comparison trials, endoscopic reduction has demonstrated equivalent results to open reduction in terms of anterior opening, mandibular deviation, posterior ramal height, and centric occlusion. The use of endoscopic assistance allows for minimal if any facial scarring, while also minimizing the risk of facial nerve injury. However, this technique is technically challenging, and there is a steep learning curve. The procedure may be time consuming, especially as the surgeon first attempts it. The senior author reviewed all cases of endoscopic subcondylar fractures and found that of the 48 patients undergoing the procedure, 2 had to be converted to open and 5 were reduced endoscopically but not plated. All of these unsuccessful attempts occurred during the early experience, illustrating the learning curve a surgeon encounters. They also found that this technique is not optimal for high neck, intracapsular issues, or those with medially displaced proximal segments. Although it does have some technical challenges, this is a reasonable alternative with lower morbidity compared with the standard extended open reduction.
Use of Maxillomandibular Fixation
The use of MMF has a long tradition. It is described in some version as far back as 1492, when the surgeon would “tie the teeth of the uninjured jaw to the teeth of the injured jaw.” However, in recent years, there has been a shift in repair techniques with MMF being used less often. In general, MMF is used to stabilize jaws while the fracture is healing and to establish correct occlusion. It is placed intraoperatively once occlusion is established, before the ORIF of the fracture. It is often left on for a period of weeks after surgery with wires as a way to stabilize the mandible in correct position, to ensure patient compliance with a liquid diet, or in the case of guiding elastics, to correct cases of minor malocclusion. There are recent data indicating that MMF may not be necessary in all cases. In several studies, it was demonstrated that MMF offered no advantages.
Postoperative maxillomandibular fixation
Regarding the use of postoperative MMF, in one study, the investigator who previously used MMF and then abandoned the practice compared complications and results in patients with and without postoperative MMF and found no significant difference. In 2 other retrospective studies, both using a matched pairing of identical fractures fixated with identical plating schemes with and without MMF, no significant difference was noted. Although it is suggested to use MMF in cases of high subcondylar, condylar, and comminuted fractures, in cases where good reduction is achieved and stabilized with a plate, postoperative MMF may not be needed.
Intraoperative maxillomandibular fixation
In another study, it was suggested that intraoperative MMF may also not be needed. In this review of a decade of trauma experience, it was noted that the use of MMF to achieve occlusion before ORIF had decreased annually, as manual reduction with ORIF became a preferred option. A comparison of the complications between the 2 methods showed no significant differences. Another study compared Erich arch bars, interdental stout wires, and manual reduction and found no significant differences infection, wound dehiscence, or symptomatic hardware requiring removal. These data suggest a shifting trend in mandible fracture management. Although arch bars are still the appropriate treatment for patients with subcondylar fractures, comminuted, significantly displaced, or multiple fractures, as well as midface fractures in addition to mandible fracture, data suggest that a select group of patients may be safely treated without arch bars.
Screw maxillomandibular fixation
Application of arch bars can be tedious, requiring significant time before the fracture repair begins. There is also the risk of blood-borne pathogens transmission via wire stick injuries to the surgeon and operating room staff. The impetus to develop faster and safer techniques to achieve MMF has led to advances in screw MMF. In these cases, the MMF screws are inserted into the bony base of both jaws between the canine and first premolar in all 4 quadrants. The screw heads act as anchor points to fasten wire loops or rubber bands connecting the mandible to the maxilla. In comparison to these tooth-borne appliances, MMF screws shorten the time to achieve intermaxillary fixation considerably and help to reduce the hazards of glove perforation and wire stick injuries. This technique is particularly effective for patients with good dentition and strong intercuspation.
On the downside, MMF screws are attributed with the risk of tooth root damage and a lack of versatility beyond the pure maintenance of occlusion. It is not recommended for use in cases that require stabilizing loose teeth, or fragments of the mandible and alveolar process. The increased distance the intermaxillary fixation wires must travel results in low vector control, which may lead to lingual rotation and poor bone healing. In all cases, there is a risk that the screw may loosen and back out. Because the fixation is largely anterior, there may be inadequate posterior stability.
Hybrid maxillomandibular fixation
In an attempt to combine the strength and rigidity of arch bars with the safety and efficiency of MMF screws, a hybrid arch bar has recently been produced. The manufacturer claims that this combination omits the need for interdental wiring, and thereby, reduces the chance of wire stick injuries for health care providers. It also is supposed to save time in application and removal and does not require an additional trip to the operating room for removal. This new technology has not yet undergone controlled trials or studies on the long-term effects, but is a promising new technique in MMF.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree