Revision rhinoplasty is a complex operation with many variables that may influence the final esthetic and functional outcome of the procedure. Cartilage forms the structural framework of the lower two-thirds of nose and is essential for long-term support and maintenance of a patent nasal airway. The use of autologous cartilage grafting is the primary source of this material, limited by donor site quantity, quality, and harvest morbidity. Alloplastic materials, solid and injectable, are often used for augmentation purposes and may have devastating consequences. This article discusses past and current treatment concepts for various nasal deformities using available autologous grafting techniques.
Key points
- •
Revision rhinoplasty must improve nasal esthetic appearance and airway patency for complete patient satisfaction.
- •
Key grafts for improving the nasal airway include spreader graft, lateral crural strut graft, and alar batten graft.
- •
Infection prevention in rhinoplasty should include topical, systemic, or combination therapy, with or without drain management during revision surgery.
- •
Pros and cons exist regarding potential pitfalls of diced cartilage versus solid cartilage grafting.
- •
Alloplastic versus autogenous grafting during revision rhinoplasty includes Augmentation of the nasal dorsum.
Introduction
Surgical rhinoplasty requires manipulation of the structural framework of the nose to elicit desired changes in contour. This procedure is exceedingly complex, especially for the revision rhinoplasty surgeon, because the esthetic outcome desired by the patient may reduce the nasal airway, leading to obstructive symptoms. Multiple variables affect the ultimate outcome, including nasal bone length, strength and resiliency of the upper and lower lateral cartilages, position and shape of the nasal septum, inferior turbinate hypertrophy, and the thickness of the overlying soft tissue envelope.
Over the past 60 years, the approach to revision rhinoplasty has expanded from a primarily reductive procedure, focusing purely on cosmetic outcome, to one that augments the structural components of the nasal skeleton. This evolving method has the ultimate goal of providing improvement in both the nasal airway and the nasal esthetics. Rhinoplasty surgeons seek to refine the techniques and methods that provide the most consistent and long-lasting outcomes. As the structural approach to rhinoplasty evolves, controversies emerge as continuing research applies the scientific method to new technology, surgical maneuvers, and long-term follow-up of surgical outcomes.
Introduction
Surgical rhinoplasty requires manipulation of the structural framework of the nose to elicit desired changes in contour. This procedure is exceedingly complex, especially for the revision rhinoplasty surgeon, because the esthetic outcome desired by the patient may reduce the nasal airway, leading to obstructive symptoms. Multiple variables affect the ultimate outcome, including nasal bone length, strength and resiliency of the upper and lower lateral cartilages, position and shape of the nasal septum, inferior turbinate hypertrophy, and the thickness of the overlying soft tissue envelope.
Over the past 60 years, the approach to revision rhinoplasty has expanded from a primarily reductive procedure, focusing purely on cosmetic outcome, to one that augments the structural components of the nasal skeleton. This evolving method has the ultimate goal of providing improvement in both the nasal airway and the nasal esthetics. Rhinoplasty surgeons seek to refine the techniques and methods that provide the most consistent and long-lasting outcomes. As the structural approach to rhinoplasty evolves, controversies emerge as continuing research applies the scientific method to new technology, surgical maneuvers, and long-term follow-up of surgical outcomes.
Controversies in rhinoplasty
Alloplastic Material versus Autologous Grafts in Dorsal Augmentation
Revision rhinoplasty frequently involves correction of iatrogenic nasal deformities, often the result of overresection of the existing nasal cartilaginous skeleton. Surgical correction requires augmentation with material similar to the natural nasal cartilage. The ideal graft material should be sufficient in quantity, strength, resiliency, and ability to be carved. It should be easily removed and unlikely to warp, migrate, become immunogenic, cause infection, or resorb. The source of this ideal graft remains elusive.
Alloplastic implants are an alternative to autologous grafting. The most popular products currently in use include silicone, porous polyethylene (Medpor, Stryker Inc., Kalamazoo, MI), polytetrafluoroethylene (Proplast, Vitek Inc., Houston, TX), and expanded polytetrafluoroethylene (Gore-Tex, W. L. Gore & Associates Inc, Flagstaff, AZ). The goal of such implants is primarily to address autologous grafting drawbacks related to increased operative time and donor site morbidity. However, alloplastic implants are associated with a unique set of potentially devastating consequences, including infection, rejection, and extrusion.
Silicone and polytetrafluorethylene (Proplast) implants are currently banned by the US Food and Drug Administration (FDA) but continue to be used almost exclusively in Asian augmentation rhinoplasty. Silicone may be produced to almost any consistency (soft to firm), has excellent elastic properties, can be carved, is easily placed, and is also easily removed due to capsule formation in vivo. Significant drawbacks include a reported extrusion/rejection rate of 8% at 160 days. Long-term studies suggest that rates of extrusion also increase with time and are a lifelong risk. The results of extrusion can be severe, including soft tissue loss and scarring of the nasal tip, which make correction to a preoperative state extremely difficult.
Expanded polytetrafluoroethylene (Gore-Tex) is composed of small pores approximately one/tenth the size of porous polyethylene and permits vascular ingrowth. A 3-year large case series (n = 1054) in Southeastern Asian primary rhinoplasty patients reported implant deviation in 1%, visible implant in 0.5%, and infection in 0.4%. However, long-term follow-up is lacking, and recent meta-analysis suggests a 10.6% infection rate with preceding fistula development.
Porous polyethylene (Medpor) has been used for reconstruction of many areas of the head and neck, including orbital fractures, chin and malar bone augmentation, as well as soft tissue augmentation during rhinoplasty and microtia repair. Characteristics include a flexible framework at body temperature, a pore size that permits rapid ingrowth of vascularized tissue, and thermoplastic properties when heated to greater than 85 ° C. Long-term follow-up has generally been lacking, but recent meta-analysis suggests that the use of Medpor and Gore-Tex implants has a 3.1% removal rate when used for nasal reconstruction, approximately half that of silicone (6.5%). Further reports have contended that Medpor is a suitable material for nasal spreader grafts.
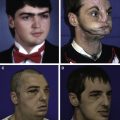
Drawbacks include difficulty in removal secondary to vascular ingrowth and infection. When Medpor was compared with auricular cartilage spreader grafts in a small case series, of 10 and 8 patients, respectively, 1 case of unilateral infection occurred in the Medpor group (10%). In another study comparing alloplastic to autogenous grafts, the highest infection rate was 23.4% when Medpor was used as a columellar strut graft. The overall autologous versus alloplastic infection rate in recent analysis was 0% versus 12.6%. Use of Medpor in the moveable portions of the nose (lower two-thirds) is fraught with higher infection and extrusion rates because the implant can erode through mucosa or skin. In addition, the Medpor dorsal shell implant is large and very difficult to remove ( Fig. 1 ). Once implanted, the skin on the nose is permanently altered and scarred.
Techniques are in development to minimize the risk of infection with alloplastic materials. There is short-term evidence demonstrating increased biocompatibility of synthetic implants is possible with platelet concentrate. The long-term effects of this therapy are unknown.
The current gold standard as well as the majority opinion of many top revision rhinoplasty surgeons favors the use of autologous grafts from the septum, auricle, or costal cartilage for dorsal augmentation. The often cited drawbacks to these sources include increased operative time, donor site morbidity, and inability to predict postoperative graft resorption and warping. However, with experience, graft harvest operative time decreases, nontraumatic technique minimizes donor site morbidity, and experience with carving the cartilage and selecting grafts helps minimize the chances of warping. Most surgeons agree that although alloplastic implants have a role in rhinoplasty, the risk of infection and extrusion must be equal to autologous tissue, with known long-term results, before they are implemented as a true replacement for autologous cartilage grafting.
Autologous Rib Versus Irradiated Rib for Nasal Reconstruction
The use of irradiated rib has been advocated as an alternative to alloplastic implants and homologous cartilage harvest. The benefits include an ample source of ideal material, replacing like tissue with like tissue, and the absence of donor site morbidity. This process is achieved by applying gamma radiation to cadaver rib, making the final product free of immunogenic and infectious potential. Use of irradiated rib for secondary rhinoplasty has been a source of controversy since its introduction, primarily due to physician concerns of graft resorption, the possibility of rejection by the host, and placement of a nonviable implant that does not become “living tissue.” Patient acceptance of a cadaveric donor tissue requires comprehensive consent and education. In addition, universal availability of the graft material may be limited by location and local regulation of donor tissues.
One 15-year retrospective study, published in 1998, concluded that irradiated rib had a high rate of resorption and should be anticipated by those using the material. This report has been contradicted by more recent studies with similar long-term follow-up. Adverse events in this study, from irradiated rib, were reported to be no greater than rhinoplasty complication rates when autologous costal grafts are used. The investigators ultimately concluded that the safety, reliability, and convenience of irradiated grafts are ideal for both primary and revision rhinoplasty.
Proponents of autologous costal cartilage grafts minimize the morbidity of graft harvest and report low risk of infection, extrusion, resorption, and warping. Autologous cartilage also becomes revascularized and can resist infection and resorption to a greater degree than irradiated grafts. Recent meta-analysis found the combined complication rates for autologous costal cartilage grafting were 3.08% (95% confidence interval [CI], 0%–10.15%) for warping, 0.22% (95% CI, 0%–1.25%) for resorption, 0.56% (95% CI, 0%–2.61%) for infection, 0.39% (95% CI, 0%-1.97%) for displacement, 5.45% (95% CI, 0.68%–13.24%) for hypertrophic chest scarring, 0% (95% CI, 0%–0.32%) for pneumothorax, and 14.07% (95% CI, 6.19%–24.20%) for revision surgery. Expert opinion maintains that warping can be controlled through careful selection of cartilage grafts, allowing sufficient time postharvest to witness the tendency of the cartilage to bend, and rigid fixation of the dorsal graft to the bony dorsum. Rigid fixation can be achieved via a perichondrial-bony interface and tight subperiosteal pocket placement ( Fig. 2 ).
In a study investigating the effects of carving plane, harvest level, and oppositional suturing techniques on autogenous cartilage warping, the methods used failed to demonstrate statistically significant results for the prevention of warping. However, the study concluded that a balanced approach, with central harvest of the rib, continues to be the most efficacious method for warping prevention because the process was found to continue up to 1 month after implantation and likely continues over time.
The ideal rib for cartilage grafting should have a primarily straight cartilaginous section of ample quantity and quality, be located away from the pleural cavity, and be harvested with minimal donor site morbidity. Based on anatomic study, the seventh rib fits these qualifications and seems to be the most ideal source in most individuals.
Novel application of available endoscopic technology has suggested that hypertrophic scarring of the chest wall associated with rib graft harvest may be eliminated via use of a transumbilical approach to the lower anterior chest wall. Proponents report an associated learning curve and increased operative time for this procedure, averaging 2 to 2.5 hours.
Based on current surgical techniques and available supporting research, autologous costal cartilage seems to be the best available material for complete nasal reconstruction during revision rhinoplasty cases compared with irradiated rib. More studies are required, with long-term follow-up, before universal acceptance of graft equality. Warping and donor site morbidity, including hypertrophic scarring, are the greatest statistical risks of the autologous harvest procedure and seem to be manageable complications with similar revision rates as those reported for primary rhinoplasty cases.
Diced Cartilage Versus Solid Cartilage Grafting
Diced cartilage dorsal augmentation grafts have been increasingly advocated as an adjunct or alternative to solid cartilage grafting over the past 20 years. The principle is to create a graft that is easy to place and mold, is not prone to warping or resorption, and will not become visible or palpable after tissue edema has subsided, especially in thin-skinned patients. Initially called a “Turkish delight,” this graft was composed of Surgicel (oxidized cellulose)-wrapped diced cartilage (0.5–1-mm cubes), sourced from autogenous septum, auricle, or rib. These rolled sleeves were used as dorsal augmentation and dorsal camouflage that were pliable and moldable via finger manipulation. Long-lasting results with few complications, including infection, resorption, or persistent overcorrection, was documented in 2365 patients over 10 years, including revision and primary rhinoplasty patients. Further investigation has failed to demonstrate long-term viability with Surgicel-wrapped grafts compared with grafts wrapped in autologous temporalis fascia, noting that as the Surgicel absorbs, unwanted contour irregularities may form. A rabbit model study replaced Surgicel with Alloderm (acellular dermis) and compared this material versus autologous fascia as a wrap for diced cartilage grafts. The investigators reported equivocal results on histology but cautioned that long-term studies are needed. Autologous tissue glue has also been reported to provide a stable scaffold for diced cartilage grafts with good results in 68 patients at 15 months follow-up.
Diced cartilage wrapped in autologous fascia may prove to be a reliable method of dorsal augmentation, but further long-term follow-up studies are needed to prove graft stability beyond 10 years. At this time, solid cartilage grafting has the advantage of documented long-term stability, structural integrity, and minimal complications with resorption or warping when treated appropriately. Solid cartilage grafting has the additional benefit of in-office needle shaving using local anesthesia if slight dorsal irregularities develop in the postoperative period. An 18-gauge needle provides a simple solution as solid grafts are firm but remain amenable to carving. Diced cartilage or alloplastic implants do not enjoy the same characteristics and instead must rely on revision surgery or injectable filler to achieve comparable results.
Injectable Cartilage Grafting
Dorsal augmentation with diced cartilage wrapped in fascia or other material requires surgical implantation via an endonasal or open approach with the possibility of postoperative dorsal irregularities due to absorption. Some surgeons think one alternative to diced cartilage is to use available septal, auricular, or costal cartilage to create an injectable cartilage slurry with high chondrocyte viability; this provides the ability to inject cartilage to fill small areas of irregularity while using solid cartilage grafting for structural support. This material should have the fine-tuning characteristics of synthetic injectables but the biocompatibility of autologous cartilage. Tissue engineering is currently lacking the technological advancements necessary to produce this material ex vivo using cell culture. Therefore, alternative methods using autologous cartilage sources have been under investigation.
Results from one study reported an otologic burr as the best instrument for creating uniform (largest dimension 0.44 ± 0.33 mm) cartilage pieces small enough for injection with an 18-gauge needle. Nasal septal cartilage produced the best results with 33% of lacunae containing viable-appearing chondrocytes. Drilled auricular cartilage produced similar size pieces, but only 10% of lacunae were occupied by viable chondrocytes. Other techniques tested (knife, morselizer, and cartilage crusher) did not produce pieces suitable as an injectable cartilage slurry. Additional research has recently been published describing a cartilage shaving technique by hand that produced an injectable cartilage slurry capable of injection through 14- or 18-gauge needles. This material was used to fill all areas of the nose in 128 patients over a 6-year period without a single case of infection, extrusion, displacement, or soft tissue irregularity. However, resorption occurred in almost all patients to some extent, leading to a 5% surgical revision rate.
This area continues to be an area of ongoing research and may have a place in the surgical armamentarium of rhinoplasty surgeons. At this time, long-term follow-up of surgical outcomes is required before wide acceptance as a viable alternative to solid cartilage, diced cartilage, or nasal filler.
Injectables in the Nose
Use of injectable facial fillers, primarily hyaluronic acid and calcium hydroxylapatite (Radiesse), has been used off label to perform “liquid,” “nonsurgical,” or “injection” rhinoplasty for many years. Although not FDA approved for this location, there are distinct advantages to the use of nonpermanent filler for alleviation of minor cosmetic defects, including minimal pain, avoidance of general anesthesia, short procedure time, quick recovery time, and reversibility with use of hyaluronic acid–based filler. Serious complications are uncommon, but catastrophic vascular compromise can occur via either direct injection of filler into end arterioles or vessel compression, leading to tissue ischemia and skin necrosis.
Short-term prospective studies by rhinoplasty surgeons have reported the use of facial filler, primarily Radiesse, for correction of postoperative deformities with good results and minimal complications that last for at least 1 year. Radiesse has gained increasing favor as the filler of choice for minor nasal augmentation because of its long duration, moldability, high viscosity, elasticity, and low immunogenicity (no allergy testing required). Noted drawbacks with hyaluronic acid intradermal nasal injection include migration and the Tyndall effect, creating a bluish tint in bright light, especially in thin skin.
Liquid silicone was the first off-label permanent filler to be used extensively as an adjunct to rhinoplasty. However, it lost favor in use because of potential long-term issues with chronic inflammation. A recent study using polymethyl methacrylate, used in 19 subjects followed for 1 year, demonstrated good cosmetic results with no serious adverse events other than palpable, but not visible, nodule formation. The product uses bovine collagen as a carrier with a potential risk for allergic reaction or rejection and requires intradermal testing before use. An issue with all permanent injectables includes need for surgical removal, if required, and potential for increased surgical complexity with revision rhinoplasty.
Use of facial filler for primary rhinoplasty or as an adjunct to postoperative irregularity is avoided by the senior author (D.M.T.). Reasons for avoidance are primarily related to the potential for vascular injury to the skin envelope of the nose. Furthermore, most patients present for rhinoplasty with airway complaints and seek improvement in nasal airflow; this requires structural support that injection rhinoplasty cannot provide. Although it is probably a safe practice to inject the nasal dorsum, injection of the nasal tip should be avoided. Nasal tip blood supply is primarily end arterioles, and major reconstruction will be required if intravascular application or local compression leads to tissue necrosis.
Spreader Flap Versus Spreader Grafts
Most reductive rhinoplasty procedures involve the removal of a dorsal hump, consisting of the caudal aspect of the nasal bones as well as the cephalic aspect of the upper lateral cartilages and superior septal cartilage. If a significantly sized hump is removed, generally more than 2 mm, an open roof deformity is created whereby the upper lateral cartilages and septum were resected. Spreader grafts are the traditional solution to addressing the middle vault region but require additional cartilage material that may or may not be available following septoplasty, especially if the procedure is a revision rhinoplasty. The autospreader or spreader flap has been proposed in several case series as a method that makes use of existing upper lateral cartilage during dorsal hump reduction. Proponents advocate this technique as consistently reproducible for preservation of the dorsal esthetic line by keeping the upper lateral intact and scoring the cartilage to allow medial infolding of the upper lateral cartilages onto themselves. The spreader flap is then sutured to the dorsal septum, closing the open roof and simultaneously improving the airway at the internal nasal valve.
Controversy with this method exists because of conflicting evidence that the autospreader technique is truly equivalent to traditional spreader grafts carved from septal or costal cartilage. A recent small study demonstrated significant improvement in nasal obstruction symptom evaluation (NOSE) scale and visual analogue scores with the autospreader technique at less than 6 months of follow-up. Another study found no statistical difference in minimal cross-sectional area or by visual analogue scale for esthetic appearance or nasal obstruction at 1-year follow-up when the autospreader technique was used.
A reported drawback of the autospreader technique is inability to address width in the lower third of the nasal dorsum and supratip region. In addition, with smaller dorsal hump reductions, there will be minimal upper lateral cartilage to fold over to create the spreader flap. In another case series, the combination of the autospreader technique was combined with small spreader grafts to increase dorsal width from 5 mm (autospreader only) to 7 mm (combination autospreader/spreader).
Autospreader or spreader flaps have a role in reduction rhinoplasty, especially with removal of large dorsal humps. At this time, long-term follow-up of this technique is insufficient to recommend their use exclusively over traditional spreader grafting, especially for revision surgery cases. A more prudent approach is combination grafting to achieve a smooth dorsal esthetic line while ensuring that the internal nasal valve remains uncompromised.
Onlay Grafting to Existing Structure Versus Complete Reconstruction
Many surgeons that perform revision rhinoplasty add cartilage to the existing deformed nasal structure to add support and improve contour. This method frequently involves use of alar batten grafts, shield tip grafts, and onlay grafts to the nasal tip. This method can be very effective but does add additional bulk to the structure of the nose and can create extra thickness ( Fig. 3 ).